Abstract
Purpose
To compare the coaxial and noncoaxial techniques of renal parenchymal core needle biopsy.
Materials and Methods
This is an institutional review board-approved randomised controlled trial comparing 83 patients (male, n = 49) who underwent renal parenchymal core biopsy with coaxial method and 83 patients (male, n = 40) with noncoaxial method. The rate of complications, the number of glomerular profiles, and the procedural time were evaluated in a comparison of the two methods. Correlation between the presence of renal parenchymal disease and the rate of complication was also evaluated.
Results
The procedural time was significantly shorter in the coaxial technique (coaxial group, 5 ± 1 min; noncoaxial group, 14 ± 2 min; p < 0.001). The rates of complications for the coaxial method was significantly lower than the noncoaxial method (coaxial group, 10.8 %; noncoaxial group, 24.1 %; p = 0.025). There was no significant correlation between gender and the rate of complication. The number of glomerular profiles was significantly higher in patents who underwent renal biopsy with the coaxial method (coaxial group, 18.2 ± 9.1; noncoaxial group, 8.6 ± 5.5; p < 0.001). In the whole study population, the rate of complications was significantly higher in patients with a pathologic renal parenchyma compared to those with a normal parenchyma (19/71 vs. 10/95; p = 0.006).
Conclusions
Renal parenchymal biopsy using a coaxial needle is a faster and safer method with a lower rate of complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Renal parenchymal core biopsy can be done either with coaxial or noncoaxial technique. In coaxial technique, the introducing needle is placed in the target organ; then, multiple tissue samples can be performed through the same tract. Alternatively, in noncoaxial technique, biopsy needle is inserted repeatedly for each tissue sampling [1]. There is only one report by Hatfield et al. [2] in the literature regarding the comparison of coaxial and noncoaxial methods of renal biopsy in their complication rate. However, their study had a recognised limitation, and different operators with different level of experience at image-guided biopsy had performed the renal biopsies in their investigation [2]. Nonetheless, the comparison of the two methods of renal biopsy in regard to the procedural time and the acquired glomerular profiles number has not yet been described to the best of our knowledge. Also, correlation between the presence of renal parenchymal disease and complication rate in regard to the biopsy method has not been studied to date. In this prospective study, the complication rate and procedural time of coaxial technique were compared with those of noncoaxial technique in percutaneous renal parenchymal biopsy. Also, correlation between the presence of renal parenchymal disease and the rate of complication was evaluated in each method.
Materials and Methods
Study Design
This study was a prospective parallel group, 1:1 randomised trial conducted in a single centre. Approved by the Institutional Review Board, this trial was compliant with Health Insurance Portability and Accountability Act regulations, and written informed consent was obtained from all enrolled patients. The protocol was registered on the ClinicalTrials.gov (NCT02758535) properly.
Participants
Patients with a suspicious renal parenchymal disease who were referred to the diagnostic and interventional radiology department for renal biopsy were considered for enrollment. Core biopsy is not indicated in end-stage renal disease patients with small-sized kidneys. So, patients with end-stage renal disease were excluded from the study. Since the focus of this study was on the core biopsy of renal parenchyma in native kidneys, those with transplant kidney, history of renal cell carcinoma or a suspicious renal mass except for a Bosniak category I or II cystic mass, if incidentally found in patients referring for the assessment of renal parenchymal disease, were also excluded. Abnormal coagulation parameters were corrected before the procedure, and those with an uncorrectable coagulopathy were excluded from the study. Acceptable activated partial thromboplastin time, international normalised ratio, and platelet count were <1.5 times of control, <1.5, and >50,000/mm3, respectively. The patients were asked to abstain from warfarin or aspirin for 5 days before the procedure. Unfractionated heparin was withheld 2–4 days before the biopsy, and short-, intermediate-, and long-acting nonsteroidal anti-inflammatory drugs were withheld 1, 2–3, and 10 days before the start of the procedure, respectively [3].
Biopsy
All biopsies were performed by a single operator with 5 years experience of interventional radiology under guidance of real-time sonography using an ultrasound machine (LOGIQ S6, GE healthcare, USA) with a 2–5 MHz curvilinear transducer (Fig. 1). The patients were randomised into two groups. One group underwent renal biopsy with a coaxial Tru-Cut needle (18-gauge semiautomatic biopsy system with a 17-gauge coaxial needle; TSK Laboratory, Tochigi, Japan), and the other group underwent renal biopsy with a noncoaxial needle (18-gauge semiautomatic biopsy system without coaxial needle; TSK Laboratory, Tochigi, Japan).
The patients were asked to lie in prone position. Local anaesthesia of the tract was administered before the procedure using 10 mL of lidocaine 2 %. In the coaxial group, the coaxial needle was advanced just to the outer cortex of the kidney, and the needle angle was adjusted so that the needle pathway was directed to the renal cortex. Then, 4 cores were obtained through the introducing needle. In the noncoaxial group, the biopsy needle was advanced just to the outer renal cortex without using an introducing needle, and after firing, the whole procedure was repeated for four times for adequate tissue sampling. A proper trajectory was chosen to avoid central hilum in both groups. In this study, all parenchymal biopsies were taken from the lower pole of left kidney.
Measurements
The time of procedure was recorded for each patient, and the mean time of procedure was compared between the two groups. After the procedure, limited images from the kidney were obtained on low-dose computed tomography to evaluate for any complications, and the scans were interpreted by another radiologist.
According to the Society of Interventional Radiology (SIR) standards of practice documents [4], major complications were defined as those that may result in minor (<48 h) or prolonged (>48 h) hospitalisation or induce permanent sequlae or death, and other complications were defined as minor ones. The overall rate of complications was compared between the two groups. Any correlation between the rate of complication and patient’s gender was sought in each group. The number of glomerular profiles and final pathological diagnosis were determined by a single pathologist. Finally, the number of glomerular profiles was compared between the two groups, and correlation between the presence of a renal parenchymal disease and rate of complications was determined for the whole study population and also in each group separately.
Sample Size, Randomisation, and Blinding
In the primary endpoint measures, the complication rates of 0.09 and 0.2 were detected in the coaxial and noncoaxial groups, respectively, and a total sample size of 161 patients was calculated to provide a power of 80 % (α = 0.05) in determining a significant difference of complication rate between the two groups. Patients were assigned to the coaxial and noncoaxial groups with the use of random permuted blocks stratified by centre. The radiologist who interpreted the computed tomography findings after the procedure and also the pathologist were blinded to the biopsy technique of the patients.
Statistical Analyses
All continuous data were expressed as mean ± standard deviation. Statistical analyses were made using SPSS software version 23.0 (IBM, Armonk, New York). Comparison of continuous and categorical variables was evaluated by employing unpaired Student t test and Pearson Chi square test, respectively. P values of <0.05 were considered to indicate a statistically significant difference.
Results
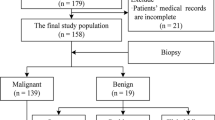
During a 12-month period beginning in March 2015, 215 patients were referred to the interventional radiology department for renal parenchymal biopsy. Among them, 9 patients with a history of renal cell carcinoma, 3 patients with end-stage renal disease, and 13 patients who refused to participate were excluded from the study. One hundred ninety patients were randomised in two groups, and 12 participants were lost to follow-up in each group. Finally, the target study population comprised 166 patients (male, n = 89; female, n = 77; mean age, 43 ± 16 years; range, 13–86 years), including 83 patients in the coaxial group (male, n = 49; female, n = 34; mean age, 45 ± 15 years; range, 13–75 years) who underwent parenchymal renal biopsy with the coaxial technique, and 83 patients (male, n = 40; female, n = 43; mean age, 42 ± 17 years; range, 13–86 years) who underwent parenchymal renal biopsy with the noncoaxial technique (Fig. 2). There was no significant difference in the gender or age of the coaxial and noncoaxial groups (p > 0.05). None of the patients was suffering from a systemic autoimmune diseases.
The mean time of the procedure in the whole study population was 10 ± 5 min. The procedural time was significantly shorter in the coaxial group (coaxial group, 5 ± 1 min; noncoaxial group, 14 ± 2 min; p < 0.001).
The rate of complications in each group is shown in Table 1. The most common complication in both groups was perinephric haematoma (coaxial group, 7.2 %; noncoaxial group, 15.7 %). The overall rate of complications for the coaxial method was significantly lower than the noncoaxial method (coaxial group, 10.8 %; noncoaxial group, 24.1 %; p = 0.025). No major complications occurred in patients according to the SIR standards of practice documents [4], and there was no significant correlation between gender and the rate of complication in each group (coaxial group, p = 0.82; noncoaxial group, p = 0.85).
Ultrasound-guided renal parenchymal biopsy resulted in satisfactory tissue sampling for histopathologic evaluation in all patients. The number of glomerular profiles was 18.2 ± 9.1 and 8.6 ± 5.5 in the coaxial and noncoaxial groups, respectively. The difference in the number of glomerular profiles between the two groups was statistically significant (p < 0.001).
Forty patients (48.2 %) in the coaxial group had a parenchymal disease with focal segmental glomerulosclerosis being the most common pathology (n = 13). In the noncoaxial group, 31 patients (37.3 %) had a parenchymal disease with diffuse proliferative glomerulonephritis being the most common pathology (n = 8).
In the whole study population, patients with a parenchymal disease showed a significantly higher rate of complications compared to those with a normal renal parenchyma (19/71 vs. 10/95; p = 0.006). In the coaxial group, complication occurred in 11 out of 31 patients with a parenchymal disease and in 9 out of 52 patients without a parenchymal disease. Although the complication rate was higher in patients with a parenchymal disease, the difference was not statistically significant in this group (p = 0.06). In the noncoaxial group, patients with a parenchymal disease also showed a significantly higher rate of complications compared to those with a normal renal parenchyma (8/40 vs. 1/43; p = 0.010).
Discussion
Percutaneous image-guided parenchymal renal biopsy has been used to detect the different pathologies of renal parenchyma, to define the degree of reversible changes, to provide the necessary information about the likelihood of treatment response in patients with renal failure, proteinuria, or haematuria, and to define when the medical treatment fails. Percutaneous core needle renal biopsy has been reported to have a higher diagnostic yield compared to fine-needle aspiration [5–7]. Using ultrasonography has the advantage of real-time observation of the site of the biopsy during the procedure and a relatively wider availability. On the other hand, computed tomography could be used as a guidance for renal biopsy to provide images with a higher resolution, but patients’ respiration may change the optimal site of biopsy, and there is also radiation exposure as a disadvantage [8–15]. Few published data are present in literature, to date, regarding the comparison of coaxial and noncoaxial techniques in renal biopsy [2]. In the current study, the performances of coaxial and noncoaxial methods in ultrasound-guided renal core biopsy were compared in terms of the procedure duration, complication rate, and the number of glomerular profiles.
In author’s experience, the coaxial method was shown to take less time than the noncoaxial method (p < 0.001). Considering that in coaxial method, the practitioner does not have to pass the introducing needle through the skin surface for each sampling, and the coaxial method had been anticipated to be faster than the noncoaxial method.
An average complication rate of 4–7 % has been documented in the literature for percutaneous renal biopsy [16]. However, despite the advent of new technologies to improve the safety and efficacy of percutaneous renal biopsy including the use of real-time ultrasonography or computed tomography, a complication rate of more than 30 % was also reported even in recent reports [17]. The reported complications after renal biopsy include bleeding complications, infection, pneumothorax, and adjacent organ injuries. Bleeding complications could be stratified as perinephric haematoma, subcapsular haematoma, and haematuria [18]. Consistent with previous investigations, perinephric haematoma was the most common complication in the patients [19].
In this study, percutaneous renal biopsy with the coaxial technique versus noncoaxial technique resulted in a significantly lower bleeding complications. Although, Hatfield et al. [2] reported no significant differences between coaxial and noncoaxial biopsy methods in complication rates, the results of their study could be biased by the fact that operators with different levels of experience, including radiology residents and fellows, senior radiologist, and nephrologists, had performed the renal biopsies. Furthermore, one of the advantages of the coaxial method is the ability to leave the cannula at the site of biopsy and injecting the occlusive materials, including natural clot, gelatin foam, glue, coils, or thrombin, during the withdrawal of the cannula [12]. Although our trial was not designed to plug the tract at the end of the coaxial technique, using an occlusive material may decrease the bleeding complication ratio even more in the coaxial method. Bleeding complications after renal biopsy had been reported to be significantly increased in female patients, biopsies from left kidney, dialysis patients, and those treated with 1-deamino-8-d-arginine vasopressin prior to biopsy to improve platelet dysfunction [20]. In a more recent study, Manno et al. [21] showed that a significant correlation exists between bleeding complications and three predictors, including gender, age, and baseline partial thromboplastin time. They found that other baseline chemistries and needle size have no significant predictive value for the bleeding complications after renal biopsy [21]. In contrast to the results of previous studies [20, 21], no significant correlation between gender and the rate of complication was found in the current study. The discordance of the overall rate of complications and the predictive value of demographic factors among the previous studies may be due to different techniques applied and the different methods of measurement.
Also, in the whole study population and the noncoaxial group, complication rate was significantly increased in the presence of a renal parenchymal disease. In the coaxial group, complications was also more likely in patients with a diseased renal parenchyma, but the correlation was not statistically significant with a p value of 0.06. Thus, the predictive value of renal parenchyma disease on the rate of complications after percutaneous renal biopsy could be better evaluated by more randomised controlled trials.
Although the size of biopsy needle for tissue sampling was the same in both groups (18-gauge), the number of glomerular profiles was significantly higher in the coaxial group for unknown reasons. As one would expect, the samples following the first sample may probably achieve less tissue in the coaxial technique. However, we did the following maneuvers to avoid the decreasing size of the cores in consecutive samplings in the coaxial method: (1) rotating the cutting needle to orient the needle gap into another direction (2) taking a sample from an intact area very close to the previous one either by adjusting the angle of coaxial stylet or by asking the patient to hold his breath in different moments of his/her respiratory cycles. Nonetheless, the biopsy procedure was successful in all patients as it yielded sufficient tissue to establish or rule out a pathologic diagnosis.
There is no baseline data in the literature about what technique is more prevalent among those who perform percutaneous renal biopsy. And, when it comes to the use of coaxial versus noncoaxial method at image-guided renal biopsy, it seems just to be a matter of practitioner’s preference especially since there is a trade-off between multiple skin punctures and using a larger outer introducing needle. However, the results of the current study do suggest a better performance for the coaxial method in terms of the safety and the duration compared to the noncoaxial method.
This study had some limitations. The level of pain experienced by the patients in each group, the size of perinephric or sabcapsular haematoma, and the grading of haematuria were not evaluated in this study. So, further investigations may be warranted considering the correlation between the biopsy technique and the mentioned variables. Also, the effect of body habitus and depth of the target from skin on the severity of complications was not evaluated in the current study.
In summary, the coaxial technique is a faster method for parenchymal renal biopsy, and in regard to complications, it had a significantly lower rate of bleeding complications and a higher rate of the acquired number of glomerular profiles compared with the noncoaxial technique.
References
Babaei Jandaghi A, Habibzadeh H, Falahatkar S, Heidarzadeh A, Pourghorban R. Transperineal prostate core needle biopsy: a comparison of coaxial versus noncoaxial method in a randomised trial. Cardiovasc Intervent Radiol. 2016. doi:10.1007/s00270-016-1437-8.
Hatfield MK, Beres RA, Sane SS, et al. Percutaneous imaging-guided solid organ core needle biopsy: coaxial versus noncoaxial method. AJR Am J Roentgenol. 2008;190(2):413–7.
Patel IJ, Davidson JC, Nikolic B, et al. Addendum of newer anticoagulants to the SIR consensus guideline. J Vasc Interv Radiol. 2013;24(5):641–5.
Gupta S, Wallace MJ, Cardella JF, et al. Quality improvement guidelines for percutaneous needle biopsy. J Vasc Interv Radiol. 2010;21(7):969–75.
Neuzillet Y, Lechevallier E, Andre M, Daniel L, Coulange C. Accuracy and clinical role of fine needle percutaneous biopsy with computed tomography guidance of small (less than 4.0 cm) renal masses. J Urol. 2004;171:1802–5.
Jaff A, Molinie V, Mellot F, Guth A, Lebret T, Scherrer A. Evaluation of imaging-guided fine-needle percutaneous biopsy of renal masses. Eur Radiol. 2005;15:1721–6.
Maturen KE, Nghiem HV, Caoili EM, et al. Renal mass core biopsy: accuracy and impact on clinical management. AJR Am J Roentgenol. 2007;188(2):563–70.
Cluzel P, Martinez F, Bellin MF, et al. Transjugular versus percutaneous renal biopsy for the diagnosis of parenchymal disease: comparison of sampling effectiveness and complications. Radiology. 2000;215(3):689–93.
Lechevallier E, Andre M, Barrol D, et al. Fine-needle percutaneous biopsy of renal masses with helical CT guidance. Radiology. 2000;216:506–10.
Eshed I, Elias S, Sidi AA. Diagnostic value of CT guided biopsy of indeterminate renal masses. Clin Radiol. 2004;59:262–7.
Gesualdo L, Cormio L, Stallone G, et al. Percutaneous ultrasound-guided renal biopsy in supine antero-lateral position: a new approach for obese and non-obese patients. Nephrol Dial Transplant. 2008;23(3):971–6.
Sharma KV, Venkatesan AM, Swerdlow D, et al. Image-guided adrenal and renal biopsy. Tech Vasc Interv Radiol. 2010;13(2):100–9.
He Q, Wang H, Kenyon J, et al. Accuracy of percutaneous core biopsy in the diagnosis of small renal masses (≤4.0 cm): a meta-analysis. Int Braz J Urol. 2015;41(1):15–25.
Marconi L, Dabestani S, Lam TB, et al. Systematic review and meta-analysis of diagnostic accuracy of percutaneous renal tumour biopsy. Eur Urol. 2016;69(4):660–73.
Redfield RR, McCune KR, Rao A, et al. Nature, timing, and severity of complications from ultrasound-guided percutaneous renal transplant biopsy. Transpl Int. 2016;29(2):167–72.
Korbet SM. Nephrology and the percutaneous renal biopsy: a procedure in jeopardy of being lost along the way. Clin J Am Soc Nephrol. 2012;7(10):1545–7.
Stratta P, Canavese C, Marengo M, et al. Risk management of renal biopsy: 1387 cases over 30 years in a single centre. Eur J Clin Invest. 2007;37:954–63.
Uppot RN, Harisinghani MG, Gervais DA. Imaging-guided percutaneous renal biopsy: rationale and approach. AJR Am J Roentgenol. 2010;194(6):1443–9.
Walker PD. The renal biopsy. Arch Pathol Lab Med. 2009;133(2):181–8.
Sateriale M, Cronan JJ, Savadler LD. A 5-year experience with 307 CT-guided renal biopsies: results and complications. J Vasc Interv Radiol. 1991;2(3):401–7.
Manno C, Strippoli GF, Arnesano L, et al. Predictors of bleeding complications in percutaneous ultrasound-guided renal biopsy. Kidney Int. 2004;66(4):1570–7.
Acknowledgments
Nothing to disclose for all authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interests.
Ethical Approval
All procedures performed in this study were in accordance with the ethical standards of local Institutional Review Board committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Written informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Babaei Jandaghi, A., Lebady, M., Zamani, AA. et al. A Randomised Clinical Trial to Compare Coaxial and Noncoaxial Techniques in Percutaneous Core Needle Biopsy of Renal Parenchyma. Cardiovasc Intervent Radiol 40, 106–111 (2017). https://doi.org/10.1007/s00270-016-1466-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-016-1466-3