Abstract
Purpose
The aim of the study was to evaluate the pharmacokinetics and tissue absorption of 2 paclitaxel (PTX) drug-coated balloons (DCB) using different drug loads in a porcine-injured iliac artery model.
Materials and Methods
Twenty-eight pigs were randomized into 2 groups. In group B1, angioplasty was performed with a 1.0 µg/mm2 DCB with PTX and in group B3, with a 3.0 µg/mm2 DCB with PTX. An overstretched model of the iliac artery was used for angioplasty under fluoroscopy. Blood and vessel wall PTX were measured with liquid-chromatography mass spectrometry at 1, 5, 30 min, 1, 7, and 28 days. Remaining drug in the balloon was analyzed.
Results
Mean PTX in blood was significantly higher in the group B3 0.269 ± 0.085 µg/ml compared with the B1 0.218 ± 0.085 µg/ml; p = 0.01. Peak blood PTX concentration was detected at 1 min, and PTX was undetectable 24 h post-angioplasty. There were no statistically significant differences in the mean arterial wall concentration from the treated iliac artery between group-B1 (15.24 ± 21.29 ng/mg) and B3 (15.68 ± 16.33 ng/mg), or in the PTX wall concentration measured at different time points. Mean remaining drug in assayed balloons was lower for group-B1 and represented 8 % of the initial dose.
Conclusions
Blood PTX was higher when using 3.0 µg/mm2 DCB, with a peak drug concentration at 1-min, although the drug was undetectable at 24 h, independently of the loading dose. This study demonstrates no difference in arterial wall uptake of a low dose DCB (1.0 µg/mm2), when compared to a common dose DCB (3.0 µg/mm2) suggesting that the dose of drug in the DCB could be reduced obtaining a similar clinical effect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of drug-eluting stents (DES) and drug-coated balloons (DCB) to reduce neointimal hyperplasia following stenting have become widespread. Neointimal hyperplasia occurs in the coronary artery up to 60 % after stent placement in a 10-year period, leading to patient readmission and repeat revascularization [1]. DES have addressed the issue of in-stent restenosis, but late stent thrombosis and delayed endothelialisation, along with longer dual antiplatelet therapy, are of concern [2]. Recent meta-analysis in the coronary artery showed similar clinical efficacy when compared to DCB [3]. Despite the use of stents, primary plain balloon PTA in selected lesions is performed and it is not free from hyperplasia, but multiple studies have demonstrated superior vessel patency when using DCB [4, 5].
DCB are becoming a promising endovascular tool, because they have the capacity of local drug transfer to the vessel wall, inhibiting cell proliferation and moderating the hypertrophic cell response to injury [6]. An additional benefit of DCB is that they do not leave any foreign body device inside the vessel, which can produce fracture or chronic inflammation.
Nowadays, more than 10 DCB are commercially available with the CE-mark in Europe, with different clinical results [7]. They mainly differ in the loading dose of drug and in the excipient or carrier that transfers the drug to the vessel wall. The current drug of choice is paclitaxel (PTX), a very powerful anti-microtubule agent that inhibits vascular smooth muscle cell proliferation and migration, by blocking the G2 or M phases of the cell cycle [8]. Loading doses of the balloon vary between 2 and 3.5 µg/mm2, being the 3 µg/mm2 dose, the most frequently used [9]. The excipient is the more variable component and is almost exclusive of each commercial brand [10].
Drug transfer does not only depend on the device but also on other factors like: DCB introduction through the sheath, navigation time, type of vessel, and morphology and histology of the lesion. All of these influence the amount of drug that will be absorbed by the vessel wall and thus the clinical outcome. An associated issue is that the drug that does not penetrate in the vessel wall circulates in the bloodstream and may have undesirable effects.
In order to understand the effect of the drug load and the grade of vessel wall uptake and pharmacokinetic of PTX, we carried out this study in a swine model and tested two DCB that only differed in the amount of loaded dose.
Materials and Methods
Device Description
The DCB device in the study was based on the Biotronik Passeo® platform. A 3.0 and a 1.0 µg/mm2 DCB coated with a carrier of BTHC (n-butyryl-tri-n-hexylcitrate) were used.
Both balloons were manufactured using a micro-pipetting technique to apply drug and carrier matrix in a trifold balloon construction. Rigorous testing ensured highest possible standards.
The DCB devices were 6 and 7 mm in diameter by 40 mm in length, in order to achieve a 20 % vessel oversize according to the iliac artery diameter.
Total PTX load in 6 × 40 mm DCB was 2700 µg for the B3 group (3.0 µg/mm2) and 900 µg for the B1 group (1.0 µg/mm2). In case a 7 × 40 mm balloon was used, the PTX loading dose was 3200 µg for the B3 group (3.0 µg/mm2) and 1000 µg for the B1 group (1.0 µg/mm2).
Experimental Procedure
The study protocol was reviewed and approved by the Animal Welfare and Institutional Animal Care and Use Committee of the University UAX and the Spanish Regulations of Health Ministry. The purpose of this study was to evaluate the pharmacokinetics and vessel wall uptake of two DCB based on Passeo platform and BTHC coatings with different PTX drug load. Pharmacokinetics evaluation of the drug released and tissue uptake were evaluated in the iliac arteries by analysis of drug concentration in blood and vessel wall tissue at 1, 30 min, 24 h, 7, and 28 days.
Twenty-eight male healthy commercial hybrid pigs (Sus scrofa domestica) were randomized into two groups, B3 and B1. In the B3 group, the 3.0 µg/mm2 DCB was used and in the B1 group, the 1.0 µg/mm2 DCB. Group and DCB loading dose, were operator-blinded. Age and weight (30 ± 2 kg) of the pigs at implantation were the same in all the procedures.
To prevent or reduce the occurrence of thrombotic events, animals were pretreated daily, with oral acetylsalicylic acid (325 mg) and clopidogrel (75 mg), beginning at least 3 days before intervention and continuing until sacrifice.
Animals were tranquilized with ketamine, azaperone, and atropine administered intramuscularly. Anesthesia induction was achieved with propofol injected intravenously. Upon induction of light anesthesia, the subject animal was intubated and supported with mechanical ventilation. Isoflurane in oxygen was administered to maintain a surgical plane of anesthesia. To prevent postoperative infection, animals were given prophylactic antibiotic Benzylpenicillin intramuscularly.
The access site was prepared with topical application of chlorhexidine, 70 % isopropyl alcohol, and proviodine. The area was then appropriately draped to maintain a sterile field.
A central vein catheter with subcutaneous reservoir was implanted to obtain the blood samples.
The left or right femoral artery was accessed percutaneously under ultrasound-guided puncture. An arterial sheath was introduced and advanced into the artery.
An initial IV bolus of unfractioned heparin (~400 U/kg) was administered and activated clotting time (ACT) was measured at least every 30 min and recorded. If ACT was <300 s, additional heparin was administered.
Drug-Coated Balloon Deployment Procedures
An ultrasound-guided puncture of the right external distal iliac artery was performed and a 5-F introducer sheath was left in place. A hand injection aortoiliac arteriogram with iodinated contrast iopamiro-300 (Iopamidol-300, Bracco SpA) was carried out using a calibrated pigtail catheter to estimate the iliac vessel diameter. The ipsilateral external iliac artery was used as the target vessel. The straight segment between the aortic bifurcation and the gluteal artery landmark was selected (Fig. 1). Thereafter, the balloon was introduced into the selected artery by advancing the balloon catheter, over the guide wire to the deployment site. The balloon was expanded according to the interventionalist’s judgment using the product compliance charts as a guide, to achieve a target balloon to artery ratio of 1.2:1 (Oversize = 20 %), with a range of 1.15:1–1.25:1, estimated visually by the physician and measured by vessel calibration software. Inflation pressure value was between nominal (6 atm) and rated burst balloon pressure (12 atm). Inflation was maintained for 30 s. In each animal, a single inflation of just one balloon (3.0 or 1.0 µg/mm2, blinded to the operator) was performed in one of the external iliacs, using the contralateral as a control, not to interfere with PTX chemical quantitation. An angiogram of the balloon at full inflation was recorded (designated balloon angiography) and the inflation pressure was noted. Complete balloon deflation was verified fluoroscopically. Injection of nitroglycerin IA was administered and final angiograms of the treated vessel were performed at orthogonal angles (designated post-deployment angiographies) and flow was evaluated.
Following successful deployment of balloons and completion of angiography, all catheters and the sheath were removed from the animal and the femoral artery was manually compressed. Balloons were cut-off from the catheters to determine residual PTX in the balloon surface.
After follow-up, the animals were euthanized, at different time points by injecting a lethal intravenous dose of thiopental sodium and a laparotomy was performed for the harvest of different organs and tissue sampling.
PTX Analysis
The pharmacokinetic evaluation of paclitaxel was determined by drawing a 6 ml blood sample in both groups from the femoral sheath during the intervention and from a venous catheter during follow-up at different time points: baseline sample after sheath introduction, 1-min sample (after DCB-angioplasty), 5-min sample, 30-min sample; 24-h sample; 7-day sample; and 28-day sample. At least, three animals were available for blood sample at each time point (Table 1).
Blood samples were transferred into EDTA tubes and then promptly transferred into polypropylene tubes. Tubes were stored on dry ice or placed directly in a −80 °C freezer pending the PK analysis Site.
The treated arteries were excised at necropsy, and kept on dry ice until storage in a −80 °C freezer.
The Blood and tissue PTX concentration measurement were performed by high-performance liquid chromatography (HPLC)/tandem mass spectrometry equipment. PTX powder from Taxus brevifolia and Docetaxel were used as internal standard. The detection limit was 0.02 µg/ml.
PTX concentration in navigated balloons was assayed by a conventional HPLC method.
All animals underwent to a comprehensive necropsy (gross examination of the heart, thoracic, and abdominal organs). Any lesion was collected and kept in neutral-buffered formalin until processed. Samples of grossly normal tissues were also harvested in neutral-buffered formalin at the discretion of the Study Pathologist.
Statistical Analysis
Descriptive and comparative statistics were performed with SPSS software (SPSS Inc, Chicago, IL).
Quantitative variables are displayed as means and standard deviation. In order to compare means, we checked normal distribution of quantitative variables with the Shapiro–Wilk test, discarding normal distribution when p < 0.05.
If normal distribution was observed, Student’s t test and variance test (Levene) were used to compare means. When normal distribution was rejected, we used Mann–Whitney U, Moses, and Kolmogoronov–Smirnov tests as an alternative. p Values <0.05 were considered statistically significant.
Results
DCB PTA and Clinical Follow-up
Technical success was achieved in all cases. There were no cases of dissection or thrombosis related to the DCB angioplasty. The 20 % PTA-vessel oversize target was reached in all the interventions. During follow-up, 2 pigs died unrelated to the procedure. One due to an infectious disease and the other secondary to a neurological disease. Both events occurred during late follow-up. No PTX was detected in blood samples in order to consider a major toxicity of PTX as the cause of death. The pig that died secondary to an infectious complication did not have a progressive deterioration of the blood count during monitoring. No remarkable findings were found in the necropsy.
Therefore, a total of 26 pigs were used for PK analysis and PTX determination in the artery. In 24 cases, the right common iliac artery was the target vessel. In 2 pigs, the target vessel was the left common iliac artery. In 90 % of the procedures, the 6 × 40 mm DCB was chosen.
Mean time from DCB insertion through the sheath to balloon inflation was 11 s, with a mean inflation pressure of 10 atm.
Iliac Artery PTX Concentration
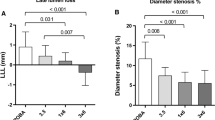
The measured (mean) arterial wall concentration from the treated iliac artery was 15.24 ± 21.29 ng/mg for the group B1 (1.0 µg/mm2 DCB) and 15.68 ± 16.33 ng/mg for the B3 (3.0 µg/mm2 DCB); p = 0.607 (Fig. 2).
Although PTX in artery was very different in the time points studied (30 min, 1, 7, 28 days) between group B1 and B3, there was no statistic significance in the mean values at the end of the studied periods.
There was no significant drop in the amount of PTX in artery in any of the groups, when comparing initial PTX in artery in an early (30 min) and late (28-day) time endpoint. PTX remained in the vessel wall after 28 days with concentrations above 12 ng/mg.
Blood PTX Concentration
PTX was only detectable in blood samples at 1, 5, 30 min, and 24 h interval after DCB inflation. The mean concentration of PTX in group B1 was 0.218 ± 0.085 µg/ml and 0.269 ± 0.085 µg/ml in group B3, being statistically significant (p = 0.012) between the two groups.
The mean PTX was 0.245 ± 0.10 in the 1-min sample and 0.192 ± 0.06 µg/ml in the 30-min sample in the B1 group. In the B3 group, it was 0.301 ± 0.09 in the 1-min sample and 0.237 ± 0.06 µg/ml in the 30-min sample (Fig. 3).
Residual DCB PTX Concentration
PTX remaining on the used balloons was measured after inflation and withdrawal through the arterial sheath. The mean PTX concentration in the 3.0 µg/mm2 DCB group was 215.585 ± 28.70 µg, and in the 1.0 µg/mm2 was 118.846 ± 37.15 µg; (p = 0.183). There was a statistical significant difference between the drug that remained in the 3.0 and 1.0 µg/mm2 DCB. This represents an 8 and 13 % of PTX dose not released during expansion, for the 3.0 and 1.0 µg/mm2 DCB, respectively. There was a statistically significance (p = 0.001) between the percentage released in the 3.0 µg/mm2 DCB, when compared with the 1.0 µg/mm2 DCB.
Discussion
The purpose of this study is to evaluate the PTX pharmacokinetics and vessel wall absorption of two DCBs with different drug load in peripheral vessels. The strength of the study relies on the comparison of 2 different PTX loading doses, using the same balloon platform, carrier and coating technology, thus eliminating multiple confusing factors. The porcine model allowed the evaluation of percutaneous trans-catheter equipment that is typically used for stent placement and PTA evaluation [11]. We conducted the study in porcine iliac arteries, differing the structure of the vessel, and amount of muscular and elastic tissue from other studies that used the coronary arteries. Porcine and human coronary and peripheral artery size and anatomy are similar and this allowed the use of standard clinical devices and accurate visualization using standard angiographic equipment [12]. Hybrid pigs were of a suitable size for studies of up to 28 days. In our study, we have used a low injury model to determine drug retention by the vessel wall and PTX behavior in the bloodstream. This model has proven to be appropriate to test the biological effects of PTX delivered in a DCB [13]. In order to resemble in-human PTA, we have used native vessel without foreign material (stents), based on the constant anatomical landmark of the gluteal artery. The external iliac artery has been a straight, non-tapered vessel that has shown a perfect matching with the DCB used.
PTX was the selected drug as it has proven in multiple reports the property of long-lasting inhibition of the SMC proliferation in the media of the vessel after a short single dose PTA [14–16].
There are few preclinical studies conducted that analyze the behavior of DCB [13, 17, 18]. PTX Blood sample and tissue values are not comparable because of the different animal models, vessel used, DCB technology, inflation protocol, and measurement equipment and methodology. An example of this variability was demonstrated by Posa et al. in an animal model using the same 3.0 µg/mm2, resulting in an increase of tissue PTX concentration depending on the inflation time [19, 23].
Several studies have being performed in order to determine the minimum and maximal dose that may have in vitro and in vivo activities inhibiting neointimal hyperplasia and avoiding toxic side effects. Although 3.0 µg/mm2 DCB are used in patients and has proven the fact, we wanted to demonstrate that by reducing up to one-third the drug load of the balloon, we could obtain similar results [19]. One of the objectives of our study was to test the use of a 1.0 µg/mm2 DCB (not commercially available) and specifically created with the same technology and quality testing that is performed in the clinically used 3.0 µg/mm2 DCB.
Iliac Artery PTX Concentration
The PTX DCB with the BTHC carrier in both platforms demonstrated an effective delivery and retention of the drug by the vessel wall up to the end of follow-up (30 days). The two interventional factors (vessel oversizing target and inflation time) that could influence in the PTX vessel wall uptake were similar in both groups.
The mean PTX uptake in the 3.0 µg/mm2 DCB group was higher than in the 1.0 µg/mm2 DCB without statistical significance. This indicates that there is a similar PTX deposition in the artery regardless of the concentration of drug used in the balloon and that the maximum drug uptake in the artery can be achieved with the lower concentration of PTX. Other study also demonstrated comparable degree of neointimal hyperplasia when lower dose 2 µg/mm2 DCB compared to 3 µg/mm2 DCB [20]. We presume that there might be a vessel wall mechanism that stops absorption of the drug once it reaches a saturation point.
When analyzing the harvested arteries at different time points, we did not find a significant loss of the drug in the artery regardless of the DCB used. This fact can explain that once the PTX is absorbed by the artery wall, it remains stable over time inside the segment of the treated vessel. This resulted in delivery of PTX to the arterial wall up to 1 month. Moreover, the PTX concentration in the artery wall in all time points, and specially at 1 month, with the different loaded balloons ranged from 9.6 to 16.7 ng/mg, and resulted in tissue levels of paclitaxel above the reported IC50 values for human inhibition of SMC (1.4–2 ng/g), and SMC cell culture experiments (1.7–6.8 ng/g) [8]. In the 1.0 µg/mm2 DCB, the mean arterial tissue uptake was 15.24 ng/mg.
Blood PTX Concentration
After PTA, PTX was washed out by the organism in 24 h. It was undetectable in the resolution of our mass spectrometer. No significant lesions were found in any organ at necropsy secondary to bloodstream circulation or theoretical risk of embolization.
Peak blood concentration of PTX was detected 1 min after PTA, being statistically significant, when the 3.0 µg/mm2 DCB was used. This can be justified by the triple dose of PTX that is packed and delivered by the balloon in a homogenous animal model. Peak blood PTX concentration of the 1.0 µg/mm2 DCB is in the range of PTX levels reported by other DCB formulations. Drug slope loss was parallel in both groups, demonstrating a similar washout tendency regardless of the DCB used.
Residual DCB PTX Concentration
DCB was used under the company instructions. Care was taken to protect the balloon when introducing it inside the sheath with the use of a plastic insertion aid. Navigation time inside the vessel was minimized and time to PTA inflation was performed in all cases with a mean time period of 11 s.
There is very little information related to the drug release from DCB [21]. There is a drug loss upon passage of the hemostatic valve of the introducer and in the blood vessel navigation. Afterward there is a second drug loss in the transfer process of the inflated DCB against the vessel wall, mediated by a gradient diffusion and mechanical forces.
The median drug percentage that remained in our balloons was 8 % in B3 and 13 % in B1 group. These data correspond to multiple drug percentages presented in other publications that ranged from 10 to 15 % [18, 22]. It emphasizes that there is no need to transfer all the drug packed in the balloon in order to achieve the goal of inhibiting vessel hyperplasia.
Surprisingly, the drug transfer of the 3.0 µg/mm2 DCB was superior to the 1.0 µg/mm2 DCB. In this scenario, if we consider that the drug uptake by the arterial wall was similar with both balloons, there would be a higher amount of non-effective PTX circulating in blood and tissues when the 3.0 µg/mm2 DCB are used.
When studying the efficiency of the DCB, we found that <1 % of the total loaded dose of PTX was transferred to the vessel wall. Ten percent of the drug was transitorily in the bloodstream the first 24 h and finally added to the 81 % that was absorbed and eliminated by the organism (Fig. 4).
Limitations
The main limitations of our preclinical study were the number of animals used (sample size) because of ethical issues and the overstretched model of a non-diseased vessel that may not totally resemble the behavior of a pathological vessel with an atheroma plaque where PTX uptake may be different. We did not perform a fluorescent marked PTX test to analyze vessel wall pattern of deposition or morphological evaluation of the treated vessel.
Although the main aim of the study was to compare the efficacy of two DCB with different loading dose, comparison at different time points within the group might be biased by the fact that we used arterial sample and venous sample, respectively, for perioperative and follow-up time.
Translational Consideration
Our results support the idea that the 1.0 µg/mm2 DCB is as effective in drug delivery and vessel wall retention as the clinically available 3.0 µg/mm2 DCB. This may lead to the existence of a “saturable vessel wall mechanism,” that could demonstrate the same clinical benefit using the lower concentration of drug. Although higher doses of PTX in commercially DCB are safe and distant from toxic dose major side effects, we think that the use of lower dose DCB may have a role in patients with hepatorenal impairment, hemodialysis fistula stenosis (recirculation of PTX metabolites), and patients with multiple drugs in order to reduce drug interactions.
Conclusions
This study demonstrates no difference in arterial wall uptake of a low dose DCB (1.0 µg/mm2), when compared to a conventional dose DCB (3.0 µg/mm2). The PTX blood levels after PTA with different loaded DCB were undetectable after 24 h. No adverse clinical or pathological effects were found, secondary to PTX. Our data suggest that you could theoretically obtain similar clinical outcomes using lower dose DCB, and that the 1.0 µg/mm2 DCB might be favorable in certain clinical settings.
Clinical studies are necessary to confirm these findings.
References
Duckers HJ, Nabel EG, et al. Essentials of restenosis for the interventional cardiologist. Totowa: Humana Press Inc; 2007.
Camenzind E, Steg PG, Wijns W. Stent thrombosis late after implantation of first-generation drug-eluting stents: a cause for concern. Circulation. 2007;115(11):1440–55.
Lupi A, Rognoni A, Secco GG, Porto I, Nardi F, Lazzero M, et al. Drug eluting balloon versus drug eluting stent in percutaneous coronary interventions: insights from a meta-analysis of 1462 patients. Int J Cardiol. 2013;168(5):4608–16.
Waksman R, Serra A, Loh JP, Malik FT, Torguson R, Stahnke S, von Strandmann RP, Rodriguez AE. Drug-coated balloons for de novo coronary lesions: results from the Valentines II trial. EuroIntervention. 2013;9(5):613–9.
Tacke J, Kieselbach D, Schulte KL. TCT-268 Randomized clinical trial favors the use of drug-coated balloons over plain balloons for the postdilatation of nitinol stents in the SFA and PI segment to lower restenosis rate. J Am Coll Cardiol. 2014; 11(64).
Oberhoff M, Kunert W, Herdeg C, Küttner A, Kranzhöfer A, Horch B, et al. Inhibition of smooth muscle cell proliferation after local drug delivery of the antimitotic drug paclitaxel using a porous balloon catheter. Basic Res Cardiol. 2001;96(3):275–82.
Byrne RA, Joner M, Alfonso F, Kastrati A. Drug-coated balloon therapy in coronary and peripheral artery disease. Nat Rev Cardiol. 2014;11(1):13–23.
Axel DI, Kunert W, Göggelmann C, Oberhoff M, Herdeg C, Küttner A, et al. Paclitaxel inhibits arterial smooth muscle cell proliferation and migration in vitro and in vivo using local drug delivery. Circulation. 1997;96(2):636–45.
Scheller B, Speck U, Abramjuk C, Bernhardt U, Böhm M, Nickenig G. Paclitaxel balloon coating, a novel method for prevention and therapy of restenosis. Circulation. 2004;110(7):810–4.
Radke PW, Joner M, Joost A, Byrne RA, Hartwig S, Bayer G, et al. Vascular effects of paclitaxel following drug-eluting balloon angioplasty in a porcine coronary model: the importance of excipients. EuroIntervention. 2011;7(6):730–7.
Festing MF. The design of animal experiments: reducing the use of animals in research through better experimental design. London: The Royal Society of Medicine Press Limited; 2002.
Schwartz RS, Chronos NA, Virmani R. Preclinical restenosis models and drug-eluting stents: still important, still much to learn. J Am Coll Cardiol. 2004;44(7):1373–85.
Yazdani SK, Pacheco E, Nakano M, Otsuka F, Naisbitt S, Kolodgie FD, et al. Vascular, downstream, and pharmacokinetic responses to treatment with a low dose drug-coated balloon in a swine femoral artery model. Catheter Cardiovasc Interv. 2014;83(1):132–40.
Patterson C, Mapera S, Li HH, Madamanchi N, Hilliard E, Lineberger R, et al. Comparative effects of paclitaxel and rapamycin on smooth muscle migration and survival: role of AKT-dependent signaling. Arterioscler Thromb Vasc Biol. 2006;26(7):1473–80.
Lavigne MC, Eppihimer MJ, Cheng R, Barry JJ. Anti-proliferative compounds for the prevention of restenosis. Curr Pharm Des. 2010;16(36):3989–4001.
Parry TJ, Brosius R, Thyagarajan R, Carter D, Argentieri D, Falotico R, et al. Drug-eluting stents: sirolimus and paclitaxel differentially affect cultured cells and injured arteries. Eur J Pharmacol. 2005;524(1–3):19–29.
Fernández-Parra R, Laborda A, Lahuerta C, Lostalé F, Aramayona J, de Blas I, de Gregorio MA. Pharmacokinetic Study of Paclitaxel Concentration after drug-eluting balloon angioplasty in the iliac artery of healthy and atherosclerotic rabbit models. J Vasc Interv Radiol. 2015;26(9):1380–7.
Kelsch B, Scheller B, Biedermann M, Clever YP, Schaffner S, Mahnkopf D, et al. Dose response to Paclitaxel-coated balloon catheters in the porcine coronary overstretch and stent implantation model. Invest Radiol. 2011;46(4):255–63.
Scheinert D, Duda S, Zeller T, Krankenberg H, Ricke J, Bosiers M, et al. The LEVANT I (Lutonix paclitaxel-coated balloon for the prevention of femoropopliteal restenosis) trial for femoropopliteal revascularization: first-in-human randomized trial of low-dose drug-coated balloon versus uncoated balloon angioplasty. JACC Cardiovasc Interv. 2014;7(1):10–9.
Gongora CA, Shibuya M, Wessler JD, McGregor J, Tellez A, et al. Impact of paclitaxel dose on tissue pharmacokinetics and vascular healing: a comparative drug-coated balloon study in the familial hypercholesterolemic swine model of superficial femoral in-stent restenosis. JACC Cardiovasc Interv. 2015;8(8):1115–23.
Seidlitz A, Nagel S, Semmling B, Petersen S, Reske T, Schmidt W, et al. In vitro estimation of drug loss during the implantation procedure of drug-eluting stents. Biomed Eng-Biomed Te. 2012;57:403–6.
Scheller B. Opportunities and limitations of drug-coated balloons in interventional therapies. Herz. 2011;36(3):232–9.
Pósa A, Nyolczas N, Hemetsberger R, Pavo N, Petnehazy O, Petrasi Z, et al. Optimization of drug-eluting balloon use for safety and efficacy: evaluation of the 2nd generation paclitaxel-eluting DIOR-balloon in porcine coronary arteries. Catheter Cardiovasc Interv. 2010;76(3):395–403.
Acknowledgments
Research grant from Biotronik.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Abadal received a grant from Biotronik, during the conduct of the study.
Ethical Approval
All applicable institutional and/or national guidelines for the care and use of animals were followed.
Rights and permissions
About this article
Cite this article
Abadal, J.M., Vazquez, E., Morales, M. et al. Pharmacokinetic Evaluation of Two Paclitaxel-Coated Balloons with Different Drug Load in a Short-Term Porcine Study. Cardiovasc Intervent Radiol 39, 1152–1158 (2016). https://doi.org/10.1007/s00270-016-1346-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-016-1346-x