Abstract
The purpose of this study was to evaluate the clinical feasibility and efficacy of transcatheter selective arterial chemoembolization (TACE) for unresectable hepatoblastoma in infants and children. The study was performed with the approval of our institutional review board. Sixteen patients (13 boys, 3 girls) with unresectable hepatoblastoma were treated one to three times with preoperative TACE in an effort to improve the surgical and clinical outcome. Their ages ranged from 50 days to 60 months, with a mean age of 20.4 months. All cases were pathologically proved hepatoblastoma by fine-needle biopsy. After an intra-arterial catheter was selectively inserted into the main feeding artery of the tumor, cycles of cisplatin (40 to 50 mg/m²) and adriamycin (20 to 30 mg/m²) mixed with lipiodol were given, followed by gelatin foam particles or stainless-steel coils. Tumor response was evaluated according to tumor shrinkage, α-fetoprotein (AFP) levels, and pathological findings. TACE procedure was performed one to three times, depending on the patient’s response. Surgical resection was carried out when the tumor volume appeared sufficiently reduced to allow safe resection by either lobectomy or extended lobectomy. A marked reduction in tumor size associated with decreased AFP level occurred after treatment. According to paired-samples test, tumor shrinkage ranged from 19.0% to 82.0%, with a mean value of 59.2%. AFP levels decreased 99.0% to 29.0% from initial levels, with a mean decrease of 60.0%. TACE allowed subsequent complete surgical resection in 13 cases and the other 3 cases underwent partial resection. One patient underwent successful orthotopic liver transplantation after receiving TACE therapy. Pathological examination showed that the mean percentage of necrotic area in the surgical specimens was 87%. Overall survival rate at 1, 3, and 5 years was 87.5%, 68.7%, and 50%, respectively. Correspondingly, event-free survival rate was 75%, 62.5%, and 43.7%, respectively. In addition, there was no marked chemotherapeutic agent-induced toxicity noted during the observation period. We conclude that TACE is feasible, well tolerated, and effective in inducing surgical resectability of hepatoblastoma in pediatric patients, which has become an independent palliative or curative therapeutic option, especially for patients without distant metastasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatoblastoma (HB) is the most common malignancy of the liver in infants and children; complete surgical resection of the primary tumor is absolutely vital to achieve HB cure [1–3]. However, 50% of cases are unresectable at initial presentation due either to local bilobar or porta hepatis invasion or to metastatic spread. In this situation it has traditionally been associated with poor prognosis [3–6]. Preoperative systemic chemotherapy plays a vital role in reducing tumor size and controlling tumor spread to convert an unresectable tumor to a resectable one [7–10]. However, there are several potential risks, including cardiac and bone marrow damage and adverse effects of hepatic regeneration after delayed operation, and some tumors remain unresectable [11–15]. Therefore, there is a need for new therapeutic methods and alternative treatments that will reduce these disadvantages of systemic chemotherapy and improve the survival rates of these patients. TACE (transcatheter selective arterial chemoembolization) refers to combination transarterial administration of a chemotherapeutic and a vascular occlusive agent in treatment of HB as a potentially independent palliative or an adjuvant preoperative treatment [4–6, 9, 16]. The purpose of our study was to evaluate the feasibility and effectiveness of preoperative TACE for HB that is unresectable because of extensive hepatic involvement and indistinct margins at medical imaging.
Materials and Methods
Patients
The study was performed with the approval of our institutional review board, and written informed consents were obtained from all patients’ legal guardians. Between 1997 and 2003, 16 cases with HB were enrolled in our study. There were 13 males and 3 females, and their ages ranged from 50 days to 60 months, with a mean age of 20.4 months. All cases were confirmed by computed tomography (CT) or magnetic resonance imaging (MRI) within 2 weeks of study entry. The tumor was considered unresectable because it involved bilobar of the liver or had main hepatic vessels or inferior vena cava invasion. According to the International Society of Pediatric Oncology (SIOP) and PRE-Treatment EXTent of disease (PRETEXT) Grouping System [17, 18], there were four cases with porta hepatis invasion (group III), two cases with multiple pulmonary metastatic lesions at presentation (group IV), seven cases with three liver sectors invasion (group III), and three cases with two liver sectors (group II). All cases were pathologically proven HB by biopsy before TACE. Serum α-fetoprotein (AFP), tumor volume, complete blood and platelet counts, liver function tests, and coagulation profile were obtained within 1 week before TACE and 3 weeks after TACE.
Treatment
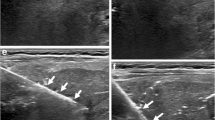
Under general anesthesia and aseptic conditions, the femoral artery was catheterized using Seldinger technique. A 4-Fr catheter was introduced percutaneously into the femoral artery. Under fluoroscopy of digital subtraction angiography (DSA), the catheter was manipulated into the celiac axis and superior mesenteric artery. Arteriography was performed to demonstrate the anatomy, identify accessory arteries, and confirm the patency of the portal vein. During the capillary phase, tumor staining was mainly distributed in the right lobe of the liver or, sometimes, the left lobe of the liver or throughout the liver; no intraportal venous thrombosis was found during the venous phase. Through the catheter, a microcatheter was selectively introduced and directed to the artery supplying the tumor. Cisplatin (40 to 50 mg/m²) and adriamycin (20 to 30 mg/m²) dispersed in lipiodol were injected into the feeding artery of the tumor within a few minutes, followed by embolic materials using gelatin foam particles (1 × 2 mm) or stainless-steel coils, until near-complete stasis of the blood flow had occurred (Fig. 1). The total volume of the suspension to be administered to achieve stasis varied in each session; however, the total volume injected was not to exceed 10 ml and treatment was to be limited to no more than 70% of the total liver volume. After treatment, patients were hydrated and continued to receive antibiotics for at least 48 h. Postprocedure pain was managed with parenteral analgesics as needed, and nausea and vomiting were treated with antiemetics. TACE procedure was performed one to three times depending on the patient’s response. Subsequent surgical resection was generally carried out at approximately 4-week intervals after last TACE. Surgical resection was carried out when the tumor volume appeared to be sufficiently reduced to allow safe resection by either lobectomy or extended lobectomy. Tumor volume was determined with CT or MR 4 weeks after TACE. Moreover, at least two courses of systemic chemotherapy were appended to all cases. Cycles of cisplatin (20 mg/m2/day for 3 days) and adriamycin (25 mg/m2/day for 3 days) were administered every 3 weeks by continuous intravenous infusion.
Evaluation of Response
Four weeks after TACE, the largest transverse diameter through the tumor center was measured on axial CT images and the tumor volume was calculated by the equation, volume = ½ × length × (transverse diameter)2 (Fig. 2). Partial response (PR) was defined as a decrease of ≥50% in tumor volume, with no evidence of new lesions or progression in any lesion. Nonresponse (NR) was defined as <25% decrease in tumor volume of all measurable lesions, with no evidence of new lesions or progression in any lesion. For purposes of this article, a decrease between 25% and 50% was also defined as NR. The extent of tumor necrosis was histologically evaluated as the percentage of necrotic or fibrotic area in the largest section of the surgical specimen. We also investigated the clinical symptoms and the serum AFP level before and after TACE on the third day.
Toxicity
Toxicity was assessed after TACE. Cadiac function was monitored by electrocardiography; renal function, by serum electrolytes, urea, creatinine, and creatinine clearance; and liver function, by glutamicoxaloacetic transaminase (GOT), glutamic-pyruvic transaminase (GPT), alkaline phosphatase, γ-guanosine 5′-triphosphate, and bilirubin. Inflammatory reaction was monitored by C-reactive protein (CRP).
Results
Response to TACE
A marked reduction in tumor size associated with a decrease in AFP level occurred after TACE (see Table 1). The tumor volume decreased from 19% to 82%, with a mean value of 59.2%. According to the above PR and NR criteria, 13 cases were considered PRs, while 3 cases were NRs. There was a PR in 81.3% cases (13/16), a minor response in 12.5% of cases (2/16), and stable disease in 6.25% of cases (1/16). AFP levels fell 29% to 99% (mean, 60%) from initial levels. No delay of surgery was encountered and the time interval between TACE and surgical rescection was 28 ± 1.8 days. TACE allowed subsequent safe complete surgical resection in 12 cases (75%), and the other 3 cases (18.7%) underwent partly resection. One patient (6.3%) underwent successful orthotopic liver transplantation (OLT) after receiving TACE therapy. Pathological examination showed massive necrosis in the excisional specimens, and the percentage of necrotic area within the tumor ranged from 18% to 92%, with a mean level of 64.9% (Fig. 3).
Clinical Symptoms
After TACE, all patients presented with fever, and their temperatures ranged from 37.5°C to 39.5°C for 2 to 3 days. Other clinical symptoms, including nausea, vomiting, and poor appetite in 14 cases, dental ulcer in 1 case, and diarrhea in 2 cases, recovered within 5 days under suitable treatment. In addition, there was no marked chemotherapeutic agent-induced toxicity noted during TACE and postoperative systemic chemotherapy.
Prognosis
During the average 46-month follow-up, two patients died of extensive lung metastasis, at 2 and 36 months after the operation, respectively. One patient died of liver failure 1 year after TACE. Six patients died of tumor recurrence. The remaining seven cases were doing well and free of disease. At 1, 3, and 5 years, overall survival (OS) was 87.5%, 68.7%, and 50%, and event-free survival (EFS) was 75%, 62.5%, and 43.7%, respectively.
Discussion
Resectability of the primary tumor is the most important factor for the long-term survival of children with HB [1–3]. The cornerstones of successful treatment include total surgical excision and adjuvant chemotherapy. However, more than half of all children with HB have unresectable tumors at presentation due to local bilobar or porta hepatis invasion or to metastatic spread [3–6]. Preoperative systemic chemotherapy plays a vital role in reducing tumor size and converts an unresectable tumor to a resectable one, thus improving prognosis [7–10]. For patients with unresectable or metastatic HB, the Pediatric Oncology Group (POG) moved to a treatment strategy based on intensification of preoperative chemotherapy according to tumor response [19]. However, the associated systemic adverse effects, such as myelosuppression and cardiotoxicity, sometimes lead to delayed surgery and hence tumor regrowth and chemotherapy-related death [11–15]. Moreover, there are the problems of drug resistance [9] and induction of a second malignancy [15] by anticancer drugs. Several reports have described the successful use of intra-arterial injection of tumor agents for unresectable HB in infants. The rationale of this treatment is the exposure of tumor cells to high concentrations of drugs, which cannot be achieved by systemic administration using the same dose. However, the treatment requires laparotomy for placement of a catheter [20, 21]. To reduce these disadvantages of systemic chemotherapy, an alternative targeting therapy, which can maximize the drug uptake of the tumor and minimize drug exposure to the host, is required.
TACE has been used extensively in hepatocellular carcinoma (HCC) in adults in the last 10 years [22–25]. It has proven to be a valuable method: first, embolization increases the dwell time of the chemotherapeutic agent; second, by occlusion of the blood supply to the tumor, ischemia ensues, followed by hypoxic tissue damage to the tumor. Furthermore, lipodol is effective as an emulsion in chemoembolization when mixed with chemotherapeutic agents, because it is selectively absorbed and retained by emulsification and pinocytosis in hepatic tumor cells [26]. It can provide differentiation between normal parenchyma and tumor as confirmed by CT imaging and pathologic findings. Liovet et al. [25] reported that preoperative TACE could improve survival in patients with unresectable HCC. However, experience with TACE in children is somewhat limited [4–6, 9, 16]. Pediatric interventions differ from adult interventions in that both the setting and the equipment must be adapted to infants and children. Needless to say, another technical challenge is the very small vessel diameter of pediatric vessels, which demands more skill and experience to avoid perforation or dissection. Therefore, the disease processes and the indications for treatment are clearly distinct in this age group. Nowadays, pediatric embolotherapy has become feasible, thanks to the availability of microcatheters and other supplies. There have been several reports in the literature of TACE application in pediatric patients with HB [4–6, 9, 16].
In our series, most patients showed a marked response to TACE, a nearly linear decrease in AFP levels, and a reduction in tumor size. Consequently, 81.3% underwent complete surgical resection of the tumor with no morbidity; the 1-, 3-, and 5-year OS was 87.5%, 68.7%, and 50%, and the EFS was 75%, 62.5%, and 43.7% respectively, values strikingly similar to the results for HB in the POG Phase II study [19]. In that study, 5-year EFS estimates were 59% ± 11% for stage III disease and 27% ± 16% for stage IV disease. In SIOPEL study-1, the long-term (current follow-up is >10 years for all patients), disease-free patient survival was 66% for the whole series [17, 27]. In contrast, 71% of these patients with macroscopic extension into the portal vein and/or the hepatic veins/vena cava were alive and disease-free more than 10 years after liver transplantation [3]. Pathological examination showed pronounced tumor necrosis, 87%, in the excisional specimens. However, whether we can effectively downstage a tumor by producing extensive tumor necrosis will be an area for future study. A “postembolization syndrome” consisting of fever, abdominal pain, nausea, vomiting, and elevated AST, ALT, and CRP levels occurs in almost all patients, but these symptoms are minimal and transient. Serious adverse effects such as myelosuppression, liver dysfunction, and pulmonary embolism did not occur. Moreover, no evidence of tumor growth or spread before operation was noted. TACE may thus be considered the initial preoperative treatment instead of systemic chemotherapy, especially for patients without distant metastasis, and it may be repeated until the tumor becomes resectable. In addition, we noted that the ranges for AFP in primary reports [4–6, 9, 16] were quite different, making it difficult to interpret any true correlation, but AFP level is a useful aid for monitoring response to TACE and disease recurrence after surgery, in our experience. CT does not predict outcome but, more importantly, serves to monitor treatment, rule out complications, and exclude extrahepatic disease [28].
The mortality and recurrence rates are still high in our series. Five-year EFS was only 43.7 %. Two cases were excited multiple pulmonary metastatic lesions. Although complete surgical resection of the primary tumor was successfully performed, the prognoses were poor. One case had right lobectomy and had no recurrence during the follow-up, but still died of chronic liver function failure. Consequently, we strongly recommend superselective catheterization in order to obtain a better efficacy and cause less damage to residual liver. The tumor size, location, number, feeding vessels, pathological typing, and clinical stage should be carefully evaluated before treatment, and suitable strategy planned individually. In the case of embolus in a portal vein, transarterial infusion of antitumor agents can be performed. Embolotherapy should be approached with caution because of ischemia to the normal liver parenchyma. Furthermore, TACE plays an important role in the primary lesion but has little effect on distal metastasis [5, 29]. Two patients died of distal extensive metastasis in this study, which may be explained by pre-existing micrometastasis. Therefore, postoperative systemic chemotherapy should be used in attempts to eliminate micrometastases that may be present at the time of transplant or malignant cells that are shed during surgical manipulation of the tumor.
There is currently no consensus regarding the timing of TACE in relation to surgery. A short interval makes the operation more difficult, owing to obvious liver capsule edema and lack of clear interspace in anatomic structure. In contrast, if the interval is longer than 6 weeks, the tumor will regrow rapidly because of embolized tumor artery recanalization. On the basis of our experience, TACE was performed one to three times, depending on the patient’s response. Surgical resection was carried out when the tumor volume appeared to be sufficiently reduced to allow safe resection by either lobectomy or extended lobectomy under radiologic criteria. The appropriate time interval between last TACE and operation is about 4 weeks.
OLT offers a chance of cure even to patients in whom HB is otherwise unresectable after chemotherapy [27, 30–32]. We agree that multifocal HB and unifocal, centrally located PRETEXT II and III tumors involving main hilar structures or all three main hepatic veins are clear and undisputed indications for liver transplantation, whatever the result of chemotherapy [17, 18]. However, recurrence is a major cause of mortality after OLT for HB [32, 33]. A recent review of the United Network for Organ Sharing [UNOS] database showed that 54% of deaths after OLT for HB were the result of disease relapse rate [34]. TACE has the potential to control tumor growth during the waiting period and to cause tumor necrosis and reduce tumor dissemination during surgery [6, 35]. Arcement et al. [6] suggest that children who do not respond to systemic therapy can eventually be cured by a combination of TACE and OLT. Majno et al. [36] also found that preoperative TACE could improve the 5-year recurrence-free survival rate for patients with larger tumors. In this study, only one case received OLT after TACE. OLT was considered at this stage but it was not appropriate in any of the patients for various reasons, that is, lack of compliance of the family, shortage of donor organs, high costs of and limited access to the transplantation program, and presence of extrahepatic or metastatic disease. The patient who received OLT died of recurrence 1 year later. We agree that, although OLT is a suitable alternative to chemoembolization in most patients with HB, chemoembolization may also be used in the pretransplantation waiting period.
In conclusion, the optimal strategy for preoperative TACE for HB of infants or children remains controversial. It is difficult to reach any definitive conclusions regarding the role of preoperative TACE based on this study because it was not a multicenter, randomized, control study. Optimal management of this disease requires careful liaison among pediatric oncologists, liver surgeons, radiologists, and histopathologists. Although chemoembolization is a minimally invasive and technically demanding procedure requiring general anesthesia, and is associated with potential complications [37, 38], yyour preliminary experience is encouraging and suggests that TACE is feasible, well tolerated, and effective in inducing surgical resectability of unresectable HB in pediatric patients, which has become an independent palliative or curative therapeutic option, especially for patients without distant metastasis during surgical resection and the pretransplantation waiting period. Further experience and follow-up are necessary to validate this approach.
References
Derek J, Perilongo RG (2006) Hepatoblastoma:an oncological review. Pediatr Radiol 36:183–186
Czauderna P, Otte JB, Roebuck DJ et al (2006) surgical treatment of hepatoblastoma in children. Pediatr Radiol 36:187–191
Brown J, Perilongo G, Shafford E et al (2006) Pretreatment prognostic factors for children with hepatoblastoma. Results from the International Society of Paediatric Oncology (SIOP) Study SIOPEL 1. Eur J Cancer 36:1418–1425
Tashjian DB, Moriarty KP, Courtney RA et al (2002) Preoperative chemombolization for unresectable hepatoblastoma. Pediatr Surg Int 18:187–189
Oue T, Fukuzawa M, Kusafuka T et al (1998) Transcatheter arterial chemoembolization in the treatment of hepatoblastoma. J Pediatr Surg 33:1771–1775
Arcement CM, Towbin RB, Meza MP et al (2000) Intrahepatic chemoembolization in unresectable pediatric liver malignancies. Pediatr Radiol 30:779–785
Ehrlich PF, Greenberg ML, Filler RM et al (1997) Improved long-term survival with preoperative chemotherapy for hepatoblastoma. J Pediatr Surg 32:999–1003
Seo T, Ando H, Watanabe Y et al (1998) Treatment of hepatoblastoma: less extensive hepatectomy after effective preoperative chemotherapy with cisplatin and adriamycin. Surgery 123:407–414
Ohtsuka Y, Matsunaga T, Yoshida H et al (2004) Optimal strategy of preoperative transcatheter arterial chemoembolization for hepatoblastoma. Surg Today 34:127–133
Feusner JH, Krailo MD, Haas JE et al (1993) Treatment of pulmonary metastases of initial stage I hepatoblastoma in childhood. Report from the Children’s Cancer Group. Cancer 71:849
Pritchard J, Brown J, Shafford E et al (2000) Cisplatin, doxorubicin, and delayed surgery for childhood hepatoblastoma: a successful approach—results of the first prospective study of the International Society of Pediatric Oncology. J Clin Oncol 18:3819–3828
Malogolowkin MH, Stanley P, Steele DA et al (2000) Feasibility and toxicity of chemoembolization for children with liver tumors. J Clin Oncol 18(6):1279–1284
Evans AE, Land VJ, Newton WA et al (1982) Combination chemotherapy (vincristine, adriamycin, cyclophosphamide, and 5-fluorouracil) in the treatment of children with malignant hepatoma. Cancer 50:821–826
Farhi DC, Odell CA, Shurin SB (1993) Myelodysplastic syndrome and acute myeloid leukemia after treatment for solid tumors of childhood. Am J Clin Pathol 100:270–275
Moppet J, Oakhill A, Duncan AW (2001) Second malignancies in children: The usual suspects? Eur J Radiol 38:325–348
Vogl TJ, Scheller A, Jakob U et al (2006) Transarterial chemoembolization in the treatment of hepatoblastoma in children. Eur Radiol 16(6):1393–1396
Otte JB, Goyet JV, Reding R (2005) Liver transplantation for hepatoblastoma: indications and contraindications in the modern era. Pediatr Transpl 9:557–565
Aronson D, Schnater JM, Staalman C et al (2005) The predictive value of the PREtreatment EXTent of disease (PRETEXT) system in hepatoblastoma: results from the international Society of Pediatric Oncology Liver Tumor Study Group (SIOPEL-1). J Clin Oncol 23:1245–1252
Katzenstein HM, Londo WB, Douglass EC et al (2002) Treatment of unresectable and metastatic hepatoblastoma: a Pediatric Oncology Group Phase II study. J Clin Oncol 20:3438–3444
Takayama T, Makuuchi M, Takayasu K et al (1990) Resection after intraarterial chemotherapy of a hepatoblastoma originating in the caudal lobe. Surgery 107:231–235
Yokomori K, Hori T, Asoh S et al (1991) Complete disappearance of unresectable hepatoblastoma by continuous infusion therapy through hepatic artery. J Pediatr Surg 26:844–846
Fan J, Tang ZY, Yu YQ et al (1998) Improved survival with resection after transcatheter arterial embolization (TACE) for unresectable hepatocellular carcinoma. Dig Surg 15(6):674–678
Trinchet JC, Rached AA, Beaugrand M et al (1995) A comparison of lipiodol chemoembolization and conservative treatment for unresectable hepatocellular carcinoma. N Engl J Med 332:1256–1261
Gattoni F, Cornalba G, Brambilla G et al (1998) Survival of 184 patients with hepatocellular carcinoma in cirrhotic liver treated with chemoembolization: a multicentric study. Radiol Med 95:362–368
Liovet JM, Real MI, Montana X et al (2002) Arterial embolization or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomized controlled trial. Lancet 359:1734–1739
Chou FI, Fang KC, Chung C et al (1995) Lipiodol uptake and retention by human hepatoma cells. Nucl Med Biol 22(3):379–386
Otte JB, Pritchard J, Aronson DC et al (2004) Liver transplantation for hepatoblastoma: results from the International Society of Pediatric Oncology (SIOP) study SIOPEL-1 and review of the world experience. Pediatr Blood Cancer 42:74–83
King SJ, Babyn PS, Greenberg ML et al (1993) Value of CT in determining the resectability of hepatoblastoma before and after chemotherapy. AJR 160:793–798
Dicken BJ, Bigam DL, Lees GM (2004) Association between surgical margins and long-term outcome in advanced hepatoblastoma. J Pediatr Surg 39:721–725
Srinivasan P, McCall J, Pritchard J et al (2002) Orthotropic liver transplantation for unresectable hepatoblastoma. Transplantation 74:652–655
Reyes JD, Carr B, Dvorchik I et al (2000) Liver transplantation and chemotherapy for hepatoblastoma and hepatocellular cancer in childhood and adolescence. J Pediatr 136:795–804
Superina R, Bilik R (1996) Results of liver transplantation in children with unresectable liver tumors. J Pediatr Surg 31:835–839
Pimpalwar AP, Sharif K, Ramani P et al (2002) Strategy for hepatoblastoma management:transplant versus nontransplant surgery. J Pediatr Surg 37:240–245
Austin MT, Leys CM, Feurer ID et al (2006) Liver transplantation for childhood hepatic malignancy: a review of the United Network for Organ Sharing (UNOS) database. J Pediatr Surg 41:182–186
Roayaie S, Frische JS, Emre SH et al (2002) Long-term results with multimodal adjuvant therapy and liver transplantation for the treatment of hepatocellular carcinomas larger than 5 centimeters. Ann Surg 235(4):533–539
Majno PE, Adam R, Bismuth H et al (1997) Influence of preoperative transarterial lipiodol chemoembolization on resection and transplantation for hepatocellular carcinoma in patients with cirrhosis. Ann Surg 226(6):688–703
Chung JW, Park JH, Han JK et al (1996) Hepatic tumors: predisposing factors for complications of transcatheter oily chemoembolization. Radiology 198:33–40
Yamaura K, Higashi M, Akiyoshi Y et al (2000) Pulmonary lipiodol embolism during transcatheter arterial chemoembolization for hepatoblastoma under general anesthesia. Eur J Anaesth 17:704–708
Acknowledgments
We express our gratitude to all members of the Department of Interventional Radiology and to Dr. Tangbin Liu and Dr. Guisheng Li of the Department of Pediatrics.
Author information
Authors and Affiliations
Corresponding author
Additional information
The abstract of this paper was presented at the RSNA meeting (2006).
Rights and permissions
About this article
Cite this article
Li, Jp., Chu, Jp., Yang, Jy. et al. Preoperative Transcatheter Selective Arterial Chemoembolization in Treatment of Unresectable Hepatoblastoma in Infants and Children. Cardiovasc Intervent Radiol 31, 1117–1123 (2008). https://doi.org/10.1007/s00270-008-9373-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-008-9373-x