Abstract
Purpose
To evaluate outcomes following treatment of transplant renal artery stenosis by percutaneous transluminal angioplasty and stent insertion.
Materials and Methods
A literature search was performed using Pubmed, MEDLINE, Embase, Wiley Interscience and the Cochrane Library databases. Outcome measures were glomerular filtration rate, creatinine, blood pressure and number of antihypertensive medications. Technical and clinical success, patency and complication rates were also analysed.
Results
Thirty-two studies met the inclusion criteria, involving a total of 884 interventions including PTA, stenting, or combinations of both. Clinical success rates were in the range 65.5–94 %. The majority of studies reported technical success rates higher than 90 %. Patency rates were in the range of 42–100 %. However, the definition and diagnostic criteria for TRAS varied widely between studies. Also, marked heterogeneity was observed in the reporting of outcome measures with no consensus in outcome criteria or follow up schedule.
Conclusion
Outcomes following PTA and stenting for the treatment of TRAS have been shown to be favourable. However, there is a distinct lack of well designed studies assessing outcomes following intervention. Outcome reporting may be improved by the introduction of standardised outcome measures with reporting of outcomes into a multi-centre registry.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Transplant renal artery stenosis (TRAS) is the most common vascular complication following renal transplantation with a reported incidence of 1–23 % [1]. The disease is often asymptomatic and unrecognised, and despite being a potentially reversible cause of refractory hypertension and graft dysfunction in kidney transplant recipients, it is associated with poor long term patient and allograft survival [2].
Reported cases of TRAS have progressively increased in parallel with the increasing use of non-invasive investigation procedures which may arouse suspicion of the disease even in non-symptomatic cases. The wide reported range of TRAS incidence may also reflect the lack of standardisation in the definition of haemodynamically significant disease [3].
A consensus regarding the management of TRAS remains elusive due to a lack of good quality published data, with some authors advocating intervention with percutaneous transluminal angioplasty (PTA) with or without endovascular stenting [4], whilst others recommend a more conservative approach [5].
PTA has been demonstrated to be efficacious in the treatment of TRAS in terms of short-term improvement in renal function. However, data on the long-term effects of PTA on graft survival are scarce and primarily from uncontrolled studies [3]. The recurrence rate of TRAS following PTA may be as high as 40 %, and the subsequent management in this setting remains controversial [6]. Therapeutic options include repeat PTA, surgery and intra-arterial stenting.
The aim of this systematic review is to evaluate the reporting of outcomes following treatment of TRAS with PTA and/or endovascular stenting.
Methodology
An electronic search was performed using Pubmed (January 2000 to May 2014), MEDLINE (January 2000 to May 2014), Embase (January 2000 to May 2014), Wiley Interscience (January 2000 to May 2014) and the Cochrane Library databases (2014). Search terms ‘transplant renal artery’, ‘transplant renal artery stenosis’, ‘transplant renal artery stent’, ‘transplant renal artery PTA’, ‘transplant renal artery stenosis treatment’, ‘transplant renal artery stenosis management’, ‘kidney transplant artery stenosis’, ‘kidney transplant artery stent’, ‘kidney transplant artery PTA’, ‘transplant renal artery endovascular’ and ‘transplant renal artery intervention’ were used in combination with the Boolean operator OR. Two authors performed the search independently in May 2014. The reference lists of articles obtained were also searched manually to identify further relevant citations.
Abstracts of the citations identified by the search were then scrutinised in order to determine eligibility for inclusion in this systematic review. Studies were included if they met each of the following criteria
-
Describe the use of angioplasty and/or stenting to treat transplant renal artery stenosis.
-
Published from 2000 onward.
-
Published in English.
-
Studied a minimum of ten patients.
Both case series and cohort studies were included in this review. In the case of serial publications by the same authors, this review considered only the most recent publication. Data from included studies was collated by Ngo, Lijister, and Markar. The outcome measures for the systematic review were glomerular filtration rate (GFR), creatinine, systolic blood pressure, diastolic blood pressure and number of anti-hypertensives pre- and post- intervention. Technical and clinical success, patency and complication rates were also studied.
Results
The literature search yielded 32 publications which comprised 26 (81 %) case series and 6 (19 %) cohort studies. Twenty-six studies (81 %) were performed retrospectively and 6 (19 %) prospectively. Twenty-eight were single centre studies. The majority of patients across the studies were male (67 %, M/F = 500/248, where recorded), with an age range of 10–79. The total number of patients included in the studies reviewed was 4048.
Intervention
A total of 884 interventions were performed for cases of transplant renal artery stenosis. These comprised 422 percutaneous transluminal angioplasties and 415 stent procedures. The remaining 47 procedures were performed in studies where PTA and stented patients were grouped into a single ‘intervention’ arm and could not be otherwise differentiated.
Seven studies included patients following PTA as the sole treatment for TRAS (n = 137) [7–13]. Eleven studies included patients following stenting alone (n = 201) [1, 2, 6, 14–21]. Twelve studies involved patients receiving either PTA alone or stenting with pre balloon dilatation (n = 407, of which PTA alone = 271, stent following PTA = 89, and PTA and/or stent following PTA not discriminated in a single intervention arm = 47) [3, 5, 22–31]. In all twelve studies, patients were followed up as a single intervention arm when considering outcomes, with no differentiation made between those treated with PTA or stenting.
The final two studies followed patients having received PTA or stenting alone (n = 139, of which PTA only n = 14 and stent only n = 125), however, grouped all patients together when analyzing all outcomes other than patency rate [32, 33].
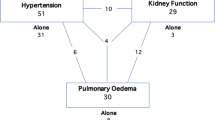
Risk Factors
There was a wide variation in the reporting of patient co-morbidities and risk factors for TRAS. The most commonly assessed co-morbidity was diabetes mellitus, recorded in 12 studies and present in 26 % of patients (n = 417). Hypertension was recorded in eight papers and present in 69 % (range 11–100 %) of the study population (n = 145). Dyslipidaemia was documented in five studies and present in 57 % of patients (n = 98), and smoking was reported in 21 % of patients (n = 53). Five studies [3, 8, 12, 13, 27] recorded the CMV status in their study population, which was overall found to be 52 % (n = 68, range 10–100 %).
Assessment of TRAS
The diagnosis of TRAS was derived using a range of imaging modalities, either in isolation or in combination, including Doppler ultrasound, magnetic resonance angiography (MRA), computed tomography angiography (CTA) and digital subtraction angiography (DSA).
Doppler ultrasound was used as the sole modality in assessing for TRAS in seven studies [1, 3, 5, 16, 17, 19, 20], and in combination with DSA in ten studies [2, 7, 11, 23–28, 32]. A combination of Doppler ultrasound, MRA and DSA were used in six studies [10, 15, 18, 22, 30, 31]. One study utilised Doppler ultrasound followed by MRA and DSA, with CTA reserved for patients only in whom MRA could not be performed [33]. A combination of ultrasound, CTA, MRA and DSA were used in two studies [12, 13].
DSA was used as the sole method for diagnosing TRAS in four studies [6, 8, 14, 29]. The remaining two studies did not disclose the method of diagnosis of TRAS.
Diagnostic Criteria for TRAS
The diagnostic criteria for TRAS showed wide variability between studies. Where Doppler ultrasound was utilised (28 studies), the most commonly accepted flow measurement at which TRAS was deemed to be present was at a peak systolic velocity (PSV) of >2 m/s (13 studies). Several studies incorporated further parameters deemed to represent TRAS. Two separate papers defined TRAS as a PSV >2.2 and >2.5 m/s. One study measured the degree of narrowing, with a >50 % stenosis deemed diagnostic for TRAS [2] (Table 1).
Flow velocities were measured in five studies within the stenotic segment and compared with pre- and/or post-stenosis segments. In all five studies, TRAS was defined by an increase in PSV of 50 % within the stenotic segment. Where ratios in flow velocities were calculated between the stenotic:pre-/post- stenotic segment, a ratio of 2:1 was accepted to represent TRAS [22, 28]. Eleven studies did not disclose the ultrasound criteria for diagnosis of TRAS.
In the 22 studies whereby DSA was utilised, 4 defined TRAS as stenosis of >50 % at angiography. Three studies deemed a >10 % peak systolic blood pressure gradient across the stenosis to be significant for TRAS [23, 26, 31], whilst one study considered a >15 mmHg pressure drop across the stenosed lesion to represent TRAS [33]. Three studies defined TRAS as 70 % luminal narrowing [7, 19, 20], with one study each defining TRAS at 60 and 75 % stenosis [25, 28]. The remaining nine studies failed to disclose their diagnostic criteria (Table 2).
In the seven studies where MRA was performed, TRAS was considered where there was >50 % stenosis in one study [22], and >70 % in another [31]. The remaining six studies did not state the diagnostic criteria [10, 12, 13, 15, 18, 30].
Interventional Technique
Nineteen studies (59 %) provided an account of the angiographic technique utilised in performing angioplasty and/or deployment of stents, where applicable. Of the 24 studies in which endovascular stents were deployed, only 9 (38 %) disclosed the type of stent used (Table 3) [2, 14, 18–21, 30, 32, 33].
Outcome Measures
Glomerular Filtration Rate
Eleven studies (34 %) recorded GFR as an outcome measure (n = 201) [1, 5, 6, 14, 15, 17, 18, 23, 25, 27, 32]. These included six studies where stent insertion was the primary intervention, with or without pre-angioplasty (n = 100) [1, 5, 14, 17, 18, 24]. These studies all reflect an improvement in GFR following intervention ranging from +18.3 ml/min/1.73 m2 immediately post intervention [19] to +10 6 years later [15]. The largest improvement seen was +23 ml/min/1.73 m2 at 2 years (n = 7) [1].
No studies observing patients receiving PTA alone recorded GFR as an outcome. The remaining five studies include cohorts who received PTA with or without stenting who were considered as a single ‘intervention group’ (n = 101). These all demonstrate an improvement in GFR, ranging from +9.6 ml/min/1.73 m2 post intervention (n = 17) [32] to +19.4 ml/min/1.73 m2 at 5 years (n = 44) [25].
In one study, not baseline measurements were disclosed and GFR change could therefore no be calculated. On a whole, following intervention, an improvement in GFR was demonstrated in all eleven studies averaging +8.6 at three months post-intervention (n = 71), +16.9 ml/min/1.73 m2 at 1 year (n = 85) and +21.1 ml/min/1.73 m2 at 2 years (n = 64) (Table 3).
There was a wide variation in the frequency at which GFR was measured pre and post-intervention, with no two studies recording results with a similar frequency or duration. In papers where a single follow up measurement was taken, studies compared GFR pre-intervention with recordings 1 month [14], 3 months [5], 6 months [23] post-intervention. Others recorded GFR with greater frequency, ranging from at baseline, 3 months, 1 and 2 years [1], to pre-intervention, immediately post-intervention, then at 3, 6, 9, 12, 18, 24 and 30 months post intervention [27]. The length of follow up ranged from measurements taken immediately post-procedure, to 6 years.
Creatinine
Twenty-eight studies (88 %) recorded creatinine as an outcome measure (n = 779). These include seven studies comprising patients receiving PTA only (n = 137) [7–13] and eight studies in patients receiving stents with or without pre-balloon dilatation (n = 141). The remaining 13 studies included both patients following PTA and stenting, who were followed up as a single mixed cohort where outcomes could not be differentiated (n = 501).
The seven studies comprising PTA only patients all demonstrated an improvement in creatinine levels following intervention. Reductions were seen of 80 µmol/L at 1 week (n = 17) [8], 25 µmol/L at 1 month (n = 26) [7], and 31 µmol/L at 6 months (n = 22) [10]. One study did not disclose baseline measurements and a calculation of change post-ntervention could therefore not be made, although yearly measurements between 1 and 3 years did demonstrate an improvement [11]. One study calculated creatinine clearance and demonstrated an improvement of 10.7 ml/min/1.73 m2 at 30–60 days post intervention (n = 10) [12]. The final study [13] reported a 15 % reduction in creatinine in six patients at 6 months and eight patients at 1 year, although no crude measurements were given.
Similarly, the eight studies comprising stented patients only (n = 141) all demonstrated an improvement in creatinine following stenting. An average creatinine reduction of 22.8 µmol/L was seen at 1 month (n = 38) and 88.3 at 1 year (n = 39). The largest reduction of 202 µmol/L was seen at 2 years in one study (n = 13) [2]. Four further studies demonstrated an improvement “post-procedure” of 0.8, 33, 52 and 132 µmol/L [3, 19, 24, 31, respectively] but did not disclose the time period following intervention that the measurements were taken.
All 28 studies demonstrated an improvement in creatinine following intervention with PTA or stenting for TRAS. Allowing for heterogeneity of the study populations, pooled analysis demonstrates a reduction of 42.5 µmol/L at 1 month (n = 302), 72.6 µmol/L at 6 months (n = 274), 79.7 µmol/L at 1 year (n = 239) and 42.1 at 3 years post-intervention (n = 128).
Four studies took measurements pre and 1 month post-intervention [7, 14, 22, 24]. Two studies recorded creatinine at baseline, then at 1 and 6 months post-intervention [3, 26]. The remainder of papers varied widely in their approach to recording creatinine. The shortest period of follow up was 1 week [8], whilst another study studied creatinine levels for up to 6 years [15]. In terms of the most frequently assessed subjects, one took 9 measurements over a 30 month period [27]. Five papers referred to measurements taken pre- and post-procedure but failed to state the length of time either before or after [12, 18, 20, 21, 29] (Table 3).
Blood Pressure
Blood pressure (BP) was measured as an outcome in 26 studies (81 %). Twenty papers (63 %) recorded systolic and diastolic blood pressure (SBP and DBP), whilst 6 papers (19 %) calculated the mean arterial blood pressure (MABP). For the purposes of pooled analysis, all blood pressure recordings have been converted to MAP using the equation [(2 × DBP) + SBP]/3].
Of the 26 studies, 5 were in patients who received PTA only as treatment for TRAS (n = 88) whilst 10 were in patients who had received stenting with or without pre-dilatation (n = 185). The remaining 11 studies included both patients following PTA and stenting, who were followed up as a single mixed cohort where outcomes could not be differentiated (n = 445).
The five studies in PTA only patients all demonstrated an improvement in blood pressure readings following angioplasty. This ranged between a reduction in MAP of 9.6 mmHg at 1 month (n = 26) [7] to a reduction of 25 mmHg at 12 months (n = 20) [9]. One study calculated the ‘mean BP standard deviation score’ and saw a reduction from 3.2 pre-intervention to 1.04 post, although no time frame was disclosed. One study failed to disclose baseline measurements, although serial measurements at 1, 2 and 3 years demonstrated a reduction from 112.7 mmHg to 109.7 mmHg to 103.3 mmHg (n = 15) [11]. The final study [8] did not disclose figures but stated all but one patient had a substantial improvement in mean DBP (n = 17).
Nine of the ten studies in stented patients demonstrated an improvement in blood pressure following intervention. In studies reporting outcomes at 1 month, the average reduction in MAP was 14.9 mmHg (n = 50). At 1 year the average seen was 17.5 mmHg (n = 57). The largest reported improvement was 23.3 mmHg (MAP) at 1 year in a cohort of 18 patients receiving stent only as treatment for TRAS [6]. The one study which failed to demonstrate an improvement did not disclose baseline measurements but recorded BP at 1 year of 129(± 4)/79(± 3) and 131(± 3)/79(± 2) at 3 years in a cohort of 26 patients all receiving stenting with pre-dilatation.
Twenty four of 26 studies demonstrated a reduction in blood pressure following intervention with either PTA or stenting for TRAS. Pooled analysis of all studies demonstrates an average reduction in MAP of 12 mmHg at 1 month (n = 283), 13.4 mmHg at 1 year (n = 402) and 17.5 mmHg over 1 year (n = 171).
Where SBP and DBP were recorded, there was a wide variation in the frequency and length of follow up. Three studies reported measurements taken pre-intervention and 1 month afterwards [7, 14, 22]. In two studies, measurements were taken pre-intervention, then 1 and 12 months post-intervention [6, 28]. Of the remaining studies, no two studies shared a common follow up schedule, ranging from pre-intervention and 1 week post-intervention [8], to 24–48 h pre- and post-intervention, then monthly for up to 6 years [15]. Four studies stated measurements were taken pre- and post-intervention but failed to disclose time periods [13, 20, 21, 29] (Table 3).
In the six studies reporting MABP, no two shared a common schedule, with follow up ranging from 2 months [33] to 3 years [19, 30]. One study recorded MABP pre- and post-intervention at varying time points between their subjects [18].
Anti-Hypertensive Medications
Twenty-six studies (81 %) recorded the number of anti-hypertensive medications taken by subjects prior to and after intervention as an outcome measure (n = 743). Of these, six studies were in patients receiving PTA only as treatment for TRAS (n = 120), whilst eight studies included patients receiving stenting with or without pre-dilatation (n = 160). The remaining 12 studies included both patients following PTA and/or stenting who were followed up as a single mixed cohort (n = 463).
Of the six studies in patients receiving PTA only as treatment, one study demonstrated a reduction in anti-hypertensive therapy of one medication following intervention in a cohort of 20 patients, although no timescale post intervention was disclosed [9]. Smaller reductions were seen in two further studies which demonstrated a reduction of 0.3 at 1 month (n = 26) [7] and by 0.75 at 6 months (n = 15) [10]. One study failed to disclose baseline measurements, therefore a calculation of change following intervention could not be made [11]. One study calculated an ‘Anti-hypertensive score’ pre-intervention but failed to disclose scores post-intervention for comparison [12]. One study reported a decrease in number of anti-hypertensives in 10 patients whilst observing an increase in two, however, no timescale was disclosed [13].
Seven of the eight studies in patients receiving stents as primary treatment for TRAS demonstrated some decrease in the number of anti-hypertensive medications following intervention. These included reductions of 0.5 “at the most recent follow up” (n = 12) [2], 0.4 “following stenting” (no time disclosed) (n = 13) [18], 0.6 post-intervention (no time disclosed) (n = 30) [20], 2 at the “end of observation” (no time disclosed) (n = 26) [17] and 2 at mean 28.3 months (n = 17) [21]. The largest decrease of 2.05 at 6 years post-intervention was seen in a cohort of 18 patients [15]. The only study not to record an improvement declared “no significant change” in the number of medications following treatment (n = 18) [6].
Follow up ranged from the number of anti-hypertensives taken recorded pre- and 1 month post-intervention in four papers [3, 7, 14, 24], to pre-intervention, then at 3, 6, 9, 12, 18, 24 and 30 months post intervention [27]. The longest follow up was up to 6 years in one study [15] (Table 3).
Periprocedural Outcomes and Re-Intervention
Technical Success
Technical success rates were reported in 23 studies (72 %), however, a definition for technical success was provided in only 11 cases. There was a wide variation in what was considered to constitute a technical success. Table 4 lists the definitions of technical success where provided.
Allowing for variability in its definition, pooled analysis demonstrates an overall average technical success rate of 93.7 % across the 23 studies disclosing a technical success rate following intervention by means of PTA and/or stenting for treatment of TRAS (n = 555). In the five studies in patients treated with PTA only, the average technical success rate of 93.1 % (80–96.3 %) (n = 102). In the 11 studies in patients receiving stents as primary treatment (n = 201) the average technical success rate was 97.3 % (83.3–100 %), with eight such studies recording a technical success rate of 100 % (Table 7).
Clinical Success
Clinical success was less widely defined, being reported in only six studies (19 %). Table 5 lists the definitions for clinical success where provided. Clinical success rates were in the range from 65.5 to 94 %. Of the six studies reporting clinical success following intervention, five recorded a success rate of 75 % or higher (Table 5).
Allowing for variability in the definition of clinical success, the two studies in patients treated with PTA only (n = 44) demonstrated an average clinical success rate of 78.9 %. No studies involving patients treated by stenting as a primary intervention recorded clinical success.
The overall clinical success rate was 76.7 %, including studies in which PTA and stented patients were grouped as a single cohort (n = 191).
Patency Rate
Long term patency rates following either PTA or stenting were recorded in 24 (75 %) studies, however, only five studies attempted to define what was considered to be a patent graft or stent, with the remaining 18 studies failing to define what constituted restenosis. Table 6 lists the definitions for patency where provided. Post-procedural follow up of renal artery/stent patency varied widely, with two studies documenting patency only immediately after intervention [18, 26], whilst one study followed patients up for up to 146 months [29].
Of the 25 studies which recorded patency rates following intervention, 5 involved patients receiving PTA only as treatment for TRAS (n = 102) [7, 8, 10, 12, 13], with a further two with mixed PTA/stenting treatment arms which disclosed separate patency rates for the PTA (n = 28) and stenting groups (n = 118) [31, 33). Patency rates were in the range from 42 % at 45 months [31] to 100 % at a median 4.1 years [12]. Allowing for variability in definition of patency rate and follow up time, the overall average patency rate across PTA patients was 73 % (n = 130).
Nine studies recording patency rates involved patients receiving stenting as the primary intervention for TRAS (n = 176) [1, 2, 6, 15–17, 19–21], with a further two with mixed PTA/stenting treatment arms which disclosed separate patency rates for the stenting (n = 118) and PTA groups [31, 33]. Patency rates were in the range from 77.8 % (n = 18, no time of follow-up disclosed) [6] to 100 % in four studies, two of which were at 3 years post intervention [1, 2, 17, 19]. Allowing for variation in definition of patency rate and follow up time, the overall average patency rate across stented patients was 90.4 % (n = 294).
Across all studies which recorded patency rate following intervention for TRAS, allowing for variation in definition of patency, the rate at 1 year was 83.6 % (n = 525) (Table 7).
Secondary patency was recorded in one study of 17 patients receiving PTA only as treatment for TRAS who found a re-intervention rate of 13 % with a secondary patency rate of 50 % (one of two patients represented with recurrent stenosis) [8].
Re-Intervention Rates
Twenty-two studies recorded re-intervention rates following intervention for TRAS. As seen with the measurement of patency rate above, there was a wide variation in follow up time following treatment. The longest period of follow up seen was 5 years in two studies [5, 21].
Allowing for this variation, the overall re-intervention rate across all studies was 14.7 % (n = 623). Of the eight studies evaluating patients following PTA only [7, 8, 10, 12, 13, 28, 31, 33], the average re-intervention rate was 18.9 % (n = 209). Of the 11 studies documenting re-intervention rates following treatment by means of stenting [1, 2, 6, 20, 23, 25, 27–29, 32, 33], the average re-intervention rate was 9.1 % (n = 289). Of these, 5 studies recorded a re-intervention rate of zero (n = 87) [1, 17, 19, 21, 31] (Table 7).
Complications
Twenty-six studies disclosed peri-procedural complications. However, only three papers provided definitions or criteria for their reported complications [14, 15, 31]. Two papers defined complications according to severity, assessing events as major or minor [22, 23].
Seventy-five complications were recorded in total across the 26 studies (n = 760), giving a global complication rate of 9.9 %. Of the 75 total complications recorded, the most frequently observed was vessel dissection, reported in 19 cases, thus constituting 25 % of the overall complications. Fifteen puncture site haematomas and 14 vessel thromboses were reported, constituting 20 and 18.7 % of the complications reported, respectively. Other complications reported included 10 malpositioned/migrated stents (13.3 %), 8 pseudoaneurysms (10.7 %), one iliac artery rupture and one stent occlusion. Two PTA procedures were listed as unsuccessful or failed, constituting 2.7 % of the complications. Of these, one was a patient in whom a double stenosis was found whereby only one vessel was amenable to angioplasty where thrombosis of the non-angioplasted kidney was proven on subsequent arteriography [29]. In the final case the authors did not to elaborate beyond reporting that one patient required vascular reconstruction due to unsuccessful PTA [10]. One study reported three cases of nephrotoxicity, constituting 4 % of the complications, one leading to graft loss [30]. The final two complications included one patient requiring vascular oversewing at the site of arterial puncture site and one listed as allograft loss [20] (Table 8).
Of the four studies concerning patients following PTA only (n = 85), there were five reported complications, giving an overall complication rate of 5.9 %. The complications listed were renal artery thrombosis (2), dissection (2) and one unsuccessful PTA resulting in vascular reconstruction.
Of the nine studies concerning patients following stenting only (n = 173), there were nine reported complications, giving an overall complication rate of 5.2 %. The complications listed were puncture site haematoma (5), stent migration (2) and pseudoaneurysm (2) (Table 8).
Discussion
This systematic review demonstrates percutaneous intervention with transluminal angioplasty (PTA) or endoluminal stenting to be effective in the treatment of TRAS. The current body of evidence supports the use of angioplasty and/or stenting, with favourable outcome in terms of technical success, clinical success and long term patency, with few reported serious complications. However, there is a distinct lack of robust well-designed studies, with no randomised controlled trials and preponderance towards retrospective single-arm cohort studies, although we accept that this may, in part, be due to the low overall incidence of TRAS which may limit the feasibility of large randomised trials. The positive findings are in contrast to those found in the treatment of native renal artery stenosis, where the clinical benefit from revascularization [34] or stenting [35] in patients with atherosclerotic renovascular disease has been widely debated [36] (Table 9).
Approaches to the diagnostic assessment of TRAS varied widely, with a number of combinations of Doppler ultrasound, MR angiography (MRA) and digital subtraction angiography (DSA) techniques employed. The use of Doppler ultrasonography in assessing TRAS is well established with a reported sensitivity of 90–100 % and a specificity of 87–100 % [37]. Catheter angiography, however, remains accepted as the ‘gold standard’ investigation in determining TRAS, whilst the use of ultrasound, CTA and/or MRA has been advocated in the setting of screening for disease.
The heterogeneity of patients was compounded by the large degree of heterogeneity in the definition of TRAS. Where disclosed, studies using MRA or DSA were consistent in defining TRAS as >50 % stenosis. However, in the 25 studies using Doppler ultrasound, three different PSV levels (>2, >2.2 and >2.5 m/s) were used to define TRAS. This may have introduced bias to patient selection, as those with less severe, albeit relevant, TRAS, which may have demonstrated significant stenosis on angiography, may have been overlooked on the basis of Doppler criteria set to detect only severe stenoses.
The majority of interventions performed were angioplasty alone, seen in around half of cases, with stents deployed in 37 % of patients, either in combination with angioplasty, or alone. Nearly half of studies failed to disclose the technique in performing angioplasty. Where the technique was documented, a Seldinger DSA was standard. In studies including subjects receiving angioplasty and/or stenting, justification of stent deployment was poorly documented. Where reasoning was given, the most common indication for stenting was failed PTA, namely due to residual stenosis or the presence of a flow limiting dissection flap. This patient subgroup may represent disease intrinsically more resistant to treatment, thus introducing possible bias to a significant proportion of stented patients.
The lack of disclosure on the stent types used may reflect that the cohort(s) analysed were offered treatment at a time when the use of stents in the management of TRAS was in its infancy meaning several differing products may have been trialled.
Overall, outcomes in terms of GFR, creatinine, blood pressure the number of anti-hypertensive medications have been shown to improve following both treatments. In assessing outcomes, a number of trials including both ‘angioplasty only’ and stented patients considered subjects together as a common ‘intervention group’ in reporting outcomes, as the main objective was not to compare the therapies, but to establish the efficacy of the intervention as a whole. The remaining dataset is too small to allow for any formal pooled analysis to be carried out in order to determine the efficacy of angioplasty against stenting.
Although we have been unable to use meta-analysis due to this inherent study heterogeneity preventing formal pooled analysis, some interesting observations can be made from the available grouped data. When compared to treatment with PTA alone, treatment by means of stenting alone or with pre-balloon dilatation demonstrates superiority in various outcomes including patency rate (73 vs. 90.4 %), re-intervention rate (18.9 vs. 9.1 %) and technical success (93.1 vs. 97.1 %). However, complication rates appear to be comparable between the two groups (5.9 vs. 5.2 %).
In addition to variability in diagnostic techniques, there was an obvious lack of consensus in the recording of outcome measures in the reported literature. While all studies assessed some combination of GFR, creatinine, BP and the number of antihypertensive medications, there was a total lack of concordance in the frequency and length of follow up. Furthermore, technical success was widely reported but definitions varied widely, with five different criteria used in eight studies. Clinical success was similarly also poorly defined. Patency rate was widely reported but very few studies disclosed any criteria for assessing graft patency, with a wide variation in the time of assessment.
A number of peri-procedural complications were recorded with the vast majority undefined. Only two studies referenced the criteria established by the Standards of Practice Committee of the Society of Interventional Radiology. Of the commonly reported complications, puncture site haematoma and puncture site pseudoaneurysm were reported in 8 (25 %) and 6 (19 %) papers, respectively, yet defined in none.
This raises the question of whether a standardised method of recording outcome measures may be of benefit in future studies. The development of “core outcome sets” has been pioneered in rheumatology with the OMERACT (Outcome Measures in Rheumatology) initiative, and more recently been suggested as a method to improve outcome reporting in surgical oncology [38]. A core outcome set is a minimum set of endpoints measured and reported in all studies in a given disease entity. This allows cross-study comparisons for at least the core outcomes to take place. Investigators may add outcomes of particular interest, but always measure and report as a minimum the ‘core set’. In the context of transplant renal artery stenosis, a core outcome set might include short-term clinical outcomes such as creatinine, GFR, BP and antihypertensive therapies, immediate technical success and patency, as well as longer term outcomes such as patency rate at 1 year, and 5 year graft survival rates/mortality.
This review has a number of limitations. The search was limited to studies published after 2000. In addition to potentially excluding important trials, it is possible that standard outcome definitions may have been published prior to this, with the more recently published articles omitting definitions on the assumption of common general knowledge. In the case of serial publications by the same authors, this review considered only the most recent publication. Differing datasets, definitions of TRAS assessment, graft patency and outcome measures previously published may have been omitted from the most recent article. Limiting the inclusion of studies to those published in English may have introduced further selection bias. Lastly, the omission of smaller studies may further compound an already limited dataset.
Conclusion
Whilst current research supports the use of interventional therapy in the treatment of transplant renal artery stenosis, this study demonstrates a lack of standard methodology and inconsistency in the reporting of outcome measures following intervention for TRAS. The introduction of ‘core outcome sets’ may improve this and is recommended to improve data collection in all studies assessing intervention in treatment of TRAS.
The current body of literature demonstrates preponderance towards retrospective cohort studies and this systematic review highlights the requirement for more robust trials and outcome reporting into a multi-centre registry in order to shape future best practice.
Abbreviations
- PTA:
-
Percutaneous transluminal angioplasty
- TRAS:
-
Transplant renal artery stenosis
- DSA:
-
Digital subtraction angiography
- CTA:
-
Computed tomography angiography
- MRA:
-
Magnestic resonance angiography
- GFR:
-
Glomerular filtration rate
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- MAP:
-
Mean arterial pressure
- CMV:
-
Cytomegalovirus
References
Del Pozo M, Martí J, Guirado L, Facundo C, Canal C, de la Torre P, Ballarín J, Díaz JM. Angioplasty and stent treatment of transplant renal artery stenosis. Nefrologia. 2012;32(4):455–8.
Abate MT, Kaur J, Suh H, Darras F, Mani A, Nord EP. The use of drug-eluting stents in the management of transplant renal artery stenosis. Am J Transplant. 2011;11(10):2235–41.
Audard V, Matignon M, Hemery F, Snanoudj R, Desgranges P, Anglade MC, Kobeiter H, Durrbach A, Charpentier B, Lang P, Grimbert P. Risk factors and long-term outcome of transplant renal artery stenosis in adult recipients after treatment by percutaneous transluminal angioplasty. Am J Transplant. 2006;6(1):95–9.
Bruno S, Remuzzi G, Ruggennenti P. Transplant renal artery stenosis. J Am Soc Nephrol. 2004;15:134.
Geddes CC, McManus SK, Koteeswaran S, Baxter GM. Long-term outcome of transplant renal artery stenosis managed conservatively or by radiological intervention. Clin Transplant. 2008;22(5):572–8.
Fluck S, Preston R, McKane W, Harris A, Morgan R, Gedroyc W, Cairns T, Palmer A, Taube D. Intra-arterial stenting for recurrent transplant renal artery stenosis. Transplant Proc. 2001;33(1–2):1245–6.
Halimi JM, Al-Najjar A, Buchler M, Birmelé B, Tranquart F, Alison D, Lebranchu Y. Transplant renal artery stenosis: potential role of ischemia/reperfusion injury and long-term outcome following angioplasty. J Urol. 1999;161(1):28–32.
Patel NH, Jindal RM, Wilkin T, Rose S, Johnson MS, Shah H, Namyslowski J, Moresco KP, Trerotola SO. Renal arterial stenosis in renal allografts: retrospective study of predisposing factors and outcome after percutaneous transluminal angioplasty. Radiology. 2001;219(3):663–7.
Stríbrná J, Schück O, Peregrin JH, Krajícková D, Skibová J. Evaluating the outcome of percutaneous transluminal angioplasty in renal graft artery stenosis using the areas under the time curve of glomerular filtration rate and blood pressure. Physiol Res. 2000;49(6):635–41.
Tang S, Tso WK, Li JH, Li CL, Chan TM, Lai KN. Clinical outcome following percutaneous transluminal angioplasty for transplant renal artery stenoses. Transplant Proc. 2000;32(7):1889–91.
Zupunski A, Buturović-Ponikvar J. Duplex-Doppler long-term follow-up of renal transplant artery stenosis: case controlled study. Ther Apher Dial. 2005;9(3):265–9.
Ghirardo G, De Franceschi M, Vidal E, Vidoni A, Ramondo G, Benetti E, Motta R, Ferraro A, Zanon GF, Miotto D, Murer L. Transplant renal artery stenosis in children: risk factors and outcome after endovascular treatment. Pediatr Nephrol. 2014;29(3):461–7.
Chew LL, Tan BS, Kumar K, Htoo MM, Wong KS, Cheng CW, Teo TK, Irani FG, Choong HL, Tay KH. Percutaneous transluminal angioplasty of transplant renal artery stenosis. Ann Acad Med Singapore. 2014;43(1):39–43.
Bruno S, Ferrari S, Remuzzi G, Ruggenenti P. Doppler ultrasonography in posttransplant renal artery stenosis: a reliable tool for assessing effectiveness of revascularization? Transplantation. 2003;76(1):147–53.
Su CH, Lian JD, Chang HR, Wu SW, Chen SC, Tsai CF, Kao PF, Ueng KC. Long-term outcomes of patients treated with primary stenting for transplant renal artery stenosis: a 10-year case cohort study. World J Surg. 2012;36(1):222–8.
Dimitroulis D, Bokos J, Zavos G, Nikiteas N, Karidis NP, Katsaronis P, Kostakis A. Vascular complications in renal transplantation: a single-center experience in 1367 renal transplantations and review of the literature. Transplant Proc. 2009;41(5):1609–14.
Polytimi L, Sofia G, Paris P. Close to transplant renal artery stenosis and percutaneous transluminal treatment. J Transplant. 2011;2011:219109.
Ridgway D, White SA, Nixon M, Carr S, Blanchard K, Nicholson ML. Primary endoluminal stenting of transplant renal artery stenosis from cadaver and non-heart-beating donor kidneys. Clin Transplant. 2006;20(3):394–400.
Salvadori M, Di Maria L, Rosati A, Larti A, Piperno R, Becherelli P, Bandini S, Biagini M, Filocamo MT, Gallo M, Bertoni E. Efficacy and safety of Palmaz stent implantation in the treatment of renal artery stenosis in renal transplantation. Transplant Proc. 2005;37(2):1047–8.
Valpreda S, Messina M, Rabbia C. Stenting of transplant renal artery stenosis: outcome in a single center study. J Cardiovasc Surg (Torino). 2008;49(5):565–70.
Guzzardi G, Fossaceca R, Di Gesù I, Cerini P, Di Terlizzi M, Stanca C, Malatesta E, Moniaci D, Brustia P, Stratta P, Carriero A. Endovascular treatment of transplanted renal artery stenosis with PTA/stenting. Radiol Med. 2013;118(5):826–36.
Beecroft JR, Rajan DK, Clark TW, Robinette M, Stavropoulos SW. Transplant renal artery stenosis: outcome after percutaneous intervention. J Vasc Interv Radiol. 2004;15(12):1407–13.
Chow KM, Szeto CC, Lee PS, Ho SS, Leung CB, Li PK. Revascularization for post-transplant renal artery stenosis. Nephrology (Carlton). 2007;12(4):406–12.
da Silva RG, Lima VC, Amorim JE, Machado PG, Pacheco-Silva A, Medina-Pestana JO. Angioplasty with stent is the preferred therapy for posttransplant renal artery stenosis. Transplant Proc. 2002;34(2):514–5.
Ghazanfar A, Tavakoli A, Augustine T, Pararajasingam R, Riad H, Chalmers N. Management of transplant renal artery stenosis and its impact on long-term allograft survival: a single-centre experience. Nephrol Dial Transplant. 2011;26(1):336–43.
Hagen G, Wadström J, Magnusson M, Magnusson A. Outcome after percutaneous transluminal angioplasty of arterial stenosis in renal transplant patients. Acta Radiol. 2009;50(3):270–5.
Henning BF, Kuchlbauer S, Böger CA, Obed A, Farkas S, Zülke C, Scherer MN, Walberer A, Banas M, Krüger B, Schlitt HJ, Banas B, Krämer BK. Percutaneous transluminal angioplasty as first-line treatment of transplant renal artery stenosis. Clin Nephrol. 2009;71(5):543–9.
Marini M, Fernandez-Rivera C, Cao I, Gulias D, Alonso A, Lopez-Muñiz A, Gómez-Martínez P. Treatment of transplant renal artery stenosis by percutaneous transluminal angioplasty and/or stenting: study in 63 patients in a single institution. Transplant Proc. 2011;43(6):2205–7.
Marques M, Prats D, Sánchez-Fuctuoso A, Naranjo P, Herrero JA, Contreras E, Barrientos A. Incidence of renal artery stenosis in pediatric en bloc and adult single kidney transplants. Transplantation. 2001;71(1):164–6.
Peregrin JH, Stríbrná J, Lácha J, Skibová J. Long-term follow-up of renal transplant patients with renal artery stenosis treated by percutaneous angioplasty. Eur J Radiol. 2008;66(3):512–8.
Voiculescu A, Schmitz M, Hollenbeck M, Braasch S, Luther B, Sandmann W, Jung G, Mödder U, Grabensee B. Management of arterial stenosis affecting kidney graft perfusion: a single-centre study in 53 patients. Am J Transplant. 2005;5(7):1731–8.
Touma J, Costanzo A, Boura B, Alomran F, Combes M. Endovascular management of transplant renal artery stenosis. J Vasc Surg. 2014;59(4):1058–65. doi:10.1016/j.jvs.2013.10.072 Epub 2013 Dec 22.
Willicombe M, Sandhu B, Brookes P, Gedroyc W, Hakim N, Hamady M, Hill P, McLean A, Moser S, Papalois V, Tait P, Wilcock M, Taube D. Postanastomotic Transplant Renal Artery Stenosis: association With De Novo Class II Donor-Specific Antibodies. Am J Transplant. 2014;14:133–43.
ASTRAL Investigators, Wheatley K, Ives N, Gray R, Kalra PA, Moss JG, Baigent C, Carr S, Chalmers N, Eadington D, Hamilton G, Lipkin G, Nicholson A, Scoble J. Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med. 2009;361(20):1953–62.
Cooper CJ, Murphy TP, Cutlip DE, Jamerson K, Henrich W, Reid DM, Cohen DJ, Matsumoto AH, Steffes M, Jaff MR, Prince MR, Lewis EF, Tuttle KR, Shapiro JI, Rundback JH, Massaro JM, D’Agostino RB Sr, Dworkin LD, CORAL Investigators. Stenting and medical therapy for atherosclerotic renal-artery stenosis. N Engl J Med. 2014;370(1):13–22.
Sarac TP. Influence and critique of the ASTRAL and CORAL Trials. Semin Vasc Surg. 2011;24(3):162–6.
Glicklich D, Tellis VA, Quinn T, et al. Comparison of captopril scan and Doppler ultrasonography as screening tests for transplant renal artery stenosis. Transplantations. 1990;49:217–9.
Blencowe NS, Strong S, McNair AG, Brookes ST, Crosby T, Griffin SM, Blazeby JM. Reporting of short-term clinical outcomes after esophagectomy: a systematic review. Ann Surg. 2012;255(4):658–66.
Conflict of interest
The authors wish to declare no disclosures or conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ngo, A.T., Markar, S.R., De Lijster, M.S. et al. A Systematic Review of Outcomes Following Percutaneous Transluminal Angioplasty and Stenting in the Treatment of Transplant Renal Artery Stenosis. Cardiovasc Intervent Radiol 38, 1573–1588 (2015). https://doi.org/10.1007/s00270-015-1134-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-015-1134-z