ABSTRACT
Purpose
To identify whether long-term symptom relief and stent patency vary with the use of covered versus uncovered stents for the treatment of benign SVC obstruction.
Methods and Materials
We retrospectively identified all patients with benign SVC syndrome treated to stent placement between January 2003 and December 2015 (n = 59). Only cases with both clinical and imaging follow-up were included (n = 47). In 33 (70%) of the patients, the obstruction was due to a central line or pacemaker wires, and in 14 (30%), the cause was fibrosing mediastinitis. Covered stents were placed in 17 (36%) of the patients, and 30 (64%) patients had an uncovered stent. Clinical and treatment outcomes, complications, and the percent stenosis of each stent were evaluated.
Results
Technical success was achieved in all cases at first attempt. Average clinical and imaging follow-up in years was 2.7 (range 0.1–11.1) (covered) and 1.7 (range 0.2–10.5) (uncovered), respectively. There was a significant difference (p = 0.044) in the number of patients who reported a return of symptoms between the covered (5/17 or 29.4%) and uncovered (18/30 or 60%) groups. There was also a significant difference (p = < 0.001) in the mean percent stenosis after stent placement between the covered [17.9% (range 0–100) ± 26.2] and uncovered [48.3% (range 6.8–100) ± 33.5] groups. No significant difference (p = 0.227) was found in the time (days) between the date of the procedure and the date of clinical follow-up where a return of symptoms was reported [covered: 426.6 (range 28–1554) ± 633.9 and uncovered 778.1 (range 23–3851) ± 1066.8]. One patient in the uncovered group had non-endovascular surgical intervention (innominate to right atrial bypass), while none in the covered group required surgical intervention. One major complication (SIR grade C) occurred that consisted of a pericardial hemorrhagic effusion after angioplasty that required covered stent placement. There were no procedure-related deaths.
Conclusion
Both covered and uncovered stents can be used for treating benign SVC syndrome. Covered stents, however, may be a more effective option at providing symptom relief and maintaining stent patency if validated by further studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Superior vena cava (SVC) syndrome is caused by obstruction of the venous blood flow from the upper part of the body through the SVC to the heart. Although most cases are due to malignancy [1], benign (non-malignant) causes can also cause SVC syndrome. The primary benign causes are fibrosing mediastinitis and indwelling central venous catheters/intravascular implanted cardiac devices [2]. Although benign causes of SVC syndrome tend to not be life threatening, associated symptoms such as facial swelling, upper limb edema, and headache are a significant burden to affected patients [3].
Treatments of benign SVC syndrome include surgical bypass, angioplasty and/or angioplasty with stent placement. Due to being minimally invasive, angioplasty and stent placement are now first-line treatments, having replaced surgical management for SVC syndrome [4, 5]. A range of stent types is available which can be grouped into covered and uncovered stents [6]. There is no current consensus as to whether covered or uncovered stents provide better treatment outcomes. This study aimed to identify whether symptom relief and stent patency vary with the use of covered versus uncovered stents for the treatment of benign SVC syndrome.
Methods and Materials
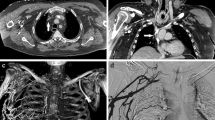
This retrospective review was approved by the institutional review board. All patients treated with stent for benign SVC syndrome between January 1, 2003 and December 31, 2015, were identified using an institutional database (n = 59). Benign SVC syndrome was defined as any patient with signs (swelling of the neck, face, or upper extremity, dilation of neck veins, etc.) and symptoms (headache, shortness of breath, and visual changes) due to non-malignant blockage of blood flow through the superior vena cava into the right atrium [7]. Only cases with both post-procedural clinical and imaging follow-up were included (n = 47). Adequate post-procedural clinical follow-up required follow-up with either the Divisions of Vascular and Interventional Radiology or Vascular Surgery. Adequate post-procedural imaging follow-up was defined as an SVC digital subtraction venogram (n = 23) or a contrast-enhanced CT venogram of the chest (n = 24).
All patients were jointly evaluated, triaged, and managed through the Divisions of Vascular and Interventional Radiology and Vascular Surgery. Patients were referred to these departments for treatment of benign SVC syndrome if they met symptom criteria for SVC syndrome as outlined by Kishi et al. [1]. Signs and symptoms reported by the patients in this study included headache, visual changes, face and neck swelling, upper limb edema, and respiratory difficulty. Patients additionally had a CT Chest with iodinated contrast demonstrating narrowing of the superior vena cava. The classification of obstruction was based on venographic criteria by Stanford and Doty [8]. Briefly, 23 (49%) patients had a type I obstruction, 9 (19%) had a type II, 10 (21%) had type III, and 5 (11%) had type IV.
Access was gained from the right internal jugular vein, basilic/brachial veins, or right common femoral vein. Access was based on pre-procedure evaluation with ultrasound for patency. Local or general anesthesia was used for sedation. After placement of a 6–12 French introducer sheath, diagnostic venogram was obtained through an angiographic catheter. If venography demonstrated a stenosis, 5000 UI of heparin was administered and recanalization was performed with hydrophilic guidewires. Pressure measurements were then obtained from the right atrium to peripheral of the obstruction based on operator preference (obtained in 20 out of 47 cases). Angioplasty was subsequently performed with 8-mm or 10-mm balloons. If post-angioplasty venography demonstrated residual stenosis or continued flow through collateral circulation, stenting was performed. Stent diameter was in the range of 14 mm with a minimum of 10 mm and a maximum of 20 mm. The length was selected so that the underlying obstruction would be covered by the stent. The selection of a covered or uncovered stent was made by the operator at the time of the procedure primarily based on operator preference and comfort with some authors placing only covered stents while others placing only non-covered stents. The uncovered stents included Wallstents (Boston Scientific-Marlborough, MA), Protégé (Covidien-Dublin, Ireland), and SMART (Cordis-Milpitas, CA) stents. Covered stents used included Gore Viabahn (Gore-Newark, DE) and iCast (Atrium-Dallas, TX) stents. If needed, balloon angioplasty was used for stent remodeling. Technical success was defined as re-establishment of patency of the SVC and lack of collateral flow. Clinical success was defined as an alleviation of symptoms or a Kishi score < 4 by the time of hospital discharge [1].
All patients were eventually re-evaluated by the Divisions of Vascular and Interventional Radiology and Vascular Surgery in accordance with planned 3-month, 6-month, and yearly outpatient follow-up. Patients with a subjective return of the above-listed symptoms were evaluated urgently. Follow-up was also obtained at the request of referring physicians. At follow-up, if evaluation of stent patency was required whether due to a return of symptoms or more than a year had passed without radiographic follow-up, imaging was obtained which consisted of a SVC digital subtraction venogram or a contrast-enhanced CT venogram of the chest. Subsequent re-treatment was based on clinical and imaging findings. Clinical findings included a return of symptoms as detailed above and/or Kishi score > 4. Imaging findings included greater than 50% stenosis diameter and return of flow through collaterals.
Recorded clinical features included demographics, clinical and procedural outcomes, complications, and percent in-stent stenosis. Percent in-stent stenosis was calculated by dividing the smallest diameter in the stenotic segment by the diameter of the adjacent normal segment of the stent and multiplying by 100. Complications were defined using the Society of Interventional Radiology standards [9]. The following definitions were used: primary patency was defined as a stent with uninterrupted patency with no procedure performed on the stent itself; primary-assisted patency was defined as a stent where patency was never lost, but intervention was performed in order to maintain patency; and secondary patency was identified as a stent where endovascular intervention was required to restore patency.
Of the 47 patients that met the inclusion criteria, 29 (62%) were female and 18 (38%) were male. Average age was 47 (range 24–74 years). Thirty-three patients (70%) had SVC obstruction caused by a chronic indwelling central line and/or pacemaker wires, and 14 (30%) were caused by fibrosing mediastinitis. In 17 (36%) patients, a covered stent was placed, and 30 (64%) patients had an uncovered stent placed. Twenty-nine (62%) had prior intervention for their symptoms whether it consisted of anticoagulation and thrombolysis or an intervention at an outside institution that consisted of angioplasty. Cases with prior stenting of the SVC were not included in the study (n = 4). Anticoagulation was continued by resuming Coumadin or weight-based lovenox in 36 (77%) of the patients after stent placement, while the remaining 11 (33%) did not continue anticoagulation. Of note, based on pre-procedural discussions with the Departments of Cardiology and Nephrology and the patients’ primary provider, the chronic indwelling central line and/or pacemaker wires were removed during the procedure in 17 out of 33 patients whose symptoms were due to a chronic line. Table 1 further details patient demographics based on covered and uncovered stent groups.
Baseline patient characteristics and outcomes of interest were compared between stent groups by either Chi-squared or Fisher’s exact test for categorical variables depending on cell size and by t test or Wilcoxon rank sum test for continuous variables depending on normality. Time to loss of primary patency was shown graphically between stent types using a Kaplan–Meier curve and compared by log-rank test. All statistical analyses were conducted using Rstudio version 3.2.3.
Results
Technical success was achieved in all cases. The average pressure difference from the right atrium to peripheral to the obstruction was a decrease of 13.3 mmHg with a range of 2 mmHg to 28 mmHg. Average clinical and imaging follow-up in years was 2.7 (range 0.1–11.1) (covered) and 1.7 (range 0.1–10.5) (uncovered), respectively. There was a significant difference (p = 0.044) in the number of patients who reported a return of the above-listed symptoms at clinical follow-up between the covered (5/17 or 29.4%) and uncovered (18/30 or 60%) groups. There was also a significant difference (p < 0.001) in the mean percent stenosis of the stents between the covered [17.9% (range 0–100) ± 26.2] and uncovered [48.3% (range 6.8–100) ± 33.5] groups. Three out of 5 patients in the covered group and 15 out of 18 in the uncovered group that reported a return of symptoms went on to further intervention to maintain patency. No significant difference (p = 0.227) was found in the time (days) between the date of the procedure and the date of clinical follow-up where a return of symptoms was reported [covered 426.6 (range 28–1554) ± 633.9 and uncovered 778.1 (range 23–3851) ± 1066.8]. These results are also covered in Table 2.
Table 3 further details patency data for the two groups. Figure 1 provides a Kaplan–Meier curve comparing the time to loss of primary patency between the two groups (p = 0.877). Although this trend reversed at about 1 year, early on the uncovered group had better primary patency, most likely due to chance from low numbers. Graphical analysis of primary-assisted and secondary patency rates could additionally not be provided given the low numbers. No significant difference (p = 0.604) was seen in the mean percent stenosis between benign SVC syndrome due to a chronic indwelling central line and/or pacemaker wires or fibrosing mediastinitis [chronic central or pacemaker line 35.3 (range 1.7–100) ± 35.7 and fibrosing mediastinitis 41.0 (range 13–100) ± 29.1].
Of significant note, one patient in the uncovered group required non-endovascular surgical intervention. This patient 10 months later had a return of previously reported symptoms of headaches and facial and upper extremity swelling with a 90% stenosis that was retreated with angioplasty and thrombolytic therapy. This patient returned 5 months later with headaches and facial and upper extremity swelling with complete stent occlusion and was then treated with an innominate to right atrial surgical bypass.
Finally, one major complication (SIR grade C) occurred. This consisted of a pericardial hemorrhagic effusion that was noticed after angioplasty with a 16 × 40 mm balloon. A covered stent was placed following placement of a pericardial drain. In this case, the intent had been to see whether angioplasty by itself would suffice, but due to the pericardial rupture a covered stent was placed. The patient remained hemodynamically stable following intervention and by discharge had a resolution of the presenting SVC syndrome-related symptoms. There were no procedure-related deaths.
Discussion
This study demonstrates that stenting of benign SVC syndrome is safe and effective. The results also indicate that a covered stent could be a better option for treatment of benign superior vena cava obstruction. In prior studies, a range of stents were used. Few prior publications analyzed whether covered or uncovered stents are more effective for benign SVC syndrome [10, 11]. In the largest cohort to date in the endovascular treatment of benign SVC syndrome which included forty-four patients, Wallstents and nitinol-based stents were primarily used, but analysis of which type of stent was more effective was not performed [12]. Moreover, there has been sparse literature comparing covered versus uncovered stents in the venous system, while several studies looking at aortoiliac atherosclerotic disease have given conflicting outcomes, with two demonstrating better patency for covered stents [13, 14] while another shows that bare metal stents have better patency [15].
Similar to past endovascular studies of SVC syndrome [16,17,18], this study demonstrates good short- and mid-term patency rates with adequate long-term patency rates being demonstrated in patients with adequate follow-up which is also similar to surgical outcomes. However, as previously demonstrated in the literature for endovascular treatment, durable long-term relief of symptoms requires multiple secondary interventions which are not usually required with surgery [4, 19, 20]. In this study, 18 out of 47 cases went on to require a secondary intervention to maintain patency. Endovascular treatment’s minimal invasiveness, ability to use local or moderate sedation, shorter hospital stays, and lower complication rate nevertheless allow endovascular treatment to be the primary choice for SVC syndrome, while surgery remains a feasible option in patients who fail endovascular treatment or are not candidates for endovascular treatment [21,22,23]. One out of 47 cases required surgical intervention, which was in the uncovered group.
A single major complication was seen in this cohort. This low complication rate is similar to prior endovascular studies [4, 12, 24]. It highlights an advantage of covered stents in that although this complication happened before stent placement, a covered stent was placed to assist in the management of the pericardial hemorrhagic effusion. As primarily demonstrated in the cardiology literature, covered stents are an adequate choice for controlling venous perforation, which is a common complication after angioplasty of the SVC [25,26,27,28]. When choosing between a stent for SVC treatment, use of a covered stent for control of a perforation should be considered. Nevertheless, inflation of an angioplasty balloon should still be considered as a first and urgent maneuver in controlling the bleeding [29].
CT venography was used in both the pre- and post-treatment evaluation of patients in this study. Fifty-one percent of the patients did undergo a CT venogram of the chest which allowed for evaluation of stent patency. CT venography offers a noninvasive method for diagnosis and post-treatment evaluation of SVC syndrome when compared to digital subtraction venography. Catheter-based venography, despite its invasiveness, allows for pressure measurement which can give added information to help with further treatment decisions [30] and use of intravascular ultrasound. Assessment of veins peripheral to the SVC obstruction and overall thrombotic burden may even be superior with CT compared to digital subtraction venography [31]. CT venography is also an appealing option in circumstances where patients are symptomatic, but stent obstruction is clinically doubtful as it can be easily obtained and can prevent an unnecessary procedure. Although not used in this study, MR venography is an additional option in patients with contraindications to iodinated contrast and it does not require radiation. The metal in the stents does give small artifacts which may limit the usefulness of MRV for follow-up of SVC stents [32].
A significant limitation of the current study is its retrospective nature, similar to prior publications [4, 12]. Due to the rare occurrence of benign SVC syndrome, which is less common than malignant SVC syndrome [33], a prospective trial is not feasible. As a tertiary care center, it is also difficult to completely track return of symptoms and delayed complications as many patients receive routine care at their local health care facility and such symptoms might not be reported. For similar circumstances, patients may have changes in management, such as the continuation or discontinuation of anticoagulation, due to local management. This furthermore limits long-term follow-up as most patients prefer to continue their management close to home. There was also a significant gender difference among the groups with only three males in the covered stent group. Finally, there was no uniformity for choosing between stent types as this depended on operator preference, as with multiple operators within the Division of Vascular and Interventional Radiology and Division of Vascular Surgery placing stents for SVC syndrome.
Conclusion
Both covered and uncovered stents can be used for treating benign SVC syndrome. Covered stents in this study appeared more effective at providing symptom relief and maintaining stent patency. Therefore, covered stents could offer a more appealing option for treatment of benign SVC syndrome if validated by further studies.
Abbreviations
- SVC:
-
Superior vena cava
- SIR:
-
Society of Interventional Radiology
References
Kishi K, Sonomura T, Mitsuzane K, et al. Self-expandable metallic stent therapy for superior vena-cava syndrome—clinical observations. Radiology. 1993;189:531–5.
Sheikh MA, Fernandez BB Jr, Gray BH, Graham LM, Carman TL. Endovascular stenting of nonmalignant superior vena cava syndrome. Catheter Cardiovasc Interv. 2005;65:405–11.
Rachapalli V, Boucher LM. Superior vena cava syndrome: role of the interventionalist. Can Assoc Radiol J. 2014;65:168–76.
Rizvi AZ, Kalra M, Bjarnason H, Bower TC, Schleck C, Gloviczki P. Benign superior vena cava syndrome: stenting is now the first line of treatment. J Vasc Surg. 2008;47:372–80.
Warner P, Uberoi R. Superior vena cava stenting in the 21st century. Postgrad Med J. 2013;89:224–30.
Barshes NR, Annambhotla S, El Sayed HF, et al. Percutaneous stenting of superior vena cava syndrome: treatment outcome in patients with benign and malignant etiology. Vascular. 2007;15:314–21.
Cheng S. Superior vena cava syndrome: a contemporary review of a historic disease. Cardiol Rev. 2009;17:16–23.
Stanford W, Doty DB. The role of venography and surgery in the management of patients with superior vena cava obstruction. Ann Thorac Surg. 1986;41:158–63.
Sacks D, McClenny TE, Cardella JF, Lewis CA. Society of Interventional Radiology clinical practice guidelines. J Vasc Interv Radiol. 2003;14:S199–202.
Chee CE, Bjarnason H, Prasad A. Superior vena cava syndrome: an increasingly frequent complication of cardiac procedures. Nat Clin Pract Cardiovasc Med. 2007;4:226–30.
Smayra T, Otal P, Chabbert V, et al. Long-term results of endovascular stent placement in the superior caval venous system. Cardiovasc Intervent Radiol. 2001;24:388–94.
Breault S, Doenz F, Jouannic AM, Qanadli SD. Percutaneous endovascular management of chronic superior vena cava syndrome of benign causes: long-term follow-up. Eur Radiol. 2017;27:97–104.
Sabri SS, Choudhri A, Orgera G, et al. Outcomes of covered kissing stent placement compared with bare metal stent placement in the treatment of atherosclerotic occlusive disease at the aortic bifurcation. J Vasc Interv Radiol. 2010;21:995–1003.
Mwipatayi BP, Thomas S, Wong J, et al. A comparison of covered vs bare expandable stents for the treatment of aortoiliac occlusive disease. J Vasc Surg. 2011;54:1561–70.
Humphries MD, Armstrong E, Laird J, Paz J, Pevec W. Outcomes of covered versus bare-metal balloon-expandable stents for aortoiliac occlusive disease. J Vasc Surg. 2014;60:337–43.
de Jager CP, Rutten MJ, Lips DJ. “Benign” superior vena cava syndrome. Intensive Care Med. 2013;39:572–3.
Lanciego C, Rodriguez M, Rodriguez A, Carbonell MA, Garcia LG. Permanent pacemaker-induced superior vena cava syndrome: successful treatment by endovascular stent. Cardiovasc Intervent Radiol. 2003;26:576–9.
Qanadli SD, El Hajjam M, Mignon F, et al. Subacute and chronic benign superior vena cava obstructions: endovascular treatment with self-expanding metallic stents. Am J Roentgenol. 1999;173:159–64.
Rosenblum J, Leef J, Messersmith R, Tomiak M, Bech F. Intravascular stents in the management of acute superior vena cava obstruction of benign etiology. JPEN J Parenter Enteral Nutr. 1994;18:362–6.
Schindler N, Vogelzang RL. Superior vena cava syndrome. Experience with endovascular stents and surgical therapy. Surg Clin North Am. 1999;79:683–94.
Doty JR, Flores JH, Doty DB. Superior vena cava obstruction: bypass using spiral vein graft. Ann Thorac Surg. 1999;67:1111–6.
Kennedy DP, Palit TK. Reconstruction of superior vena cava syndrome due to benign disease using superficial femoral vein. Ann Vasc Surg. 2010;24(555):e7–12.
Kalra M, Gloviczki P, Andrews JC, et al. Open surgical and endovascular treatment of superior vena cava syndrome caused by nonmalignant disease. J Vasc Surg. 2003;38:215–23.
Lanciego C, Chacon JL, Julian A, et al. Stenting as first option for endovascular treatment of malignant superior vena cava syndrome. AJR Am J Roentgenol. 2001;177:585–93.
Al-Mukhaini M, Panduranga P, Sulaiman K, Riyami AA, Deeb M, Riyami MB. Coronary perforation and covered stents: an update and review. Heart Views. 2011;12:63–70.
Jamshidi P, Mahmoody K, Erne P. Covered stents: a review. Int J Cardiol. 2008;130:310–8.
Baruah DK. Covered stent to treat saphenous venous graft perforation—a case report. Catheter Cardiovasc Interv. 2010;76:844–6.
George S, Mamas M, Nolan J, Ratib K. Radial artery perforation treated with balloon tracking and guide catheter tamponade—a case series. Cardiovasc Revasc Med. 2016;17:480–6.
Kuhn J, Kilic A, Stein E. Management of Innominate Vein Rupture During Superior Vena Cava Angioplasty. A A Case Rep. 2016;7:89–92.
Qanadli SD, El Hajjam M, Bruckert F, et al. Helical CT phlebography of the superior vena cava: diagnosis and evaluation of venous obstruction. AJR Am J Roentgenol. 1999;172:1327–33.
Kim H, Chung JW, Park JH, et al. Role of CT venography in the diagnosis and treatment of benign thoracic central venous obstruction. Korean J Radiol. 2003;4:146–52.
Sonavane SK, Milner DM, Singh SP, Abdel Aal AK, Shahir KS, Chaturvedi A. Comprehensive imaging review of the superior vena cava. Radiographics. 2015;35:1873–92.
Wilson LD, Detterbeck FC, Yahalom J. Clinical practice. Superior vena cava syndrome with malignant causes. N Engl J Med. 2007;356:1862–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Benjamin Simmons: Contribution was funded in part by Grant R25 HL92621 from the National Institutes of Health. Sanjay Misra: NIH funding from HL098967 and DK 108780 and DSMB Chair for Flex Stent from Cordis J and J. The other authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Haddad, M.M., Simmons, B., McPhail, I.R. et al. Comparison of Covered Versus Uncovered Stents for Benign Superior Vena Cava (SVC) Obstruction. Cardiovasc Intervent Radiol 41, 712–717 (2018). https://doi.org/10.1007/s00270-018-1906-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-018-1906-3