Abstract
Purpose
To evaluate the outcome of patients with melanoma liver metastasis treated with stereotactic radiofrequency ablation (SRFA).
Material and Method
Following IRB approval, a retrospective evaluation of the treatment of 20 patients with 75 melanoma liver metastases was performed.
Results
A median number of 2 lesions (range 1–14) per patient with a median size of 1.7 cm (range 0.5–14.5 cm) were treated. 67 lesions were <3 cm (89.3 %) and 8 lesions were >3 cm (10.7 %). Per patient a median of 1 ablation session was performed (range: 1–4) totaling 34 sessions. There were no procedure-related deaths and all major complications (n = 3) could be easily treated by pleural drainages. The primary and secondary success rates were 89.3 and 93.3 %, respectively. The overall local recurrence rate was 13.3 %. Four of ten local recurrences were re-treated successfully by SRFA. During follow-up, 9/20 patients developed extrahepatic metastatic disease and 10/20 had liver recurrence at any location. The median OS from the date of SRFA was 19.3 months, with an OS of 64, 41, and 17 % at 1, 3, and 5 years, with no significant difference for patients with cutaneous and ocular melanoma. The median DFS after SRFA for all 20 patients was 9.5 months, with 37, 9, and 0 % at 1, 3, and 5 years.
Conclusions
Due to the high local curative potential and the promising long-term survival rates associated with minimal morbidity and mortality, radiofrequency ablation seems to be an attractive alternative to resection in patients with melanoma liver metastases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of melanoma is increasing worldwide, up to one-third of patients developing distant metastasis. 10 % of these patients present with liver metastases [1]. The median survival of patients after diagnosis of liver metastases from cutaneous and ocular melanoma ranges from 2 to 8 months [1–3]. Conventional chemotherapy has shown treatment response rates ranging from only 10 to 30 % [3, 4]. Unfortunately, responses to modern immunotherapeutic drugs appear to be temporary in almost all cases [2]. Thus, treatment of melanoma liver metastases requires at least a combination of systemic with locoregional therapy.
Hepatectomy may improve survival in patients with limited hepatic disease [5–7]. However, due to the dismal prognosis the question arises whether invasive surgery is warranted.
Radiofrequency ablation (RFA) may be a minimal invasive alternative. However, up to now only very few patients with melanoma liver metastases included in large case series were reported [8–11]
In this retrospective review of our prospective electronic institutional database, we report our experience with CT-guided multi-probe stereotactic RFA [12–14] in the treatment of 20 patients with a total of 75 melanoma liver metastases over an 8-year period. For SRFA, a frameless stereotactic navigation system is used to plan and introduce multiple probes in order to treat also large tumors. In addition, image fusion is used for evaluation of probe positioning accuracy and coverage of the tumor by the ablation zone. SRFA requires general anesthesia and is more time-consuming as compared to conventional RFA [15, 16].
To the best of our knowledge, this is the first RFA case series including patients with melanoma liver metastases only.
Materials and Methods
Patients
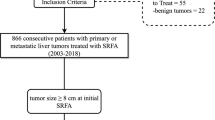
With approval from our institutional review board, we retrospectively reviewed our prospective database of all patients with melanoma liver metastases who were consecutively treated by percutaneous stereotactic radiofrequency ablation (SRFA) at our department from January 2005 to December 2013.
Only patients with a maximum of 5 melanoma metastases confined to the liver at initial presentation were treated by SRFA.
Additional exclusion criteria were an abnormal coagulation status or liver function and tumors in close vicinity to the central bile ducts (<1 cm).
20 consecutive patients (14 men, 6 women) with a median age of 60 years (range 42–76 years) with 1–5 liver metastases at initial presentation (mean 2.05, median 2, SD 1.2) were identified and included in the study.
In total, 75 liver lesions (41 lesions at first presentation, 24 lesions detected during follow-up, and 10 local recurrences) were treated in 34 SRFA sessions. The primary tumor was ocular in 6 patients and cutaneous in 14 patients, respectively. Local treatment of the primary ocular melanoma included enucleation (n = 6). In the patients with cutaneous melanoma, the primary tumors were treated by wide local excision (n = 4) or wide local excision plus lymph node dissection (LND) (n = 10), respectively. All patients received systemic chemotherapy (n = 20).
RFA was considered the treatment of choice after discussing each case with the institutional interdisciplinary tumor board consisting of dermatologists, oncologists, surgeons, and radiologists. Standard preoperative evaluation of patients with metastatic melanoma included baseline history, physical examination, serum laboratory tests, and contrast-enhanced computed tomography (CT) of the chest, abdomen, and pelvis.
Informed consent was obtained from all individual participants included in the study. None of the patients had undergone previous local treatments for the liver metastases.
Table 1 gives a detailed overview about the clinical and pathological features of the 20 consecutive patients who underwent SRFA between 2005 and 2013.
The maximum tumor size was 14.5 cm and the maximum number of lesions per patient treated during the observation period was 14.
The liver metastases were synchronous in 3 patients, and metachronous in the remaining 17 patients.
RFA
The aim of radiofrequency ablation is the induction of a thermal lesion by electric energy. Due to the high tissue impedance and the resulting friction of the ions, focused heating in the tissue around the tip of the RFA probe is induced, resulting in coagulation necrosis. The alternating current flows between the uninsulated probe tip and a dispersive skin electrode. The unipolar rapid-switching multiple-electrode RF system Tyco Cooltip (Covidien, Burlington, Massachusetts, USA) is based on three cooled monopolar electrodes and a rapid-switching multi-electrode control. RFA is performed during a 16-min ablation per cycle, allowing for simultaneous treatment of multiple tumors.
Procedure (Fig. 1)
RFA probes were inserted into the tumor by stereotactic CT guidance in general anesthesia and with respiratory triggering. Perioperative intravenous broadband antibiotics (1500 mg cefuroxime) were administered as a single shot 30 min prior to RFA probe insertion.
SRFA procedure in a patient with 2 melanoma liver metastases. A Trajectory planning for multiple RFA probe positions in order to cover the whole tumor (including a safety margin) by the ablation zone. Two liver metastases from ocular melanoma were treated in one session. For the visible lesion, five trajectories (one central and four in the periphery of the lesion) were planned on the 3D dataset with a maximum inter-probe distance of 2 cm. B For registration, skin fiducials are indicated by the navigation probe and correlated on the 3D dataset. C After sterile draping, the tracker (purple) of the navigation system is introduced into the aiming device (black) and aligned with the virtual path. Thereafter, the coaxial needles are introduced through the aiming device to the preplanned depth (not visible). D Superposition of control CT (with coaxial needles) to the planning CT (with the planned trajectories) for checking the accuracy of needle placement. Note the precise alignment between the planned path (blue lines in the upper and lower left quadrant) and the respective needle. E Ablation is performed by simultaneous activation of three RFA probes (1,2,3) that are sequentially introduced into the coaxial needles. F Contrast-enhanced control CT after ablation. Due to image fusion with the planning CT, the ablation result can be evaluated in the identical reformatted planes by blending between the two different datasets from 0 % (see A) to 100 % (visible) (Note the slide bar “Blend setting”)
The technique of stereotactic radiofrequency ablation using multiple RFA probes has been described in detail [13, 14]. In brief, the anesthetized patient was immobilized in a vacuum cushion on the CT table. 8–10 fiducial markers were attached to the patient. A contrast-enhanced CT was acquired during temporary disconnection of the tracheal tube (TT) for control of respiration. On the Treon frameless stereotactic navigation system (Medtronic Inc., Boulder, Colorado, USA), multiple pathways were planned using multiplanar and 3D reconstructions of the CT dataset. Unsterile patient registration was performed by indicating the real fiducials on the patient with a probe and correlation of the virtual markers on the CT dataset. After checking the registration accuracy, sterile draping of the patient was performed. A dedicated aiming device (Atlas, Medical Intelligence Inc., Schwabmünchen, Germany) was used to advance the coaxial needles along the planned trajectory to the target. During every needle placement, a temporary disconnection of the TT for a few seconds was performed. The coaxial needles served as guides for the radiofrequency electrodes.
To verify correct needle placements, a native control CT in TT disconnection was performed and fused with the planning CT. A biopsy sample was obtained via the coaxial needles. Subsequently, radiofrequency electrodes were introduced via the coaxial needles for serial tumor ablation. After hot withdrawal of the RFA probes, a contrast- enhanced CT was obtained to exclude complications. In addition, superpositioning of the contrast-enhanced control CT to the planning CT by means of image fusion may help to verify complete ablation of the tumor. If the intended safety margin is not achieved in three dimensions, the procedure may be continued.
Follow-up CT scans were performed one month after SRFA and every three months thereafter.
Statistical Analysis
Primary technical effectiveness rate was assessed for every metastasis on the basis of the absence of residual tumor in the 1-month CT control after initial treatment. Secondary technique effectiveness rate included lesions that had undergone re-ablation after identification of local tumor progression in the 1-month CT control. Major complications were defined as events that increased the level of care and led to a prolonged hospital stay. Patient survival was calculated from the date of SRFA to the date of death (event) or the most recent follow-up visit (censoring). Evaluation of recurrence-free time was performed on per-lesion and per-patient bases. Statistical analysis was performed by PASW Statistics, version 15.0 (SPSS, Chicago, IL). Survival estimates were calculated by the Kaplan–Meier and life table method.
Results
A median number of 2 lesions (range 1–14) per patient with a median size of 1.7 cm (range 0.5–14.5 cm) were treated. 67 lesions were <3 cm (89.3 %) and 8 lesions were >3 cm (10.7 %) totaling 75 liver lesions. Per patient 1–4 ablation sessions were performed totaling 34 sessions.
Complications
There were no procedure-related deaths. In 34 SRFA sessions, a total of 3 complications (3 pleural effusions) requiring pleural drainages postoperatively occurred. The median length of hospitalization was 4.5 days (range 2–18 days). Despite treatment of large liver metastases, no relevant liver function impairment was observed.
Primary and Secondary Success Rates
The primary success rate was 89.3 % (67/75). Residual tumor was re-treated in 3 patients, resulting in a secondary success rate of 93.3 % (70/75).
Local Recurrence
According to Kaplan–Meier estimation, local recurrence-free survival rates were 85 % at 1 year and 76 % at 3 and 5 years (Fig. 2).
Despite precise probe placement by stereotactic RFA, local recurrence was observed in 10/75 tumors (13.3 %). A detailed overview about the features of the recurring nodules is given in Table 2. In two large tumors, the intended safety margin of 1 cm could not be achieved due to the vicinity to large vessels and extensive infiltration of the diaphragm. Retrospective analysis revealed proximity to hollow organs in two cases as possible explanations. The remaining six local recurrences in four different patients may have been avoided by placement of additional probes and by discrete analysis of image fusion between the planning and control CT with subsequent placement of additional probes. Unfortunately, this option was not exploited in these cases, despite borderline ablation margins (<1 cm). However, four of ten local recurrences were successfully re-treated by SRFA.
Distant Recurrence
1/6 (16.6 %) patients with ocular melanoma and 8/14 (57.1 %) with cutaneous melanoma developed extrahepatic metastatic disease during follow-up. The following organs were involved: lung (6 patients), brain (4 patients), distant lymph nodes (5 patients), peritoneal (2 patients), and bone (1 patient). During the follow-up period, 10/20 patients (50 %) had liver recurrence at any location.
Overall Survival and Disease-Free Survival
Among all patients, the median OS from the date of SRFA was 19.3 months, with an OS of 64, 41, and 14 % at 1, 3, and 5 years, (Fig. 3A).
Overall survival (OS) rates from the date of SRFA in months grouped by prognostic factors. A Overall survival (OS) including all patients. B Overall survival (OS) of patients with ocular versus cutaneous melanoma. C Overall survival (OS) of patients depending on patient age (<70 vs. >70 year). D Overall survival (OS) depending on lesion size (<3 vs. >3 cm)
The median overall survival (OS) from the date of SRFA of ocular melanoma diagnosis was 38 months, and for cutaneous melanoma 11.6.
If those four patients are excluded, which would have required further treatment in the same session due to insufficient ablation margin as revealed by image fusion, the median OS from the date of SRFA was 15.7 months, with an OS of 55, 39, and 24 % at 1, 3, and 5 years.
The factors affecting OS are depicted in Fig. 3B–D. Tumor type (p = 0.063), patient age (p = 0.213), size of metastasis (p = 0.365), and number of metastases (p = 0.646) did not significantly affect OS.
The median disease-free survival (DFS) from the date of SRFA for all 20 patients was 9.3 months, with 37, 9, and 0 % at 1, 3, and 5 years (Fig. 4).
Discussion
The role of liver resection with local curative intent for patients with metastatic melanoma is still controversial. In four major referral centers, 40 patients underwent hepatic resection for melanoma over a 12-year period. The study included 24 patients with cutaneous and 16 patients with ocular melanoma [7]. A short median time to recurrence from liver resection (8.3 months), a median survival of 28.2 months, and a 10.9 % 5-year survival with no significant difference between ocular and cutaneous melanoma were reported.
An evaluation of the two largest melanoma databases worldwide from the John Wayne Cancer Institute and the Sydney Melanoma Unit [6] showed that only a very limited number of melanoma patients with liver metastases qualify for aggressive surgical treatment. After meticulous selection, only 24/1750 patients presenting with liver metastases from melanoma were finally resected. However, in this highly selected group a 5-year overall survival of 29 % could be achieved.
In recent years, minimal invasive local palliative transarterial treatments for liver metastases, including transarterial chemoembolization (TACE) [17], selective internal radiation therapy (SIRT) [18], hepatic arterial infusion (HAI), and isolated hepatic arterial perfusion (IHP) have been introduced [19]. Most of the evidence for these treatment modalities is based on small, non-comparative, single-institution studies. In seven small case studies, an overall survival of 5.2–11.5 months was achieved by transarterial chemoembolization (with Cisplatin, Carboplatin, and Doxorubicin in various combinations with polyvinyl sponge and ethiodized oil) [19].
Carling et al. [20] have evaluated treatment response and complications of irinotecan (DEBIRI) transarterial chemoembolization in 14 patients with melanoma liver metastases. From the time of treatment, an overall survival of 9.4 months (range 1.7–39) was achieved. There were 12 major complications in nine patients, possibly including one case of mortality due to disseminated intravascular coagulation (DIC).
Recently, minimal invasive local ablation therapies including radiofrequency ablation (RFA), cryotherapy, and focused ultrasound have served as an alternative to resection. In most centers, RFA is the first choice for percutaneous ablation of unresectable liver malignancies. The therapeutic efficiency and the low morbidity and mortality of radiofrequency ablation of primary and secondary liver tumors have been reported in a number of clinical studies [14, 21, 22].
In a retrospective study [2] among a total of 1078 patients with ocular or cutaneous melanoma liver metastases, only 58 (5.4 %) were selected for local curative therapy (resection ± ablation). Median and 5-year overall survival from hepatic metastasis diagnosis was 8 months and 6.6 %, respectively, for non-surgical patients versus 24.8 months and 30 %, respectively, for surgical patients (p < 0.001). Median OS was similar among patients undergoing ablation (with or without resection) relative to those undergoing surgery alone. Patients selected for locoregional therapy experienced markedly improved survival relative to those receiving only medical therapy.
Apart from that, there are very limited reports available describing RFA for unresectable metastatic melanoma to the liver [10, 11, 23–25]. In all these studies, only a few patients with melanoma metastases were part of large studies. The results were not described individually and no specific details were provided regarding the patients with melanoma.
To the best of our knowledge, the current paper is the first paper focusing on radiofrequency ablation of melanoma liver metastases only. Our results with a median OS of 19.3 months of patients with melanoma liver metastasis and an OS of 64, 41, and 14 % at 1, 3, and 5 years from the date of RFA despite the inclusion of 2 patients with liver metastases of >10 cm in diameter are well comparable with the results after liver resection.
Due to the similar local curative potential associated with 2–4 times lower mortality and morbidity as compared to surgery, RFA seems to be an attractive alternative to resection in patients with melanoma liver metastases.
The authors are well aware of the disadvantages of a nonrandomized retrospective evaluation. Unfortunately, the precise criteria for treatment selection cannot be fully known. The small patient number including patients with ocular and cutaneous melanoma is explained by the fact that only a small number of patients with liver metastases are considered suitable for local curative therapy. This is also reflected by the fact that even in the largest centers worldwide only a very low percentage of patients with melanoma liver metastases undergo surgical (resection ± ablation) therapy, and in most surgical publications ocular and cutaneous melanoma liver metastases are reported simultaneously.
Further studies will be required to evaluate the role of RFA in the treatment of melanoma liver metastasis. In analogy to resection, appropriate selection of patients is crucial and it may be considered only in those cases where all diseases can be addressed and a disease-free stage can be achieved. In addition, locoregional treatment of liver metastases should be combined with systemic chemotherapy [26].
Conclusion
A few highly selected patients where all disease can be addressed can benefit from local curative treatment of the liver metastases. Due to its low complication rates and similar local recurrence rates and survival rates as compared to conventional liver surgery, SRFA is a very attractive alternative.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Abbreviations
- CT:
-
Computed tomography
- TT:
-
Tracheal tube
- LND:
-
Lymph node dissection
- MRI:
-
Magnetic resonance imaging
- RFA:
-
Radiofrequency ablation
- SRFA:
-
Stereotactic radiofrequency ablation
References
Leiter U, Meier F, Schittek B, Garbe C. The natural course of cutaneous melanoma. J Surg Oncol. 2004;86(4):172–8.
Faries MB, Leung A, Morton DL, et al. A 20-year experience of hepatic resection for melanoma: is there an expanding role? J Am Coll Surg. 2014;219(1):62–8.
Barth A, Wanek LA, Morton DL. Prognostic factors in 1,521 melanoma patients with distant metastases. J Am Coll Surg. 1995;181(3):193–201.
Soni S, Lee DS, DiVito J Jr, et al. Treatment of pediatric ocular melanoma with high-dose interleukin-2 and thalidomide. J Pediatr Hematol Oncol. 2002;24(6):488–91.
Caralt M, Marti J, Cortes J, et al. Outcome of patients following hepatic resection for metastatic cutaneous and ocular melanoma. J Hepatobiliary Pancreat Sci. 2011;18(2):268–75.
Rose DM, Essner R, Hughes TM, et al. Surgical resection for metastatic melanoma to the liver: the John Wayne Cancer Institute and Sydney Melanoma Unit experience. Arch Surg. 2001;136(8):950–5.
Pawlik TM, Zorzi D, Abdalla EK, et al. Hepatic resection for metastatic melanoma: distinct patterns of recurrence and prognosis for ocular versus cutaneous disease. Ann Surg Oncol. 2006;13(5):712–20.
Eisele RM, Neumann U, Neuhaus P, Schumacher G. Open surgical is superior to percutaneous access for radiofrequency ablation of hepatic metastases. World J Surg. 2009;33(4):804–11.
Schumacher G, Eisele R, Spinelli A, et al. Indications for hand-assisted laparoscopic radiofrequency ablation for liver tumors. J Laparoendosc Adv Surg Tech A. 2007;17(2):153–9.
Siperstein A, Garland A, Engle K, et al. Laparoscopic radiofrequency ablation of primary and metastatic liver tumors. Technical considerations. Surg Endosc. 2000;14(4):400–5.
Bleicher RJ, Allegra DP, Nora DT, Wood TF, Foshag LJ, Bilchik AJ. Radiofrequency ablation in 447 complex unresectable liver tumors: lessons learned. Ann Surg Oncol. 2003;10(1):52–8.
Bale R, Freund M, Bodner G, Kovacs P, Jaschke W. Precise Computer-assisted liver tumor puncture for biopsy and thermal ablation. Radiology. 2002;225(S):242.
Bale R, Widmann G, Haidu M. Stereotactic radiofrequency ablation. Cardiovasc Intervent Radiol. 2011;34(4):852–6.
Bale R, Widmann G, Schullian P, et al. Percutaneous stereotactic radiofrequency ablation of colorectal liver metastases. Eur Radiol. 2012;22(4):930–7.
Bale R, Widmann G, Stoffner DI. Stereotaxy: breaking the limits of current radiofrequency ablation techniques. Eur J Radiol. 2010;75(1):32–6.
Bale R, Widmann G, Jaschke W. Navigated open, laparoscopic, and percutaneous liver surgery. Minerva Chir. 2011;66(5):435–53.
Huppert PE, Fierlbeck G, Pereira P, et al. Transarterial chemoembolization of liver metastases in patients with uveal melanoma. Eur J Radiol. 2010;74(3):e38–44.
Gonsalves CF, Eschelman DJ, Sullivan KL, Anne PR, Doyle L, Sato T. Radioembolization as salvage therapy for hepatic metastasis of uveal melanoma: a single-institution experience. AJR Am J Roentgenol. 2011;196(2):468–73.
Sato T. Locoregional management of hepatic metastasis from primary uveal melanoma. Semin Oncol. 2010;37(2):127–38.
Carling U, Dorenberg EJ, Haugvik SP, et al. Transarterial chemoembolization of liver metastases from uveal melanoma using irinotecan-loaded beads: treatment response and complications. Cardiovasc Intervent Radiol. 2015;38:1532–41.
Livraghi T, Solbiati L, Meloni MF, Gazelle GS, Halpern EF, Goldberg SN. Treatment of focal liver tumors with percutaneous radio-frequency ablation: complications encountered in a multicenter study. Radiology. 2003;226(2):441–51.
Mulier S, Mulier P, Ni Y, et al. Complications of radiofrequency coagulation of liver tumours. Br J Surg. 2002;89(10):1206–22.
Berber E, Ari E, Herceg N, Siperstein A. Laparoscopic radiofrequency thermal ablation for unusual hepatic tumors: operative indications and outcomes. Surg Endosc. 2005;19(12):1613–7.
Eisele RM, Zhukowa J, Chopra S, et al. Results of liver resection in combination with radiofrequency ablation for hepatic malignancies. Eur J Surg Oncol. 2010;36(3):269–74.
Helton WS. Ocular melanoma metastatic to the liver: the role of surgery in multimodality therapy. Ann Surg Oncol. 2004;11(3):242–4.
Chapman PB, Hauschild A, Robert C, et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364(26):2507–16.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Reto Bale is a co-inventor of the Atlas aiming device and a co-shareholder in its financial returns. The other authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Bale, R., Schullian, P., Schmuth, M. et al. Stereotactic Radiofrequency Ablation for Metastatic Melanoma to the Liver. Cardiovasc Intervent Radiol 39, 1128–1135 (2016). https://doi.org/10.1007/s00270-016-1336-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-016-1336-z