Abstract
Purpose
The aim of this work was to develop and test a general methodology for the planning and performance of robot-assisted, MR-guided interventions. This methodology also includes the employment of software tools with appropriately tailored routines to effectively exploit the capabilities of MRI and address the relevant spatial limitations.
Methods
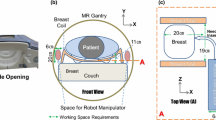
The described methodology consists of: (1) patient-customized feasibility study that focuses on the geometric limitations imposed by the gantry, the robotic hardware, and interventional tools, as well as the patient; (2) stereotactic preoperative planning for initial positioning of the manipulator and alignment of its end-effector with a selected target; and (3) real-time, intraoperative tool tracking and monitoring of the actual intervention execution. Testing was performed inside a standard 1.5T MRI scanner in which the MR-compatible manipulator is deployed to provide the required access.
Results
A volunteer imaging study demonstrates the application of the feasibility stage. A phantom study on needle targeting is also presented, demonstrating the applicability and effectiveness of the proposed preoperative and intraoperative stages of the methodology. For this purpose, a manually actuated, MR-compatible robotic manipulation system was used to accurately acquire a prescribed target through alternative approaching paths.
Conclusions
The methodology presented and experimentally examined allows the effective performance of MR-guided interventions. It is suitable for, but not restricted to, needle-targeting applications assisted by a robotic manipulation system, which can be deployed inside a cylindrical scanner to provide the required access to the patient facilitating real-time guidance and monitoring.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Minimally invasive interventions performed under image guidance most usually involve imaging modalities, such as computed tomography (CT), ultrasound (US), and x-ray fluoroscopy, but not magnetic resonance imaging (MRI). MRI does not use potentially harmful ionizing radiation and is not limited by the need for an acoustic window. It allows imaging in any arbitrary plane and provides a wealth of different contrast mechanisms, effectively allowing visualization not only of the anatomy and morphology but also function. Such supplementary information may be effectively exploited for stricter control over the interventional procedure itself [1]. Nevertheless, several reasons contribute to the limited use of MRI in interventional applications. First, MRI involves the use of strong static magnetic fields, rapidly switching magnetic field gradients, and radiofrequency (RF) fields, which impose strict limitations to any object exposed to the scanner’s environment. Second, for real-time image-guidance (i.e., with the patient inside the scanner) there is limited patient access and free space for maneuvering inside the gantry of the scanner [2, 3]. Additional factors, such as imaging time costs and availability, are also important. Real-time MR-guided interventions usually take place in low-field MR scanners, which mitigate the magnetic field effects and the patient access problem. Although open, high-field scanners currently constitute an attractive alternative [1, 4, 5], exploitation of the large installed base of high-field and ultra high-field cylindrical scanners, which are widely used in clinical practice, is highly desirable. In general, cylindrical scanners yield images of high quality by exploiting their high or ultrahigh field strength, improved static field homogeneity, and optimal gradient performance. A comprehensive review of standard diagnostic systems, including specially designed MRI systems, focuses on how well current systems meet the requirements of interventional MRI [6].
Until today, MRΙ-guided interventions have been primarily performed manually and various navigation concepts have been considered, such as stereotactic guidance and dynamic guidance (tracking interventional instruments by controlling the slice position/orientation), as reviewed by Moche et al. [7]. The use of robotic devices can achieve the required access to the patient inside the standard cylindrical scanner and exploit the advantages of high-resolution MRI for interventional purposes. A robotic manipulation system also may provide integration with software preoperative planning tools, whilst it may present further advantages compared to manual methods, including higher accuracy and steady-hand. Specialized MR-compatible robotic systems using appropriate materials and actuation/sensing methods have been developed for this purpose, as reviewed by Tsekos et al. [2]. Although most systems developed are experimental, a general purpose system for the positioning of interventional tools inside the scanner and performance of percutaneous procedures using preoperative planning software [8, 9] was commercialized (Innomotion™). In principle, with a manipulator facilitating the access to the patient inside the MR scanner and the use of an appropriate software tool, a procedure can be performed in a single session, effectively avoiding cumbersome and time-consuming multiple reentries. An example is the robotic system developed by Hata et al. [10], which uses an appropriate human-manipulator interface. Significant advantage of advanced robotic systems is their ability to provide haptic information to the operator (e.g., information regarding sight, sound and touch from the surgical site), as with the NeuroArm system [11], which was designed for microsurgery and stereotaxy.
The aim of this work was to develop a general methodology for patient-customized planning and performance of robot-assisted MR-guided interventions, and implement a software platform endowed with a graphic user interface (GUI) for its interactive use. The applicability and effectiveness of the proposed method and developed software were investigated with phantom studies performed using a prototype of a manually actuated and MR-compatible manipulation system currently developed by our team. The manipulator was specifically designed to provide access to the patient inside a cylindrical scanner for real-time guidance of needle-targeting procedures. The software tool was specifically designed to utilize preexisting MR images and embody planning and execution of minimally invasive interventions in a single, short session.
Materials and Methods
Methodology and Software for Preoperative Planning and Performance of an MR-Guided Intervention
The proposed methodology was developed considering image-guided, needle-based interventions in particular, such as biopsies [12] and local delivery of diagnostic [13] or therapeutic [14] agents. The software tool and GUI were developed using Matlab (The MathWorks, Inc.). Figure 1 shows a flowchart of the procedures and information regarding the proposed approach, which entails three distinct stages.
Flowchart of the proposed methodology for preoperative planning and performance of an MR-guided intervention using the software tool developed. The upper-left box represents the feasibility stage, the lower box the stereotactic preoperative planning procedure, and the upper-right box the intraoperative, interventional stage
The first stage is a feasibility study to investigate whether the specific patient under consideration can indeed be treated given the scanner-imposed geometric limitations and using the available manipulation system and interventional tools (e.g., biopsy needle of specific size). The software tool also enables the physician to make a decision regarding the appropriate positioning of the patient on the scanner’s table depending on the specific application and the targeted anatomy. For this stage, the required input to the software is the previously acquired set of DICOM images upon which the initial diagnosis was based warranting the interventional procedure.
The second stage is the preoperative planning procedure, which commences with the placement of the patient on the scanner’s table and the installation of the manipulator. The registration procedure, which relates the scanner’s coordinate reference system to that of the robot’s, is then performed. A multislice scan over the patient’s volume of interest (e.g., abdominal region) is acquired and uploaded to the preoperative planning software. Using the GUI provided, the operator runs through the acquired slices and freehand delineates the target region-of-interest (ROI), as well as any ROIs potentially at risk. Thus, the three-dimensional (3D) target volume, as well as any “critical” volumes that the needle’s path is not allowed to trespass, are selected. Having defined the target volume, the inverse kinematics procedure for the manipulator is employed to provide any available arm positions that will yield alignment of the needle on the end-effector with the target volume. Inverse kinematics is the mathematical procedure of finding the sets of positions of the joints of a robotic manipulator that must be attained so that its end-tool reaches a prescribed position. In practice, and within the context of this work, the software performs the inverse kinematics to deploy the robot so that the tip of the interventional tool (e.g., a biopsy needle) may reach a particular point (e.g., the center of a lesion) as it is selected from the preoperative MR images. Often, a certain target can be reached along alternative paths, as calculated by the inverse kinematics. In this case, the interventionalist may select the apparently most appropriate solution. For this purpose, any solutions that violate the defined critical ROIs are automatically eliminated by the software and the remaining ones are evaluated based on specified criteria. Those criteria are set by the operator and each one has different weighting in the process of selecting the most appropriate one (for example, see the collection of criteria in Table 1 and the relevant details provided in the “Results” section).
The third stage of the procedure begins with the adjustment of each joint of the manipulator to the required position. The correctness of the resulting tool alignment with the target is verified using appropriately prescribed MR images and, if necessary, fine position adjustments are performed. Needle insertion, target acquisition, and performance of the actual interventional task are performed using real-time MR imaging. After verification of task accomplishment, the procedure is concluded with the needle removal and the release of the patient. In the experiments described hereinafter, a proprietary interactive imaging interface (Philips Medical Systems, Best, The Netherlands) and a projector with a projection-screen built in-house were used for MR fluoroscopy and in-room display, respectively.
Manipulator
In the studies presented herein, a prototype of a manual manipulator was used [15]. The robotic manipulation device was designed to directly mount onto the patient’s table and provide the required access to the patient inside a cylindrical scanner, allowing the performance of needle targeting applications using real-time MR guidance. To ensure MR-compatibility, the manipulator was constructed of a variety of plastic materials. Unlike many of the systems previously developed, it is a general purpose system, i.e., not application or anatomy specific. The system is endowed with five degrees-of-freedom, which are manually actuated through a control handle from outside the gantry. An interchangeable end-effector is attached at the tip of the arm and serves as a holder for the application tool (e.g., a biopsy needle). Given the construction materials, which are MR-inert, the device is not visible in the images. To visualize the needle while performing a targeting procedure, MRI-visible markers have been appropriately installed on the end-effector. Specifically, a pair of parallel, thin cylindrical tubes, filled with a gadolinium chelate solution of 0.01 mM (Magnevist, Bayer Shering Pharma, Berlin, Germany), was symmetrically placed on either side of the needle. In T1-weighted images, these markers appear as two bright lines allowing designation of needle orientation and determination of tip position.
Experimental Validation Studies
The herein described planning method and the associated software were tested with experimental studies involving human volunteers and an appropriate phantom. The trials first assessed the ability of the robotic hardware to provide the required access to a human subject inside the confined space of the MR gantry. Then, in a series of phantom studies, the applicability and effectiveness of the proposed methodology was examined with regard to the acquisition of a selected target along alternative needle insertion paths, while reliably avoiding designated critical anatomies and reducing the time required to complete the task.
To test the methodology steps and the software module that relate to the investigation of the feasibility of a particular minimally invasive MR-guided interventional procedure, a human volunteer imaging study was conducted. Four volunteers, exhibiting a range of body habiti from quite lean to very chubby, were imaged using a cylindrical, 1.5T MRI system with a bore diameter of 60 cm (NT-Intera, Philips Medical Systems). Transverse, sagittal, and coronal sections were acquired using a T2-weighted turbo spin echo (TSE) pulse sequence (100 ms echo time, 1600 ms repetition time). The built-in, quadrature RF body coil was used for both excitation and signal detection.
A phantom study was performed to simulate the preoperative planning procedure and performance of a targeting intervention under realistic clinical conditions. The phantom was comprised of a box-shaped container filled with fat (butter), in which an elliptically shaped grape (maximum and minimum diameters of 2 and 1 cm, respectively) was immersed to represent the target. A group of vitamin capsules was embedded in a plastic cup, which was also placed at the surface of the fat 1.5 cm above the target, representing a subcutaneous physical obstruction, such as a bony structure. A plastic tube filled with an aqueous solution (0.01 mM) of a paramagnetic contrast agent (Magnevist, Bayer Shering Pharma, Berlin, Germany) was dipped in the fat at a 4 cm distance from the target, representing a critical anatomy to be avoided during needle targeting. The prototype manipulator and a commercially available (Somatex Medical Technologies, Teltow, Germany) MRI-compatible needle typically used for the injection of drugs and for fine needle aspiration biopsies (MRI Chiba Needle, 20 G/0.95 × 150 mm) were used for performing the experiment within the above-mentioned MRI scanner and with the use of the RF body coil. A single-shot, RF-spoiled, gradient echo pulse sequence (4.6 ms echo time, 7.7 ms repetition time) was used for localization purposes and intraoperative dynamic imaging (temporal resolution of 1 ms), whilst a T1-weighted TSE pulse sequence (7.4 ms echo time, 450 ms repetition time) was used for morphological imaging (isotropic spatial resolution of 3 mm).
Results
Among the outputs of the developed software are images, such as the one presented in Fig. 2. This figure shows a transverse MR image acquired from a volunteer of moderate body size with geometrical information superimposed on it. It includes calculated distances between the body perimeter and gantry wall along selected radial directions. The two dash-lined ellipses represent the effective field-of-view (FOV) at the isocenter of the specified scanner (outer ellipse), as well as at a distance ±9 cm away along its longitudinal axis (inner ellipse). The three marked zones extending inside the body of the patient represent the “attainable volume,” i.e., the accessible anatomical volume for a needle of the specified length (8 cm in this example), along three different directions (two from sideways and one from the top). The figure also depicts the physical dimensions of the end-effector. Given that this approach does not consider any physical obstructions to the needle’s passage (e.g., bones) or any other limitations due to the presence of sensitive organs and/or deformable tissues, the presented information only provides a rough, but yet useful, indication of the accessible body regions for a specific setup.
Preoperative feasibility study based on patient-specific data. Software output combines: A Calculated distances between patient and gantry wall (circle) along selected radial directions. B Scanner’s effective FOV. Outer ellipse FOV at the isocenter, inner ellipse FOV approximately ±9 cm away from the isocenter. C Attainable anatomical region for an 8 cm–long needle. D Graphical representation of the end-effector at the upright position (vertical to the patient surface)
Figure 3 shows a screen caption of the preoperative planning GUI with data acquired from the experimental phantom study. In this study, the phantom was positioned so its top surface corresponds to the approximate position of the torso surface of an average sized human. As mentioned previously, the tool allows the physician to inspect all acquired slices and delineate the target, as well as any physical obstructions and critical areas or organs at risk on a slice-by-slice basis. By repeating the procedure on a sufficient number of consecutive slices, the 3D geometries of the volumes of interest are defined. Alternatively, if desired the operator may skip intermediate slices in which case the 3D volume is reconstructed by interpolation from the slices that have been marked. The inverse kinematics routine is then executed to provide any attainable solution(s), i.e., the sets of joint positions that yield alignment of the end-effector with the selected target. In the case of multiple possible solutions, the interventionalist may select the preferred one by taking into account various designated criteria. Criteria adopted and applied in the current study are presented in Table 1. The software module automatically calculates the distance between the target’s centroid and the interventional tool’s axis for any given solution, whereas it provides the necessary measurement tools so that the operator can determine the various distances and angles of interest.
Screen caption of the preoperative planning software GUI. The interventionalist goes through a set of consecutive images and freehand delineates the target ROI and the critical ROIs using the mouse. A selected target area (circular area), as well as two drawn critical areas (a horizontal rectangle simulating a physical obstruction near the upper boundary, and an upright rectangle representing an organ at risk) appear in the main display image. Upon confirming the corresponding volumes, the software produces the inverse kinematics solutions for the placement of the manipulator with the end-effector aligned with the target. An image perpendicular to that of the main display, which corresponds to the level of the target’s centroid, is shown on the upper left corner of the GUI
Figure 4A shows a 3D representation of the phantom inside the gantry (constructed through a segmentation procedure), along with the prescribed target (center) and critical volumes, as appear on the GUI. Three different configurations of the arm with the needle accessing the target, selected from the attainable inverse kinematics solutions, also are presented. For each solution, the software provides the corresponding joint positions that were used for adjusting the end-effector to the required position. The correctness of the end-effector positioning was confirmed by using appropriate oblique images depicting the MRI markers, and needle insertion was initiated while the procedure was monitored under real-time imaging. Figure 4B–D show the needle having acquired the target after the implementation of the three selected configurations of the manipulator. It is noted that the magnetic susceptibility artifact associated with the needle in the high receiver bandwidth image of Fig. 4B has a smaller diameter (approximately 4 mm) compared with that of the artifact in Fig. 4C (approximately 5 mm), which was obtained with a low receiver bandwidth. In both cases, as well as in the case of Fig. 4D, the needle’s long axis was not perpendicular to the main magnetic field, B0, resulting in a moderate magnetic susceptibility artifact [16] not exceeding 5 mm, which has been postulated as the limit for avoiding obscurement of critical anatomic information [17].
A Three-dimensional representation showing the phantom (generated through segmentation of a multislice set), along with the selected target and critical volumes. The line representations of the manipulator correspond to three attainable solutions. B Transverse MR image (2.7 kHz per pixel receiver bandwidth) showing the needle having acquired the target with implementation of solution (i). C Transverse MR image (0.4 kHz per pixel receiver bandwidth) showing the needle having acquired the target with implementation of solution (ii). D Oblique transverse MR image (2.7 kHz per pixel receiver bandwidth) showing the needle having acquired the target with implementation of solution (iii). The MRI markers used to confirm the needle’s position outside the phantom and the alignment of the end-effector with the target are visualized
During the phantom studies, the physician became accustomed to comfortably using the preoperative planning software as well as controlling the manipulation system to guide the intervention without any prior systematic training. A contributing factor was the rather intuitive kinematic structure of the arm that has been developed. Initially, it was confirmed that usage of the robotic manipulation system may indeed provide a dexterous reach inside the bore of an MR scanner as required to capitalize on its scanning capabilities for real-time image guidance. The steady-hand characteristic of the manipulation device was positively commented by the physician. Also pointed out was the fact that the robotic device alleviates the need for the operating physician to maintain an awkward position as often required when operating inside an open, low-field scanner. The combination of stereotactic together with real-time guidance was found effective in accomplishing an accurate needle targeting with potential enhancements to patient safety by reliably avoiding critical structures. It also circumvents the need for successive reentries of the patient into the scanner to complete a targeting and effectively accelerates task execution. Testing showed that target acquisitions through alternative needle paths proposed by the planning software were consistent and straightforward, without requiring successive needle insertion trials.
Discussion
Most of the MR-guided interventions involving a cylindrical scanner are performed stereotactically (such as neurosurgical interventions which take place outside the scanner’s bore with the use of preoperative images and stereotactic frames) or employ an iterative, “try and test” procedure (such as biopsies that comprise manual needle feed with the patient outside the bore, and target selection along with verification of needle positioning and target acquisition with the patient inside the bore). Capitalizing on the use of manipulation assistance, the capabilities of high-field MRI can be fully exploited enhancing the interventional procedure’s effectiveness and securing patient’s safety. For example, the possibility of false-negative biopsy results can be drastically reduced, whereas, in the case of a targeted drug delivery, accurate needle targeting can be achieved increasing agent’s concentration in the target and minimizing nontarget distribution.
Integration of interventional MRI with computer-assisted surgery allows relating data originating from different sources or collected at different times (e.g., preoperative and intraoperative data), thus enhancing the effectiveness of image-guided interventions [18]. To fully exploit the power of MRI, appropriate tools have to be developed, such as that presented by Gering et al. [19], where different data sets representing both morphology and function are fused and effectively combined into a single visualization environment to facilitate planning and guidance of neurosurgical procedures performed in an open MRI scanner. In an effort to improve image quality while maintaining patient accessibility in MR-guided prostate therapy, Fei et al. [20] suggested the registration of a high-resolution MRI volume acquired at 1.5T with real-time images obtained at low-field. Tang et al. [21] considered capturing and fusing information obtained simultaneously from two different modalities, MRI and US, to be used for needle guidance in breast biopsy. To facilitate image-guided targeting, Wacker et al. [22] implemented an augmented reality system, which effectively maps medical data (preoperative MR images) onto the patient’s body. Whereas the navigation-based approaches facilitate and simplify the interventional procedure itself, deformable registration between image sets can introduce inaccuracies [23].
The present work proposes a methodology for performing MR-guided targeting procedures inside a cylindrical scanner with a manipulation system and effectively encompasses three discrete stages: (1) Feasibility study customized for a prescribed minimally invasive procedure on an individual using previously acquired image datasets. (2) Stereotactic localization and planning based on preoperative MR imaging. The option of frameless stereotaxy is made possible by the fact that MRI provides a fixed coordinate reference system. Upon registering a robotic arm with this system, the manipulator may accurately align its end-effector with a target identified in the acquired images (as long as the patient maintains a fixed position). The privilege of having an inherent-to-the-modality fixed reference coordinates system is not enjoyed by US, where a scan is performed using a hand-held probe. (3) Real-time intraoperative imaging for tracking the motion of interventional tools (e.g., needle insertion) and monitoring of the actual interventional task execution. MRI may further facilitate this part given that scan plane geometry and image contrast can be adjusted dynamically [24]. Real-time image guidance practically overcomes a weakness inherent in stereotactic approaches employing frames, which they lack intraoperative information and, therefore, are blind to tissue displacement, tissue deformation, or needle bending during insertion [25]. Most reported techniques maintain a focus on a stereotactic or a real-time guidance approach. The methodology presented herein (summarized in Fig. 1) capitalizes on both approaches to exploit the benefits of each one. Also, the preoperative feasibility study has become an integrated part of the procedure. Another novelty regarding the implementation of the approach is the use of a fully manually actuated manipulator rather than a computer-controlled robotic device, which has been the case with the majority of the experimental results reported in the literature, as for example [8, 10, 11, 18, 24]. However, the proposed approach is not specific to the manual arm used in this work, but it can be used in conjunction with any other suitable MR-compatible robotic manipulator.
The performed human volunteer studies suggest that the developed tool may assist an interventionalist to evaluate the feasibility of a standard clinical approaching path for performing a prescribed minimally invasive procedure inside a cylindrical scanner and make a patient-customized decision. An MRI-compatible robotic manipulator has to be deployed inside the scanner’s gantry to provide access to the patient as required for real-time guidance. Although geometric considerations associated with the physical dimensions of the MRI gantry and the given patient anatomy, as well as the manipulation system and the application tools utilized, are well understood, usually they are not systematically analyzed and evaluated. The software module developed can make effective use of MR images previously acquired and possibly used for the initial diagnosis that led to the prescription of an interventional procedure. As illustrated in Fig. 2, a needle longer than 8 cm may be needed to reach some anatomical regions when the patient considered lies in supine position, whilst the chosen end-effector must be tilted away from its upright position to enable a sideways approach. The physician can also visualize the approximate attainable anatomical regions with the patient in the prone position by flipping the transverse images (e.g., in the case that the target is a paraspinal lesion) or can visualize the attainable regions on sagittal and/or coronal sections exploring the feasibility, for example, of an approaching path below the thoracic cage for targeting a subdiaphragmatic lesion.
The implemented inverse kinematics routine may provide many solutions, one solution, or no solution at all. The last case effectively corresponds to a target lying outside the manipulator’s workspace and patient repositioning should be considered. The first case, encountered in the presented experimental validation study, represents the most probable scenario given that when planning the procedure a target volume is selected rather than a target point. It is imperative, therefore, to make sure that the optimal solution is finally implemented. To this scope, certain general criteria were set that have to be considered while selecting an optimal solution, mainly with regard to patient’s safety and the intervention’s effectiveness. Of course, one can appreciate that these criteria have to be refined, expanded, or appropriately adjusted for specific interventional practices and procedures. Although the performed experimental phantom study does not permit to further elaborate on the above-mentioned issue, it helps to evaluate the validity, reliability, and accuracy of the suggested methodology. In this study, all three attempted solutions successfully acquired the prescribed target.
The proposed approach and the implementation software can be further refined to provide more assistance to the interventionalist, mainly by automating certain tasks. The fact that the developed tool does not incorporate an algorithm for semiautomatic tissue segmentation may be regarded as a limitation, although it does not limit the generality of the method. To implement this functionality, patient-specific information will need to be effectively combined together with anatomical atlases. Nevertheless, the painstaking manual segmentation approach not only allows the detailed delineation of the target, but also the consideration for physiological variations in size, shape, and position of the sensitive anatomical structures, e.g., bladder filling, respiratory movement, and peristaltic movement. In effect, the physician can prescribe the critical volumes by encompassing the organs at risk with a safety margin to account for these internal, physiological variations, and deformations. Another useful improvement would be the ability of the system to automatically propose an optimal solution, when multiple solutions are available, regarding the positioning of the arm before targeting. For this purpose, each attainable solution can be graded on the basis of appropriate criteria (Table 1) after assigning them weighting factors indicating their significance. Various other constraint conditions eliminated in this work, such as the use of patient immobilization and support appurtenances, also have to be considered.
In conclusion, the approach presented is well-suited to various diagnostic and therapeutic, minimally invasive applications involving MR-guided needle targeting inside a cylindrical scanner. However, the specifics of each interventional procedure need to be thoroughly considered to properly adapt the methodology, software tool, and manipulation hardware for meeting prescribed requirements and goals.
References
Streitparth F, Gebauer B, Melcher I et al (2009) MR-guided laser ablation of osteoid osteoma in an open high-field system (1.0 T). Cardiovasc Intervent Radiol 32:320–325
Tsekos NV, Khanicheh A, Christoforou E, Mavroidis C (2007) Magnetic resonance-compatible robotic and mechatronics systems for image-guided interventions and rehabilitation: a review study. Ann Rev Biomed Eng 9:351–387
Keroglou C, Seimenis I, Tsekos NV et al. (2010) Consideration of geometric constraints regarding MR-compatible interventional robotic devices. In: Proceedings of 3rd IEEE/RAS-EMBS international conference on biomedical robotics and biomechatronics, Tokyo, Japan
Wonneberger U, Schnackenburg B, Streitparth F et al (2010) Evaluation of magnetic resonance imaging-compatible needles and interactive sequences for musculoskeletal interventions using an open high-field magnetic resonance imaging scanner. Cardiovasc Intervent Radiol 33:346–351
Fischbach F, Bunke J, Thormann M et al (2011) MR-guided freehand biopsy of liver lesions with fast continuous imaging using a 1.0-T open MRI scanner: experience in 50 Patients. Cardiovasc Intervent Radiol 34:188–192
Hushek SG, Martin AJ, Steckner M et al (2008) MR systems for MR-guided interventions. J Magn Reson Imaging 27:253–266
Moche M, Trampel R, Kahn T et al (2008) Navigation concepts for MR image-guided interventions. J Magn Reson Imaging 27:276–291
Melzer A, Gutmann B, Remmele T et al (2008) INNOMOTION for percutaneous image-guided interventions: principles and evaluation of this MR- and CT-compatible robotic system. IEEE Eng Med Biol Mag 27:66–73
Moche M, Zajonz D, Kahn T et al (2010) MRI-guided procedures in various regions of the body using a robotic assistance system in a closed-bore scanner: preliminary clinical experience and limitations. J Magn Reson Imaging 31:964–974
Hata N, Tokuda J, Hurwitz S, Morikawa S (2008) MRI-compatible manipulator with remote-center-of-motion control. J Magn Reson Imaging 27:1130–1138
Sutherland GR, Latour I, Greer AD (2008) Integrating an image-guided robot with intraoperative MRI: a review of the design and construction of neuroArm. IEEE Eng Med Biol Mag 27:59–65
Weiss CR, Nour SG, Lewin JS (2008) MR-guided biopsy: a review of current techniques and applications. J Magn Reson Imaging 27(2):311–325
Graves MJ, Wakely S, Bearcroft PW et al (2008) MR-guided direct arthrography of the hip. J Magn Reson Imaging 28:462–465
Arepally A (2008) Targeted drug delivery under MRI guidance. J Magn Reson Imaging 27:292–298
Keroglou C, Tsekos NV, Seimenis I et al. (2009) Design of MR-compatible robotic devices: magnetic and geometric compatibility aspects. In Proceedings of 9th international conference on information technology and applications in biomedicine, Larnaca, Cyprus
Kühn J-P, Langner S, Hegenscheid K et al (2010) Magnetic resonance-guided upper abdominal biopsies in a high-field wide-bore 3-T MRI system: feasibility, handling, and needle artefacts. Eur Radiol 20:2414–2421
Frahm C, Gehl H-B, Melchert UH et al (1996) Visualization of magnetic resonance-compatible needles at 1.5 and 0.2 Tesla. Cardiovasc Intervent Radiol 19:335–340
Jolesz FA, Nabavi A, Kikinis R (2001) Integration of interventional MRI with computer-assisted surgery. J Magn Reson Imaging 13:69–77
Gering DT, Nabavi A, Kikinis R et al (2001) An integrated visualization system for surgical planning and guidance using image fusion and an open MR. J Magn Reson Imaging 13:967–975
Fei B, Duerk JL, Boll DT et al (2003) Slice-to-volume registration and its potential application to interventional MRI-guided radio-frequency thermal ablation of prostate cancer. IEEE Trans Med Imaging 22:515–525
Tang AM, Kacher DF, Lam EY et al (2008) Simultaneous ultrasound and MRI system for breast biopsy: compatibility assessment and demonstration in a dual modality phantom. IEEE Trans Med Imaging 27:247–254
Wacker FK, Vogt S, Khamene A et al (2006) An augmented reality system for MR image-guided needle biopsy: initial results in a swine model. Radiology 238:497–504
Susil RC, Camphausen K, Choyke P et al (2004) System for prostate brachytherapy and biopsy in a standard 1.5 T MRI scanner. Magn Reson Med 52:683–687
Christoforou E, Akbudak E, Ozcan A et al (2007) Performance of interventions with manipulator-driven real-time MR-guidance: Implementation and initial in vitro tests. Magn Reson Imaging 25:69–77
Abolhassani N, Patel R, Moallem M (2007) Needle insertion into soft tissue: a survey. Med Eng Phys 29:413–431
Acknowledgments
This work was supported by the Cyprus Research Promotion Foundation and the European Regional Development Fund (grant TEXNOLOGIA/MHX/0308(BIE)/05). NVT acknowledges partial support by the National Science Foundation (NSF) award CNS-0932272.
Conflict of interest
The authors declare that they have no conflict of interest regarding the work presented in this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Seimenis, I., Tsekos, N.V., Keroglou, C. et al. An Approach for Preoperative Planning and Performance of MR-guided Interventions Demonstrated With a Manual Manipulator in a 1.5T MRI Scanner. Cardiovasc Intervent Radiol 35, 359–367 (2012). https://doi.org/10.1007/s00270-011-0147-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-011-0147-5