Abstract
Purpose
To evaluate the safety and feasibility of percutaneous transsplenic access to the portal vein for management of vascular complication in patients with chronic liver diseases.
Methods
Between Sept 2009 and April 2011, percutaneous transsplenic access to the portal vein was attempted in nine patients with chronic liver disease. Splenic vein puncture was performed under ultrasonographic guidance with a Chiba needle, followed by introduction of a 4 to 9F sheath. Four patients with hematemesis or hematochezia underwent variceal embolization. Another two patients underwent portosystemic shunt embolization in order to improve portal venous blood flow. Portal vein recanalization was attempted in three patients with a transplanted liver. The percutaneous transsplenic access site was closed using coils and glue.
Results
Percutaneous transsplenic splenic vein catheterization was performed successfully in all patients. Gastric or jejunal varix embolization with glue and lipiodol mixture was performed successfully in four patients. In two patients with a massive portosystemic shunt, embolization of the shunting vessel with a vascular plug, microcoils, glue, and lipiodol mixture was achieved successfully. Portal vein recanalization was attempted in three patients with a transplanted liver; however, only one patient was treated successfully. Complete closure of the percutaneous transsplenic tract was achieved using coils and glue without bleeding complication in all patients.
Conclusion
Percutaneous transsplenic access to the portal vein can be an alternative route for portography and further endovascular management in patients for whom conventional approaches are difficult or impossible.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vascular complication, including variceal bleeding, portosystemic shunt, and portal vein thrombosis, is a major cause of mortality and morbidity in patients with chronic liver disease [1]. Once gastric varices bleed, the mortality rate ranges 25–55% [2, 3]. A portosystemic shunt is a bypass of the liver by the systemic circulatory system and may cause deterioration of hepatic function. Portal vein thrombosis is another serious complication, particularly in patients with a transplanted liver, and can result in variceal hemorrhage, sepsis, and graft failure.
These various vascular complications have been treated by transcatheter endovascular treatment, such as a transjugular intrahepatic portosystemic shunt, percutaneous transhepatic embolization, balloon-occluded retrograde transvenous obliteration, and percutaneous endovascular recanalization of portal vein thrombosis [4–9]. In transjugular intrahepatic portosystemic shunt and percutaneous transhepatic embolization, percutaneous or intrahepatic access to the portal venous system is required. Percutaneous transhepatic access and transjugular intrahepatic access to the portal vein are commonly used access techniques [4–8]. Recanalized umbilical vein may also provide vascular access to the portal venous system. Balloon-occluded retrograde transvenous obliteration could be considered for gastric varix embolization; however, it is feasible only in patients with a gastrorenal shunt [9]. However, use of these methods for access to the portal venous system may be difficult or even impossible in patients with hematoma in the perihepatic space, non-visualized intrahepatic portal vein, or total occlusion of the main portal vein.
The percutaneous transsplenic approach is another way to access the portal venous system. Splenoportography was first introduced in 1951, but was soon abandoned as a result of the risk of bleeding from the splenic puncture site [10]. Later, Probst et al. [11] reported on a simple method for prevention of bleeding complications by plugging the splenic tract with a compressed absorbable gelatin sponge. In 1985, Tsang et al. [12] first reported on a case with percutaneous transsplenic catheterization of the splenic vein for balloon dilatation of a stenotic surgical splenorenal shunt. Still, percutaneous transsplenic access to the portal vein has not been widely used and only a few literature reports have supported the safety and effectiveness of this procedure [13–15]. The present study was performed in order to evaluate the safety and feasibility of percutaneous transsplenic access to the portal vein for management of vascular complication in patients with chronic liver diseases.
Materials and Methods
Patients
Between Sept 2009 and April 2011, nine patients (seven men and two women; age range 1–70 years; mean 36 years) with vascular complication related to underlying chronic liver disease were referred to our department for endovascular treatment. Of these patients, four patients underwent variceal embolization in order to stop hematemesis or hematochezia. Two patients underwent portosystemic shunt embolization in order to improve portal venous blood flow. Portal vein recanalization was attempted in three patients with a transplanted liver and occlusion of the main portal vein. The clinical features of the nine patients are summarized in Table 1. The reason for percutaneous transsplenic access were main portal vein occlusion by tumor thrombi in two patients with hepatocellular carcinoma, main portal vein occlusion in three patients with transplanted liver, attenuated intrahepatic portal vein in two patients with native liver, cavernous transformation of the portal vein in one patient with a native liver, and extensive hematoma in the perihepatic space in one patient with a transplanted liver. This study was approved by our institutional review board, and the requirement for informed consent was waived because the study was retrospective.
Techniques
Contrast-enhanced computed tomography (CT) was undertaken to demonstrate the vascular anatomy in all patients prior the procedures. All of the patients underwent percutaneous transsplenic access to the portal venous system. Ultrasonography of the spleen was performed in order to determine the best access route into the splenic vein and portal venous system. Color Doppler was routinely used to discriminate the splenic vein from the splenic artery. Percutaneous transsplenic puncture of the perihilar splenic vein was performed using a 21-gauge Chiba needle (Cook, Bloomington, IN) under ultrasonographic and fluoroscopic guidance. Perihilar splenic vein was punctured because peripheral splenic vein was commonly too thin to be easily accessed. If puncture of the splenic vein failed, a Chiba needle was slightly retracted within the splenic parenchyma and was advanced again to puncture the splenic vein—that is, we punctured the splenic capsule only once because multiple puncture of splenic capsule might cause perisplenic hemorrhage. A 0.018-inch guide wire (Cope Mandril; Cook) was then advanced through the 21-gauge needle within the splenic vein. The 5F Accu-introducer catheter (Sungwon Medical, Seoul, Korea) was advanced over the 0.018-inch guide wire. A 0.035-inch angled hydrophilic guide wire (Terumo, Tokyo, Japan) was advanced through the Accu-introducer catheter. A 4F to 9F sheath (Terumo) was placed over a 0.035-inch guide wire. After placement of the sheath into the splenic vein, each interventional procedure was performed for each patient.
Splenoportography was performed using a 4F to 5F catheter in order to demonstrate vascular complication and to determine a plan for endovascular treatment in all patients. Huge gastric or jejunal varix was noted on splenoportography in four patients with hematemesis or hematochezia. The main afferent vein was selected using a 5F catheter and a 2.4F microcatheter (Microferret, Cook), and venography was obtained. Glue (Histoacryl, B. Braun, Tuttlingen, Germany) and lipiodol mixtures (1:3~1:6 ratio) were used as embolization material for variceal embolization. When the variceal vessels were occluded or the blood flow in varices was very slow, the varices were considered completely embolized. After the sheath was slightly pulled back, the puncture tract of the spleen was first embolized using various coils (standard coil and nester coil, Cook). When the sheath was pulled back to the surface of the spleen, glue and lipiodol mixture (1:2 ratio) were used for embolization of the splenic puncture site.
Portosystemic shunt embolization was performed in two patients. Large draining vein was selected using a 5F catheter and venography was obtained in order to evaluate the size and blood flow of the shunt. An Amplatz vascular plug, microcoils, glue, and lipiodol mixtures were used as embolic material for shunt embolization. Almost near total occlusion with decreased blood flow was demonstrated by postembolization splenoportography. As previously described, the transsplenic tract and the splenic puncture site were embolized by coils, glue, and lipiodol mixture.
Portal vein recanalization was attempted in three patients with a transplanted liver. In one patient, portography confirmed occlusion of the main portal vein and gastric varices. The thrombosed main portal vein was catheterized using a 4F Davis catheter and an angled hydrophilic wire (Terumo). Repetitive aspiration thrombectomy was then performed using a 6F guiding catheter. Balloon angioplasty for stenosis of the main portal vein was performed using a 4-mm balloon (Savvy; Cordis Europa, Roden, The Netherlands). For clearing of residual thrombus, 200,000 units of urokinase was infused through the main portal vein for 1 h. Gastric varix was embolized with glue and lipiodol mixtures in order to improve portal venous blood flow. Finally, portal vein recanalization was achieved in this patient. In the other two patients, recanalization of the main portal vein was attempted; however, the guide wire failed to traverse the occluded main portal vein. As previously described, the transsplenic tract and splenic puncture site were embolized using coils, glue, and lipiodol mixture.
Follow-up
After the procedure, we performed immediate ultrasonography investigation to rule out possible perisplenic hematoma. Contrast-enhanced CT was obtained in order to evaluate the technical success and procedure-related complications (mean time interval, 7 days; interval range : 2–19 days) in all nine patients. Technical success in patients with varix or portosystemic shunt embolization was defined as complete clotting of the varices or shunts as observed on CT images in the portal phase. Patent blood flow through the extrahepatic and intrahepatic portal veins was identified as criteria for technical success in patients with portal vein recanalization. Procedure-related complication, especially bleeding from the spleen, such as intrasplenic hemorrhage or perisplenic hematoma, was confirmed on follow-up CT images.
Results
Under ultrasonography guidance, percutaneous transsplenic access to the portal venous system was performed successfully in all of the patients (100%, 9 of 9). Each interventional procedure was technically successful in seven patients (78%, 7 of 9). Two patients showed failure to traverse the occluded extrahepatic main portal vein. The technical results are summarized in Table 1.
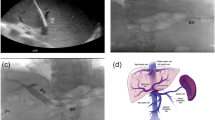
Gastric or jejunal varix embolization with glue and lipiodol mixture was performed successfully in four patients (Fig. 1). Complete obliteration of varices without residual blood flow was noted on follow-up contrast-enhanced CT. In four patients with gastric or jejunal varix embolization, neither recurrent varix formation nor variceal bleeding was observed during the follow-up period. Among the four patients, two patients needed blood transfusion as a result of massive ongoing variceal bleeding form gastrointestinal tract. Two patients (patients 1 and 2) received six units of packed red blood cell (RBC) transfusion before and during the variceal embolization, and took two packed RBC transfusion after the procedure. Only one patient (patient 1) died on the fifth day after the procedure as a result of acute hepatic and renal failure, which was thought to be caused by massive variceal bleeding and transfusion before the procedure.
A 59-year-old man with underlying advanced liver cirrhosis presented with hematochezia and hematemesis. He had undergone eight sessions of chemoembolization for hepatocellular carcinomas. A Transverse contrast-enhanced CT scan of the abdomen demonstrates the gastric varices (arrows) in patient with advanced liver cirrhosis. Note the occlusion of left portal vein by tumor thrombi (arrowheads) and accumulation of iodized oil in the right anterior portal vein (curved arrow). B Transverse contrast-enhanced CT scan of the abdomen shows partial occlusion of the main portal vein by tumor thrombi (arrow). Note enhancement of patent right posterior portal vein (arrowhead). C Initial venography of the splenic and portal veins demonstrates the tortuous and dilated left gastric (white arrow) and posterior gastric veins (white arrowhead). Sengstaken-Blakemore tube (black arrows) was inserted in the stomach for hemostasis of gastric variceal bleeding by balloon tamponade. Note the filling defect (black arrowheads) at main portal vein due to tumor thrombi that was seen on previous contrast-enhanced CT scan of the abdomen. Left portal vein is not seen due to tumor thrombi. D Venography of the splenic and portal veins, after embolization of gastric varices, shows near totally occlusion of left gastric vein (arrows) and posterior gastric vein (arrowheads). E Percutaneous transsplenic tract was embolized by multiple coils (arrow) and glue and lipiodol mixtures (arrowheads). Note glue and lipiodol mixtures in the splenic parenchymal tract, around splenic capsule puncture site, and in the subcutaneous puncture tract
In two patients with large portosystemic shunts, embolization of shunting vessels with a vascular plug, microcoils, glue and lipiodol mixture was achieved successfully. Follow-up CT imaging showed a near totally obliterated shunt by embolic materials or by formation of thrombi.
Portal vein recanalization was attempted in three patients with a transplanted liver; however, only one patient was treated successfully. Failure to traverse the occluded extrahepatic main portal vein by guide-wire and catheter was observed in two patients (patients 7 and 9) who had chronic occlusion (>1 year) of the main portal vein. In the other patient (patient 8) who had acute occlusion (2 days) of the main portal vein, the guide-wire and catheter passed through the thrombosed extrahepatic main portal vein, and, after repeated aspiration, thrombolysis by urokinase and balloon angioplasty was performed. Follow-up CT imaging taken after three weeks showed patent extrahepatic and intrahepatic portal veins without recurrent thrombosis (Fig. 2).
A 1-year-old boy underwent liver transplantation 2 days before due to biliary atresia. Thrombosis of main portal vein was noted on postoperative contrast-enhanced CT scan of the abdomen. A Under ultrasonographic and fluoroscopic guidance, perihilar splenic vein puncture was performed. B Initial venography of the splenic vein showing the occlusion of the main portal vein (X) with massive gastric varices (arrows) and dilated inferior mesenteric vein (arrowheads). C Passing the guide wire through thrombosed main portal vein was successfully achieved. D Venography of the splenic vein, after recanalization of the main portal vein, reveals patent portal vein and decreased collateral vessels
In all nine patients, there was no occurrence of procedure-related complication and perisplenic hematoma on immediate ultrasonography. As seen on follow-up CT imaging, bleeding from the spleen, such as intrasplenic hemorrhage or perisplenic hematoma was not observed in any of the patients. Eight patients survived more than 3 months after the procedure without late complications.
Discussion
Several techniques are available for catheterization in the portal venous system. First, the percutaneous transhepatic approach has been widely adopted by most radiologists. However, passage through a thrombosed segment of the intrahepatic portal vein may be difficult. It can also be difficult in patients with a large amount of ascites or hematoma around the liver. Second, direct catheterization through a mesenteric vein via minilaparotomy is a relatively safe procedure, but much more invasive than the percutaneous technique [16]. Third, the use of a transjugular intrahepatic portosystemic shunt is another method for vascular access to the portal venous system [17]. This method has become an important alternative in management of intractable ascites, acute and chronic variceal hemorrhage, and other complications of portal hypertension. However, the relatively long way to the portal venous system may be disadvantageous for handling of vascular catheters. Fourth, recanalized umbilical vein with blood flow can also provide vascular access to the portal venous system. Use of the percutaneous transumbilical approach for esophageal varix embolization was reported more than two decades ago [18]. In addition, complete chemoembolization of hepatocellular carcinoma fed by the portal vein via a percutaneous transumbilical approach has also been reported [19]. The transumbilical approach has an advantage over the percutaneous transhepatic approach because it can obviate intra-abdominal hemorrhage in a patient with tense ascites [18]. However, a patent umbilical vein with intact blood flow is an aberrant vessel and is not observed in all patients. Fifth, the transsplenic approach provides the straightest pathway for entry into branches of the portal vein and several varices or shunts. However, the very tortuous course of the splenic vein may prevent catheter advancement, and a higher rate of bleeding complications may occur, compared with the transhepatic approach [14, 15, 20]. In this study, we did not encounter any problem resulting from tortuous course of the splenic vein and bleeding complication.
Since the introduction of a simple method for prevention of bleeding complications by plugging the splenic tract with a compressed absorbable gelatin sponge by Probst et al. [11], splenoportography is now accepted as a safe procedure. However, endovascular treatment with percutaneous transsplenic access is still a subject of controversy. Hemorrhage from the splenic puncture site and intrasplenic hematomas should be considered as principal complications in the context of portal hypertension, splenomegaly, and thrombocytopenia [14, 20]. Severe complications after transsplenic portal vein catheterization have been reported. Liang et al. [20] tried percutaneous transsplenic catheterization of the portal venous system in 17 patients. One patient had a 1-cm intrasplenic hematoma at CT 6 days later. In another two patients, CT revealed a 5-cm intrasplenic hematoma in one patient, and a small hemoperitoneum in the other. Because of complaints of dizziness, both patients received one unit of packed RBC transfusion. One patient complained of pain in the left upper quadrant of the abdomen after the procedure. Chest radiography revealed minimal left pleural effusion, which had subsided spontaneously 4 days later. Gong et al. [15] performed percutaneous transsplenic embolization of esophageal and gastriofundal varices in 18 patients. Erythrocyte counts of all patients showed a decrease after the procedure, and five of them required blood transfusion. Two patients experienced hemoperitoneum, and one patient had mild reactive pleural effusion. Two patients died of postprocedural acute liver failure or acute renal failure.
The spleen is a hypervascular organ, communicated with whole parenchymal tissue by complex channels. The principal complication of splenic vein catheterization is hemorrhage from the splenic puncture site and tract; this is more likely in the context of portal hypertension, splenomegaly, and thrombocytopenia. Embolization of the percutaneous transsplenic puncture site with an absorbable gelatin sponge has been well described and is an established technique after vascular access. This method is relatively safe and simple to perform, and the risk of subsequent splenic hemorrhage is low [11]. However, the absorbable gelatin sponge is not a permanent but a transient embolic material. We used permanent embolic materials (coils and glue) for closure of the transsplenic tract and splenic puncture site. After the sheath was slightly pulled back, coils were deployed within the parenchymal puncture tract to prevent massive regurgitation of blood through the puncture tract. Various coils of 0.035 inch diameter were used : standard coils were used in the early study period and nester coils were commonly used in the later study period. The size of coils was determined considering the size of sheath. Glue and lipiodol mixture was injected through the sheath while we removed the sheath, so glue and lipiodol mixture was plastered over the puncture site of splenic capsule. The ratio of glue and lipiodol was determined as 1:2 in volume because we thought fast polymerization of glue would be useful to seal the puncture site off. Neither immediate nor delayed bleeding from the spleen was observed during the follow-up period in all nine patients.
Not only the vascular access route of endovascular treatment, but also splenic biopsy for tissue confirmation is important in modern medicine: splenomegaly and focal splenic lesions may be of primary diagnostic importance and often define the course of treatment in patients with malignancy, risk of metastases, or relapsed hematopoietic disorders. Several methods have been proposed for reduction of postbiopsy bleeding in the abdominal solid organs, including the liver, spleen, and kidney. These methods include plugging the biopsy tract using a hemostatic agent, such as an absorbable gelatin sponge, a coil, fibrin sealants, or a Histoacryl-Lipiodol mixture, and application of radiofrequency energy in order to occlude the biopsy tract [21–24]. Lee et al. [23] demonstrated that a glue-lipiodol mixture, when used as a plug material for the renal biopsy tract, is an efficacious method of bleeding control that is associated with a low incidence of pathological alterations in an anticoagulated rabbit model. The study group of Choi et al. [24] compared radiofrequency cauterization, splenic biopsy tract embolization using an absorbable gelatin sponge, and Histoacryl-Lipiodol mixture plugging as bleeding reduction methods after splenic core biopsy in a dog model. All of the methods were effective for control of postsplenic biopsy bleeding. However, each method showed distinct disadvantages. Histoacryl-Lipiodol mixture plugging has a propensity to cause splenic and portal vein embolism. Gelatin sponge tract embolization requires a comparatively long procedure time. And radiofrequency cauterization leads to parenchymal alteration and higher cost, compared with other procedures.
The percutaneous transhepatic approach to the portal vein has been widely utilized for various portal vein interventions including portal vein stent placement and portal vein embolization [25, 26]. A potential risk of the percutaneous transhepatic approach to the portal vein is also the peritoneal hemorrhage during and after the procedure. But, most interventional radiologists believe that the percutaneous transhepatic approach is safer than the percutaneous transsplenic approach. Although we presented the feasibility of percutaneous transsplenic approach in this article, we think the percutaneous transsplenic approach should be reserved for patients for whom conventional transhepatic or transjugular intrahepatic approaches are difficult or impossible.
In three cases of attempted portal vein recanalization, portal vein recanalization failed in two patients with chronic portal vein occlusion. This is not a problem of access to the portal venous system but, a problem of chronic stage of portal vein occlusion. In one patient (patient 8) who had acute portal vein thrombosis, recanalization of the portal vein was achieved by angioplasty and thrombolysis using urokinase. Thrombolytic therapy for portal vein thrombosis has been reported to accompany major complications up to 60% [27]. Whereas the mean total dose of urokinase was 7.2 million U (range 1.84–20.5 million U) over 23–72 h in that study [27], we used only 0.2 million U of urokinase over 1 h. We did not try transhepatic approach first in these three patients, because one patient (patient 9) had severely attenuated intrahepatic portal vein and two patients (patients 7 and 8) who received living donor liver transplantation had acute angle of portal vein.
This study has some limitations. First, the study consisted of a very small population and heterogeneous groups for endovascular treatment: four for gastric or jejuna varix embolization, two for portosystemic shunt embolization, and another three for possible portal vein recanalization. Second, the study lacked a standard follow-up imaging protocol. Ultrasound investigation is necessary and effective for detection of early complication from the splenic puncture site during the immediate postprocedural period. CT scan was performed in all patients but was undertaken at 2–19 days after the procedures. Eight patients survived >3 months after the procedure without late complications. One patient who died on the fifth day after the procedure had no bleeding around the spleen on CT scan obtained 2 days after the procedure. We thought this patient died of hepatic and renal failure caused by massive variceal bleeding and transfusion before the procedure.
In conclusion, we have demonstrated that several vascular complications in patients with chronic liver disease can be treated successfully using a percutaneous transsplenic approach without bleeding complication from the spleen. Therefore, percutaneous transsplenic access to the portal vein can be an alternative route for portography and further endovascular management in patients for whom conventional transhepatic or transjugular intrahepatic approaches are difficult or impossible.
References
Williams SG, Westaby D (1994) Management of variceal hemorrhage. BMJ 308:1213–1217
Sarin SK, Lahoti D, Saxena SP et al (1992) Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology 16:1343–1349
Kim T, Shijo H, Kokawa H et al (1997) Risk factor for hemorrhage from gastric fundal varices. Hepatology 25:307–312
Kwak HS, Han YM (2008) Percutaneous transportal sclerotherapy with N-butyl-2-cyanoacrylate for gastric varices: technique and clinical efficacy. Korean J Radiol 9:526–533
Luo JJ, Yan Z, Wang J et al (2011) Endovascular treatment for nonacute symptomatic portal venous thrombosis through intrahepatic portosystemic shunt approach. J Vasc Interv Radiol 22:61–69
Carnevale FC, Santos AC, Tannuri U et al (2010) Hepatic veins and inferior vena cava thrombosis in a child treated by transjugular intrahepatic portosystemic shunt. Cardiovasc Interv Radiol 33:462–470
Novellas S, Denys A, Bize P et al (2009) Palliative portal vein stent placement in malignant and symptomatic extrinsic portal vein stenosis or occlusion. Cardiovasc Interv Radiol 32:462–470
Ferro C, Rossi UG, Bovio G et al (2007) Transjugular intrahepatic portosystemic shunt, mechanical aspiration thrombectomy, and direct thrombolysis in the treatment of acute portal and superior mesenteric vein thrombosis. Cardiovasc Interv Radiol 30:1070–1074
Kiyosue H, Mori H, Matsumoto S et al (2003) Transcatheter obliteration of gastric varices: part 2. Strategy and technique based on hemodynamic features. Radiographics 23:921–937
Brazzini A, Hunter DW, Darcy MD et al (1987) Safe splenoportography. Radiology 162:607–609
Probst P, Rysavy JA, Amplatz K (1978) Improved safety of splenoportography by plugging of the needle tract. AJR Am J Roentgenol 131:445–449
Tsang YM, Au WY, Chen CM et al (1985) Percutaneous transsplenic balloon dilatation of stenotic distal splenorenal shunt. J Jpn Surg Soc 15:395–398
Harald B, Eva-Doreen P, Thomas B et al (2010) Transsplenic endovascular therapy of portal vein stenosis and subsequent complete portal vein thrombosis in a 2-year-old child. J Vasc Interv Radiol 21:1760–1764
David JT, Ffrrcsi JR, Mervin HD et al (2007) Percutaneous transsplenic access in the management of bleeding varices from chronic portal vein thrombosis. J Vasc Interv Radiol 18:1571–1575
Gong GQ, Wang XL, Wang JH et al (2001) Percutaneous transsplenic embolization of esophageal and gastrio-fundal varices in 18 patients. World J Gastroenterol 7:880–883
Durham JD, Kumpe DA, Stiegmann GV et al (1990) Direct catheterization of the mesenteric vein. Combined surgical and radiological approach to the treatment of variceal hemorrhage. Radiology 177:229–233
Bilbao JI, Quiroga J, Herrero JI et al (2002) Transjugular intrahepatic portosystemic shunt (TIPS): current status and future possibilities. Cardiovasc Interv Radiol 25:251–269
Spigos DG, Tauber JW, Tan WS et al (1983) Work in progress: umbilical venous cannulation: a new approach for embolization of esophageal varices. Radiology 146:53–56
Kim SC, Kim HC, Chung JW et al (2011) Percutaneous transumbilical portal vein embolization in patient with a ruptured hepatocellular carcinoma supplied by the portal vein. Cardiovasc Interv Radiol 34(suppl 2):214–217
Liang HL, Yang CF, Pan HB et al (1997) Percutaneous transsplenic catheterization of the portal venous system. Acta Radiol 38:292–295
Zins M, Vilgrain V, Gayno S et al (1992) US-guided percutaneous liver biopsy with plugging of the needle track: prospective study in 72 high-risk patients. Radiology 184:841–843
Smith TP, McDermott VG, Ayoub DM et al (1996) Percutaneous transhepatic liver biopsy with tract embolization. Radiology 198:769–774
Lee SH, Hahn ST, Yoo J et al (2000) Hemostatic effect of glue–lipiodol mixture plugged in the needle tract after renal biopsies in a high risk, anticoagulated rabbit model. Invest Radiol 35:684–688
Choi SH, Lee JM, Lee KH et al (2005) Postbiopsy splenic bleeding in a dog model: comparison of cauterization, embolization, and plugging of the needle tract. AJR Am J Roentgenol 185:878–884
Yoo H, Ko GY, Gwon DI et al (2009) Preoperative portal vein embolization using an amplatzer vascular plug. Eur Radiol 19:1054–1061
Kim KR, Ko GY, Sung KB, Yoon HK (2011) Percutaneous transhepatic stent placement in the management of portal venous stenosis after curative surgery for pancreatic and biliary neoplasms. AJR Am J Roentgenol 196:W446–W450
Hollingshead M, Burke CT, Mauro MA, Weeks SM, Dixon RG, Jaques PF (2005) Transcatheter thrombolytic therapy for acute mesenteric and portal vein thrombosis. J Vasc Interv Radiol 16:651–661
Acknowledgments
This study was supported by a grant from the Korea Healthcare technology R&D projects, Ministry of Health, Welfare & Family Affairs, Republic of Korea (A100655).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chu, H.H., Kim, HC., Jae, H.J. et al. Percutaneous Transsplenic Access to the Portal Vein for Management of Vascular Complication in Patients with Chronic Liver Disease. Cardiovasc Intervent Radiol 35, 1388–1395 (2012). https://doi.org/10.1007/s00270-011-0311-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-011-0311-y