Abstract
Purpose
Mechanical thrombectomy (mTE) proved to be effective treating acute vessel occlusions with an acceptable rate of procedural complications. Potential long-term side effects of the vessel wall trauma caused by mechanical irritation of the endothelium are unknown up to now.
Methods
From a retrospectively established database of 640 acute stroke treatments, we selected 261 patients with 265 embolic vessel occlusions treated successfully by mTE without permanent implantation of a stent. Analysis comprised the type of devices used and the number of passes performed. Digital subtraction angiography immediately after treatment was evaluated for vasospasm, dissection, and extravasation. Control angiographic images were evaluated for any morphological change compared to the immediate posttreatment angiographic run.
Results
Recanalization was achieved with a median of one (range 1–10) mTE maneuvers. Vasospasm occurred in 69 territories (26.0 %) and was treated with glyceroltrinitrate in three. Dissection was observed in one vessel (0.4 %). Intraprocedural hemorrhage in two patients (0.8 %) was either wire or device induced. Follow-up digital subtraction angiography was available for 117 territories after a median of 107 days, revealing target vessel occlusion in one segment (0.9 %) and a de novo stenosis of four segments (3.4 %). All findings were clinically asymptomatic. Posttreatment vasospasm was more frequent in patients with de novo stenosis and occlusion (p = 0.038).
Conclusion
De novo stenoses and occlusions occur in a small proportion of patients after mTE. Because all lesions were clinically asymptomatic, this finding does not affect the overall benefit of the treatment. Vasospasm may predict late vessel wall changes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
No more than 15 % of all patients with acute ischemic stroke fulfill the inclusion criteria for intravenous thrombolysis (IVT), leaving a high proportion of severely affected patients without specific therapy. Despite a measurable positive impact of IVT on patient outcome, the overall results remain sobering [1, 2]. Numbers needed to treat for benefit range from 3.6 to 6.1, depending on the time from symptom onset to start of IVT [3, 4]. Especially in proximal large vessel occlusions with high thrombus load, recanalization rates are low [5, 6]. Local intraarterial fibrinolysis seems to add some clinical benefit but still leaves room for fundamental improvement in patient outcome [7].
The next step toward a more effective acute stroke treatment is endovascular mechanical recanalization. The search for the ideal mechanical method for rapid revascularization yielded several devices [8–11]. None of these clot retrievers, however, was able to fully satisfy clinical expectations. The breakthrough came with the incidental observation that the SolitaireAB stent (Covidien/ev3, Irvine, CA, USA) could be used for mechanical thrombectomy (mTE) with high levels of safety and efficacy [12]. Inspired by the obvious success of this concept and device, several derivates were developed. Currently used in clinical practice are SolitaireFR (Covidien/ev3), Trevo Pro 4 (Stryker, Kalamazoo, MI, USA), ReVive (Codman and Shurtleff Inc., Raynham, MA, USA), Capture (MindFrame Inc., Irvine, CA, USA), Aperio (Acandis, Pforzheim, Germany), 3 D Separator (Penumbra Inc., Alameda, CA, USA), and pREset (Phenox, Bochum, Germany).
In the meantime, several studies have been published promising angiographic and clinical results with mTE in acute ischemic stroke [13–15]. To date, reports on mTE are focused on recanalization rates and clinical outcome, and are mostly based on small series. Little is known about the safety margins of mTE under real-world conditions. There is uncertainty whether mTE devices that expose the endothelium to high radial forces cause damage to the wall of target vessels, leading to long-term side effects. Therefore, we offered follow-up digital subtraction angiography after mTE to all eligible patients to exclude delayed and potentially harmful morphological changes of the target vessel.
Material and Methods
Ethical Adherence
This is a retrospective analysis of clinical cases. In our daily routine, decisions about endovascular treatment were made individually on the basis of the assumed prognosis with standard treatment alone. Each case was discussed with the referring neurologist. Informed consent was obtained from conscious patients. If informed consent could not be obtained, we acted according to the assumed will of the patient after discussion with relatives. Control angiography was part of our routine follow-up protocol after mTE to exclude potentially harmful vessel wall changes. Informed consent for control angiography was obtained from each patient.
Retrospective data analysis was approved by the local review board.
Patient Selection
Our hospital is a large tertiary referral center for neurointerventions providing service for 13 regional stroke units on a 24/7 basis. Between January 2008 and May 2012, we performed 640 endovascular recanalization procedures in the setting of acute stroke. This number represents 3 % of all patients treated for ischemic stroke in the 13 referring hospitals.
Because our main purpose was to evaluate long-term effects of mTE devices, we selected cases of intracranial embolic vessel occlusion that were successfully recanalized by mTE alone without supportive balloon dilatation or permanent implantation of a stent. Successful recanalization was defined as a thrombolysis in cerebral infarction score of 2b or 3. Additional intraarterial thrombolysis or stent angioplasty of proximal stenoses in the access site did not result in exclusion of a case.
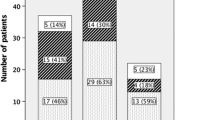
Application of the predefined criteria led to exclusion of 379 patients. Baseline clinical data of the remaining 261 cases are summarized in Table 1. Follow-up modified Rankin scores were collected either during control angiography or by telephone interview after 3–6 months. Data were available for 251 patients. The distribution of modified Rankin scores is summarized in Fig. 1.
Treatment Protocol
Patients referred for mechanical recanalization had an acute onset of clinical symptoms caused by cerebral ischemia and a relevant neurological deficit (National Institutes of Health Stroke Scale score ≥4). We also considered patients with minor but fluctuating or progressive symptoms and large vessel occlusion for endovascular treatment. This subgroup is known to be at significantly higher risk for clinical deterioration and poor outcome despite minor symptoms at presentation [16, 17]. Intracranial hemorrhage was excluded by CT or MRI, and large vessel occlusion was confirmed by CT or MRI angiography. Because patients were referred from several hospitals, there was no uniform imaging protocol.
Intravenous recombinant tissue plasminogen activator was provided before the procedure in a small subset of patients according to generally accepted inclusion and exclusion criteria for IVT. The referring neurologist decided the additional intravenous treatment. Patients in whom an extracranial stenosis or dissection was identified at imaging, or whose medical history caused us to be suspicious of an underlying stenosis were pretreated with 500 mg aspirin and 600 mg clopidogrel. If a patient did not receive a loading dose but stenting had to be performed, 500 mg aspirin was applied intravenously, followed by 600 mg of clopidogrel via nasogastric tube.
All procedures were performed under general anesthesia by a group of six experienced interventional neuroradiologists. During the induction of general anesthesia, all possible efforts were undertaken to avoid a drop in arterial systolic blood pressure.
A three-vessel diagnostic angiography with whole-head runs of the anterior and posterior circulation was performed before treatment to visualize the extent of leptomeningeal collaterals and to exclude multiple vessel occlusions. For procedures in the anterior circulation, an 8F guiding catheter with or without balloon was used [8F Guider Soft Tip and 8F Merci Balloon Guiding Catheter (both Stryker) and 8F Cello Balloon Guiding Catheter (Covidien/ev3)]. In most cases, an additional intermediate catheter [DAC 0.57-inch (Stryker), ReFlex 0.58-inch (Reverse Medical, Irvine, CA, USA)] was introduced. Posterior circulation access was gained with a 6F guiding catheter (Envoy XB; Codman and Shurtleff Inc.). The occluded vessel segment was catheterized with a 0.021 or 0.027-inch inner diameter microcatheter [Prowler Select Plus, RapidTransit (both Codman and Shurtleff Inc.), Rebar 18, or Rebar 27 (both Covidien/ev3)] with a 0.014-inch micro guide wire [SilverSpeed 14 (Covidien/ev3), Traxcess 14 (Microvention/Terumo, Tustin, CA, USA), and Transend X (Stryker)].
At the discretion of the operator, a device for mTE was chosen. Under fluoroscopy, the mTE device was inserted starting just beyond the level of vessel occlusion and deployed by withdrawal of the microcatheter. After a minimum of 3 min of device incubation, a digital subtraction angiography run was performed to define the length of vessel occlusion. Two milligrams of glyceroltrinitrate (Nitrolingualinfus; Pohl Boskamp, Hohenlockstedt, Germany) were slowly injected intraarterially to avoid vasospasm during device withdrawal. Arterial hypotension was compensated by intravenous injection of cafedrinhydrochlorid/theodrenalinhydrochlorid (Akrinor; AWD Pharma, Radebeul, Germany). Under fluoroscopy, the microcatheter and the deployed thrombectomy device were withdrawn with simultaneous aspiration of the guide or extension catheter, eventually under proximal balloon occlusion. After removal of the device and careful purging of the guide or extension catheter, the result of mTE was assessed angiographically. In case of persistent occlusion or incomplete recanalization, mTE was repeated with the same or another device. After successful restoration of flow, a final angiographic run was performed to exclude distal emboli. If recanalization could not be achieved after several mTE maneuvers, the procedure was either aborted or continued with angioplasty and/or stents. The latter cases were excluded from further analysis. After mTE, the patient was kept sedated and ventilated until the next day to allow precise management of blood pressure tolerating a maximum peak systolic value of 130–150 mm Hg.
In case of stenting, dual antiplatelet medication was continued for 6 weeks up to 1 year (depending on the type of stent), followed by 100 mg aspirin for life. Otherwise, anticoagulation or antiplatelet treatment was administered according to generally accepted neurological guidelines.
Control angiography was scheduled after 3 months or later, depending on the clinical status of the patient to assess the integrity of the recanalized vessels and to exclude stenosis of additionally implanted stents.
Data Evaluation
Pre- and posttreatment angiographic images were assessed for the site of occlusion, target vessels for treatment, and therapy-induced vasospasm, dissection, or extravasation. The number and type of mTE devices and the number of passes performed per vessel segment were recorded.
Follow-up angiographic images of the treated vessel were compared with the posttreatment final run to detect morphological changes including new stenoses, occlusions, or focal ectasia that might have been caused by the mechanical injury.
Statistical Analysis
Statistical analysis was performed with Stata/IC 11.2 for Windows (StataCorp, College Station, TX, USA). To describe the relationship between vasospasm, dissection, and vessel perforation and the number of passes, we calculated odds ratios (OR), 95 % confidence intervals (CI), and p values. Fisher’s exact test was used to analyze the relationship between vasospasm and late vessel wall changes. A p value of ≤0.05 was accepted to be significant.
Results
We defined 265 target territories in 261 patients who were recanalized with a median of one pass (range 1–10 passes). Types and numbers of mTE devices as well as the number of passes per device are summarized in Table 2.
Vasospasm was obvious in 69 vessel territories (26.0 %). Treatment with additional intraarterial glyceroltrinitrate was deemed to be necessary on three occasions (Fig. 2). None of the treated patients exhibited significantly reduced flow in the final angiographic run. One target vessel dissection occurred (0.4 %) and was uneventfully treated with a stent. In addition, we observed two intraprocedural hemorrhages (0.8 %). In one case, contrast leakage stopped after reduction of blood pressure; in the second, the bleeding branch was occluded by glue injection. Ninety-day modified Rankin score was 2 in the first patient and 5 in the second patient. Regarding the cause, it was not possible to discriminate wire perforation and device-associated laceration because no angiographic run was performed between probing and device deployment.
A After mTE of the left middle and anterior cerebral artery territory, a 47-year-old patient developed a flow compromising vasospasm of the left A2 segment (arrow). Irregularities of the M1 and A1 segments indicated moderate spasm there. B After fractionated intraarterial injection of 4 mg glyceroltrinitrate, flow was sufficiently restored in the left A2 segment (arrow)
Statistical analysis did not reveal a significant relationship between the number of mTE passes and vasospasm (OR 1.09, 95 % CI 0.9–1.31, p = 0.394), dissection (OR 1.01, 95 % CI 0.26–3.92, p = 0.985), or vessel perforation (OR 1.64, 95 % CI 0.63–4.27, p = 0.315).
Control angiography was available for 116 patients with 117 target territories. Angiography was performed after a median of 107 days (range 24–524 days). We found one secondary occlusion (0.9 %) of a successfully recanalized vessel. A de novo stenosis of a previously normal vessel was observed in four patients (3.4 %) (Figs. 3, 4). Details of the patients exhibiting de novo stenosis or occlusion are summarized in Table 3. All lesions were clinically asymptomatic. We did not observe any pathological vessel dilatation. Posttreatment vasospasm was more often observed in patients with subsequent stenosis or occlusion (p = 0.038).
A Final angiographic run of a 75-year-old patient (patient 5) revealed a normal caliber of the middle cerebral artery and division branches after recanalization by mTE. B Follow-up angiography after 154 days revealed an asymptomatic high-grade stenosis of the superior M2 branch and a narrowing of the carotid T (arrows)
A Final angiographic run of a 60-year-old patient (patient 2) treated for a left vertebral ostium stenosis with appositional thrombus and embolic occlusion of the left V4 segment demonstrating complete recanalization of the V4 segment with persistent occlusion of the posterior inferior cerebellar artery (PICA). B Follow-up angiography after 222 days revealed an asymptomatic high-grade stenosis at the level of the origin of the left PICA (arrow)
Discussion
The ideal method for endovascular treatment of ischemic stroke with large vessel occlusion would allow recanalization of the occluded vessels within a short period of time (i.e., minutes) without interference with the coagulation system and without a need for supportive anticoagulation, antiaggregation, or fibrinolysis; without damage to the occluded vessel; without fragmentation of the thrombus; and relying on a reasonable level of technical skills of the trained operator. Most of these requirements are well addressed by mTE, which has been demonstrated to be superior to local intraarterial fibrinolysis [18].
The potential damage to the vessel wall, which is one of the safety aspects of mTE, has been evaluated in animal models [19]. Vasospasm of swine renal arteries was a frequent observation after deployment of the SolitaireFR device, but permanent vessel laceration after stent retrieval did not occur. No stenosis was found during follow-up. Delayed hyperplasia of the intima layer was only visible on histology specimens in animals that had been killed, and had no hemodynamic effect. Mordasini et al. [20] published similar results and did not observe any device-related complications in their experiments. The Trevo stentlike retriever was also evaluated in preclinical animal studies, including histological analysis immediately after thrombectomy [21]. Vasospasm occurred frequently, but no vessel wall damage was obvious in angiographic runs. Histologic examination revealed severe disruption of the intima without affection of the media and adventitia layers.
Our observation of a low acute device-related complication rate after mTE is in line with the results of published animal experiments and clinical case series. Machi et al. [14] observed mechanically induced vasospasm in 32 % of patients after Solitaire mTE, without further adverse effects. Vasospasm was also described after mTE with the Merci and Catch device [9, 22] and does not seem to be confined to stent retrievers. mTE-induced vasospasm can effectively be prevented by intraarterial injection of glyceroltrinitrate after deployment of the device and before removal. This may also help to avoid vessel dissection and could possibly increase the efficacy of the mTE process. An incubation time of several minutes may act similarly. If significant vasospasm occurs despite all precautions, it can be treated by application of additional vasodilating drugs. We used intraarterial glyceroltrinitrate as a vasodilating agent because of its immediate effect. Other interventionalists prefer nimodipine either as a continuos infusion during the intervention or on demand. Comparative studies regarding the optimal drug and the ideal way of administration have not been performed.
Dissection of the arterial wall after mTE seems to be rare but was reported after use of the Merci device [23, 24]. The only dissection in our case series was uneventfully treated by stent placement and did not lead to clinical deterioration. Two intraprocedural hemorrhages were observed, but the cause could not be precisely attributed to either the guide wire or the mTE device. This is a serious adverse event that requires immediate reduction of blood pressure and reversal of heparin. In cases of non-self-limiting severe hemorrhage, occlusion of the bleeding vessel has to be considered. Depending on vessel size, it can be done by glue injection—as in our case—or by coiling. More diffuse hemorrhages may be treated by temporary balloon occlusion. Clinical outcome after intraprocedural hemorrhage varies depending on the amount of extravasation and the location of hemorrhage. Statistical analyses did not reveal a relationship between the number of thrombectomy passes, dissection, and intraprocedural hemorrhage. In cases of dissection and hemorrhage, the number of events was low, which increases the chance of a type II error.
During follow-up, we found de novo stenoses as well as target vessel occlusion with an incidence of 3.4 and 0.9 %, respectively. The lesions observed in this study were, without exception, asymptomatic. The most likely mechanism of stenosis formation after mTE is mechanically induced endothelial trauma or microdissection. In an animal model, Nogueira et al. [21] proved intima disruption after mTE histologically that was not visible angiographically. These endothelial microtrauma are likely to occur in human species also and may induce significant intima hyperplasia in a small subset of patients.
Vasospasm was more frequent in patients with subsequent vessel wall changes. Two hypotheses may serve as an explanation. Vessel constriction could be an indicator for the degree of mechanical irritation, with more severe trauma inducing enhanced intima hyperplasia. Because observations from other endovascular procedures demonstrate that the frequency of vasospasm varies between individuals, development of vasospasm might also reflect a genetically determined higher vulnerability of the vessel wall.
The limitations of this study are both methodological and conceptional. This is a retrospective analysis. We included a variety of devices, which have different radial forces and designs. For some devices, the number of treatments was low, which affects the validity of the study for these retrievers. In addition, it is not certain whether the results of this series apply for all other mTE devices currently available. Modifications in design and radial force may have more impact on the vessel wall. The only method applied for evaluation was digital subtraction angiography, which is able to show the lumen but not the vessel wall itself. Intravascular ultrasound and high-resolution MRI might be able to provide better visualization into vessel wall changes.
In conclusion, mTE of acutely occluded intracranial vessels in ischemic stroke using commercially available devices is well tolerated by the vessel wall in most cases. The likelihood of inducing delayed stenosis or occlusion is low. These risks are overcompensated by the clinical benefits of the procedure. Vasospasm may predict late vessel wall changes.
References
National Institute of Neurological Disorders and Stroke RT-PA Stroke Study Group (1995) Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 333:1581–1587
Hakke W, Kaste M, Bluhmki E et al (2008) Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 359:1317–1329
Lansberg MG, Schrooten M, Bluhmki E et al (2009) Treatment time specific number needed to treat estimates for tissue plasminogen activator therapy in acute stroke based on shifts over the entire range of the modified Rankin scale. Stroke 40:2079–2084
Saver JL, Gornbein J, Grotta J et al (2009) Number needed to treat to benefit and harm for intravenous tissue plasminogen activator therapy in the 3- to 4.5-hour window: joint outcome table analysis of the ECASS 3 trial. Stroke 40:2433–2437
Riedel CH, Zimmermann P, Jensen-Kondering U et al (2011) The importance of size: successful recanalization by intravenous thrombolysis in acute anterior stroke depends on thrombus length. Stroke 42:1775–1777
Saqqur M, Uchino K, Demchuk AM et al (2007) Site of arterial occlusion identified by transcranial Doppler predicts the response to intravenous thrombolysis for stroke. Stroke 38:948–954
Mattle HP, Arnold M, Georgiadis D et al (2008) Comparison of intraarterial and intravenous thrombolysis for ischemic stroke with hyperdense middle cerebal artery sign. Stroke 39:379–383
Smith WS, Sung G, Saver J et al (2008) Mechanical thrombectomy for acute ischemic stroke: final results of the Multi MERCI trial. Stroke 39:1205–1212
Mourand I, Brunel H, Costalat V et al (2011) Mechanical thrombectomy in acute ischemic stroke: catch device. AJNR Am J Neuroradiol 32:1381–1385
Henkes H, Reinartz J, Lowens S et al (2006) A device for fast mechanical clot retrieval from intracranial arteries (Phenox clot retriever). Neurocrit Care 5:134–140
Penumbra Pivotal Stroke Trial Investigators (2009) The penumbra pivotal stroke trial: safety and effectiveness of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke 40:2761–2768
Pérez MA, Miloslavski E, Fischer S et al (2012) Intracranial thrombectomy using the Solitaire stent: a historical vignette. J Neurointerv Surg 4:154
Castaño C, Dorado L, Guerrero C et al (2010) Mechanical thrombectomy with the Solitaire AB device in large artery occlusion of the anterior circulation: a pilot study. Stroke 41:1836–1840
Machi P, Costalat V, Lobotesis K et al (2012) Solitaire FR thrombectomy system: immediate results in 56 consecutive acute ischemic stroke patients. J Neurointerv Surg 4:62–66
Rohde S, Haehnel S, Herweh C et al (2011) Mechanical thrombectomy in acute embolic stroke: preliminary results with the revive device. Stroke 42:2954–2956
Nedeltchev K, Schwengler B, Haefeli T et al (2007) Outcome of stroke with mild or rapidly improving symptoms. Stroke 38:2531–2535
Rajajee V, Kidwell C, Starkman S et al (2006) Early MRI and outcomes of untreated patients with mild or improving ischemic stroke. Neurology 67:980–984
Möhlenbruch M, Seifert M, Okulla T et al (2011) Mechanical thrombectomy compared to local-intraarterial thrombolysis in carotid T and middle cerebral artery occlusions: a single center experience. Clin Neuroradiol. doi:10.1007/s00062-011-0099-9
Jahan R (2010) Solitaire flow-restoration device for treatment of acute ischemic stroke: safety and recanalization efficacy study in a swine vessel occlusion model. AJNR Am J Neuroradiol 31:1938–1943
Mordasini P, Frabetti N, Gralla J et al (2011) In vivo evaluation of the first dedicated combined flow-restoration and mechanical thrombectomy device in a swine model of acute vessel occlusion. AJNR Am J Neuroradiol 32:294–300
Nogueira RG, Levy EI, Gounis M et al (2012) The Trevo device: preclinical data of a novel stroke thrombectomy device in two different animal models of arterial thrombo-occlusive disease. J Neurointerv Surg 4:295–300
Gupta R (2009) Arterial vasospasm during mechanical thrombectomy for acute stroke. J Neuroimaging 19:61–64
Smith WS, Sung G, Starkman S et al (2005) Safety and efficacy of mechanical embolectomy in acute ischemic stroke. Results of the MERCI trial. Stroke 36:1432–1440
Yin NS, Benavides S, Starkman S et al (2010) Autopsy findings after intracranial thrombectomy for acute ischemic stroke—a clinicopathologic study of 5 patients. Stroke 41:938–947
Conflict of interest
W. Kurre is a consultant to Phenox, received travel expenses from Phenox, and received speaker honoraria from Codman and Shurtleff Inc. M. Aguilar-Pérez is a consultant to Phenox. D. Horvath does not have any conflict of interest. E. Schmid received speaker honoraria from Bayer vital. H. Bäzner received speaker honoraria from Bayer vital, UCB Pharma, Biogen Idec and Boehringer Ingelheim. H. Henkes received speaker honoraria as well as travel expenses from Covidien/ev3 and Codman and Shurtleff Inc. He was cofounder of Dendron (the company that developed the Solitaire and was later acquired by ev3) and Phenox (the company that developed the pREset retriever).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kurre, W., Pérez, M.A., Horvath, D. et al. Does Mechanical Thrombectomy in Acute Embolic Stroke Have Long-term Side Effects on Intracranial Vessels? An Angiographic Follow-up Study. Cardiovasc Intervent Radiol 36, 629–636 (2013). https://doi.org/10.1007/s00270-012-0496-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-012-0496-8