Abstract
The purpose of our study was to determine if preferential radiographic tumor response occurs in tumors located in posterior versus anterior liver segments following radioembolization with yttrium-90 glass microspheres. One hundred thirty-seven patients with chemorefractory liver metastases of various primaries were treated with yttrium-90 glass microspheres. Of these, a subset analysis was performed on 89 patients who underwent 101 whole-right-lobe infusions to liver segments V, VI, VII, and VIII. Pre- and posttreatment imaging included either triphasic contrast material-enhanced CT or gadolinium-enhanced MRI. Responses to treatment were compared in anterior versus posterior right lobe lesions using both RECIST and WHO criteria. Statistical comparative studies were conducted in 42 patients with both anterior and posterior segment lesions using the paired-sample t-test. Pearson correlation was used to determine the relationship between pretreatment tumor size and posttreatment tumor response. Median administered activity, delivered radiation dose, and treatment volume were 2.3 GBq, 118.2 Gy, and 1,072 cm3, respectively. Differences between the pretreatment tumor size of anterior and posterior liver segments were not statistically significant (p = 0.7981). Differences in tumor response between anterior and posterior liver segments were not statistically significant using WHO criteria (p = 0.8557). A statistically significant correlation did not exist between pretreatment tumor size and posttreatment tumor response (r = 0.0554, p = 0.4434). On imaging follow-up using WHO criteria, for anterior and posterior regions of the liver, (1) response rates were 50% (PR = 50%) and 45% (CR = 9%, PR = 36%), and (2) mean changes in tumor size were −41% and −40%. In conclusion, this study did not find evidence of preferential radiographic tumor response in posterior versus anterior liver segments treated with yttrium-90 glass microspheres.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the western hemisphere, hematogenous spread of cancer is the most common cause of hepatic malignancies. The incidence is 18–20 times that of primary liver cancer [1]. The dual blood supply coupled with the expression of humoral factors that promote cellular growth provides a suitable milieu for malignant seeding. Since the portal vein drains the abdominal viscera, it then serves as the preferred conduit for the transmigration of cancer cells from primary gastrointestinal cancers.
Radioembolization using yttrium-90 (Y90) has gained recognition for achieving excellent tumor responses while maintaining a minimal toxicity profile. This is a minimally invasive procedure in which arterial catheter placement is used to infuse microspheres containing the radioactive isotope Y90 into tumor feeding arteries. This locoregional therapy has been shown to be safe and effective in treating patients with primary and secondary liver malignancies [2–7]. As with all liver-directed intra-arterial therapies, this therapy takes advantage of the dual blood supply to the liver. Eighty percent of hepatic tissue derives its blood supply from the portal vein, whereas liver tumors are preferentially supplied by the arterial system [8, 9]. Embolotherapy using radioactive microspheres has emerged as a method to deliver tumoricidal doses of radiation directly into the neoplastic microvasculature while concomitantly sparing normal parenchyma [10].
Currently, two commercial products using Y90 microspheres are available as delivery devices—one uses resin-based microspheres and the other uses glass-based microspheres [11]. Although both types of microspheres contain Y90 as the radioactive isotope, the two products have significant characteristic differences [12, 13]. The specific gravity of glass microspheres is two times that of resin microspheres (3.2 versus 1.6 mg/cm3) and may theoretically settle in the dependent regions of the liver. In settling in the dependent regions of the liver, nondependent tumors may achieve a less favorable tumor response [14]. As a result of gravitational and dependent flow we postulate that glass microspheres will preferentially deposit, and therefore have a superior radiographic response, in posterior segment tumors. In order to test this hypothesis, we compare the radiographic tumor response in lesions located in the anterior segments (V, VIII) versus posterior segments (VI, VII) in patients who received whole-right-lobe treatments with Y90 glass microspheres.
Materials and Methods
Patients
This open-label cohort study was approved by our institutional review board, and signed informed consent was obtained from all patients. Between 2002 through 2006, 137 patients with progressing secondary liver malignancies were prospectively enrolled and treated [15]. Of these, 89 patients were identified as having either solitary or multifocal right lobe tumors necessitating whole-right-lobe treatments. All patients underwent pre-and posttreatment diagnostic imaging with either computed tomography (CT) or gadolinium-enhanced magnetic resonance imaging (MRI) of the abdomen. Treatments were directed to hepatic segments V, VI, VII, and VIII via the right hepatic artery. The rationale for evaluating right lobe tumors is that, in the supine position, infusion of microspheres via the hepatic artery permits the effects of dependent flow (gravity) to be maximized. As a result, imaging response differences between anterior (V, VIII) and posterior (VI, VII) segment lesions may be compared.
Patient eligibility for treatment included (i) chemorefractory or progressive liver-dominant metastases; (ii) unresectable disease; (iii) Eastern Cooperative Oncology Group (ECOG) score 0–2; (iv) noncompromised pulmonary function test; (v) able to undergo angiography and selective visceral catheterization; (vi) adequate hematology (granulocyte count ≥ 1.5 × 109/L, platelets ≥ 50 × 109/L) and renal function (creatinine ≤ 2.0 mg/dl); (vii) liver function (bilirubin ≤ 2.0 mg/dl); and (viii) limited extrahepatic disease deemed clinically insignificant by the referring physician. Patients were deemed ineligible and excluded from the study based on the following criteria: (i) any other liver therapy planned for their cancer; (ii) significant extrahepatic disease with an expected mortality of <2 months; (iii) liver failure (bilirubin > 2.0 mg/dl); (iv) hepatogastrointestinal shunting uncorrectable by catheter techniques; and (v) estimated radiation doses to the lungs exceeding 30 Gy in a single administration or cumulative 50 Gy over successive treatments [16]. For the purpose of this subset analyses, only right-lobe infusions with corresponding lesions in segments V, VI, VII, and VIII are reported.
Y90 Device
Therasphere 90Y microspheres (MDS Nordion, Ottawa, ON, Canada) are approved under a Humanitarian Device Exemption for the treatment of unresectable hepatocellular carcinoma (HCC) [12]. It recently received approval for its use in patients with partial or branch portal vein thrombosis (PVT), as a bridge to transplantation and neoadjuvant to surgery [11]. It is also approved for the treatment of liver neoplasia in Europe and Canada. It is composed of nonbiodegradable microsphere with Y90 as an integral constituent of the glass. The microsphere diameter ranges from 25 to 35 μm. Y90 is a pure β-emitter with an estimated half-life of 64.2 h, after which it decays to stable zirconium (90Zr). The average energy of β-emissions is 0.9367 MeV, with a mean tissue penetrating range between 2.5 and 10 mm. One gigabecquerel (27 mCi) of 90Y per kilogram of tissue provides a dose of 50 Gy. In brief, CT or MR imaging is used to determine the targeted liver volume to be treated with 90Y microspheres [2, 6, 17–19]. The targeted liver volume is that portion of liver tissue that will be treated once the catheter is in the desired location. A conversion factor of 1.03 g/cm3 is used to calculate the corresponding targeted liver mass from the targeted liver volume. The required activity is calculated from the following formula:
[18]. When lung shunt fraction (LSF) and percentage of residual activity (R) in the vial after treatment are taken into account, the actual dose delivered to the target mass is calculated by rearranging the previous equation as follows:
[18]. Cumulative liver dose is defined as the accumulated dose to that specific volume that was treated multiple times. By targeting delivery to a hepatic segment or lobe, 90Y therapy results in high radiation doses to the tumor while sparing normal liver parenchyma. These tumoricidal doses have proven effective in the ability of 90Y microspheres to reduce tumor viability, demonstrating an increasing therapeutic effect with radiation dose [6].
Pre- and Postprocedural Evaluation
All eligible patients underwent standard Y90 assessment before treatment initiation. This included (i) a complete medical history and physical examination; (ii) pretreatment serologic evaluation of hematologic, renal, and hepatic panels; (iii) triple-phase contrast material-enhanced CT or gadolinium-enhanced MRI of the liver; (iv) liver angiography with selective visceral catheterization; (v) a 99mTc macroaggregated albumin (MAA) scan to determine the presence and extent of hepatopulmonary shunting; and (vi) when necessary, embolization of gastroduodenal vessels to prevent the adverse effects of nontarget radiation [5]. Imaging studies were reviewed prior to treatment to document the extent of tumor and its location, assess vascular anatomy, determine if the portal vein is patent, and measure liver volumes for dosimetry calculations.
Patients returned to the interventional radiology suite on a later date for Y90 liver-directed therapy. Using standard catheter techniques, a 3-Fr microcatheter was introduced percutaneously and advanced into the right hepatic artery (RHA), where the calculated dose and predetermined activity was infused into the right hepatic artery, specifically targeting tumors of the right lobe. Postprocedurally, patients were monitored in the recovery room for a period of 2–6 h before being discharged in stable condition. Patients were followed in clinic at 4 weeks and then every 3 months. Serial serologic studies including complete blood counts, renal function tests, and liver function tests were documented at each follow-up visit.
Data Collection
The following parameters were calculated: (i) median activity and dose; (ii) median lobar volume; (iii) median pretreatment tumor size; and (iv) mean change in tumor response (defined as percentage change from baseline lesion). Lesions were then categorized: (a) complete response (CR); (b) partial response (PR); (c) stable disease (SD); or (d) progressive disease (PD). Standard imaging follow-up was utilized. Posttreatment studies were compared to baseline studies by four board-certified radiologists utilizing CT or MRI. Assessment of tumor response was performed at 1 month and every subsequent 3 months following therapy. Response Evaluation Criteria in Solid Tumors (RECIST) and World Health Organization (WHO) criteria were used in determining the radiographic tumor response to treatment. Tumor response by WHO criteria was determined by taking the sum of the cross products of the longest diameter and its perpendicular distance. WHO responses were categorized as follows: (i) CR was defined as a decrease in the cross product to zero (i.e., complete disappearance of tumor); (ii) PR was noted with a decrease in the cross product by >50%; (iii) PD was categorized by an increase in the cross product by >25%; and (iv) SD was considered a size between that for PR and that for SD. RECIST was calculated by measuring the sum of the longest diameter of the target lesions [20]. RECIST criteria were defined as follows: (i) CR was the disappearance of the target lesion; (ii) PR was categorized as at least a 30% decrease in the longest diameter of the target lesion; (iii) PD was noted with at least a 20% increase in the longest diameter; and (iv) and SD was considered for tumors measuring a size between that for PR and that for SD.
Statistical Analyses
For the primary statistical study, 42 treated patients with demonstrable tumor masses in both anterior and posterior segments of the right lobe were identified. Pretreatment tumor size of anterior segment lesions were compared to that of posterior segment lesions using the two-tailed t-test for paired samples. On further analysis of this cohort, the 42 patients were stratified into three distinct groups based on the primary malignancy: (I) colorectal, (II) neuroendocrine, and (III) noncolorectal, nonneuroendocrine (NCNN). Tumor response between anterior and posterior segments were compared for this entire cohort (n = 42) and for each of the three primary tumor groups. Tumor response comparisons between anterior and posterior segments were conducted using the two-tailed t-test for paired samples. Pearson correlation coefficient was used to evaluate the relationship between pretreatment tumor size and posttreatment tumor response. All statistical tests were performed using MedCalc version 9.3.9 for Windows (MedCalc Software, Mariakerke, Belgium).
Results
Patient Demographics
There were 41 men and 48 women. Median age was 63 years (range, 31–89 years). Primary sites of malignancy were colon (n = 36), breast (n = 14), neuroendocrine (n = 9), lung (n = 4), cholangiocarcinoma (n = 3), renal (n = 3), adenocarcinoma of unknown origin (n = 3), and others (n = 17). The ECOG performance statuses at baseline were 0, 1, and 2 in 56, 25, and 8 patients, respectively. Ten and 79 patients had unilobar and bilobar disease, respectively. Four, 65, and 20 patients had disease occupying 0–25%, 26–50%, and >51% of their liver, respectively. Figures 1 and 2 graphically summarize the distribution of anterior and posterior pretreatment tumor sizes. The median size of all tumors (n = 193), as measured by RECIST, was 3.1 cm (range, 0.7–13.8 cm; 95% CI, 2.8–3.5).
Treatment and Radiation Dose
Eighty-nine patients successfully underwent a total of 101 whole-right-lobe (segments V, VI, VII, VIII) administrations of Y90 glass microspheres. All patients tolerated the procedure on an outpatient basis and were discharged within 2–6 h postprocedurally. The median administered activity (corrected for shunt, residual, and decay), delivered radiation dose, and treatment volume were 2.3 GBq, 118.2 Gy, and 1,072 cm3, respectively.
Comparative Statistical Outcomes
Comparative statistical studies were carried out for the 42 patients with tumor masses in both anterior and posterior segments of the right hepatic lobe. There were no statistically significant differences between the pretreatment tumor size of lesions in anterior (mean, 3.40 cm; 95% CI, 2.54–4.26) versus posterior (mean, 3.27 cm; 95% CI, 2.40–4.14) segments (p = 0.7981). Tables 1 and 2 summarize the tumor response by RECIST and WHO criteria for the 42 patients. No statistically significant differences were detected between anterior and posterior segment tumor responses in all analyses. Table 3 further classifies the Y90-induced tumor response by CR, PR, SD, and PD using both RECIST and WHO criteria.
Imaging Response of All Lesions
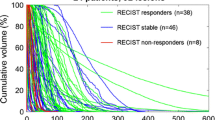
Tumor response classified by CR, PR, SD, and PD for all lesions (n = 193), using RECIST and WHO criteria, are summarized in Table 4. Figures 1 and 2 displays the pretreatment tumor sizes for anterior (n = 97) and posterior (n = 96) segments in a histogram. Figures 3 and 4 present waterfall plots of Y90-induced tumor responses for all anterior (n = 97) and posterior (n = 96) segment lesions. Table 5 summarizes the mean change in tumor size for all lesions stratified by primary tumor type.
Imaging response using RECIST is presented as a waterfall plot. Bar values demonstrate maximum change in tumor size from baseline in 193 lesions following Y90 glass microsphere therapy. Anterior segment responses are superimposed onto posterior segment responses, demonstrating similar trends of responses
Imaging response using WHO criteria is presented as a waterfall plot. Bar values demonstrate maximum change in tumor size from baseline in 193 lesions following Y90 glass microsphere therapy. Anterior segment responses are superimposed onto posterior segment responses, demonstrating similar trends of responses
Statistical Correlation Between Tumor Size and Tumor Response
Results from the correlative study suggest that no significant relationship between pretreatment tumor size and posttreatment tumor response exists (r = 0.0554, p = 0.4434). Figure 5 displays pretreatment tumor size versus posttreatment tumor response in a scatter diagram.
Discussion
We report the radiographic tumor response of 193 hepatic metastatic lesions in 89 patients following whole-right-lobe administrations of radioactive Y90 glass microspheres. From within this cohort, 42 patients with metastatic lesions in both anterior and posterior segments of the right lobe were statistically evaluated for differences in tumor response. By RECIST and WHO criteria, there were no significant differences between the mean change in tumor size in anterior versus posterior segments. Using RECIST for all measured lesions (n = 193), the mean change in tumor size for anterior and posterior lesions were −23% and −24%, respectively. Similarly, using WHO criteria for all measured lesions (n = 193), mean change in tumor size for anterior and posterior lesions were −36% and −38%, respectively.
The basis underlying radioembolization for liver malignancies is the differential arterial perfusion between cancerous and normal tissue. Given that normal liver parenchyma is primarily supplied by the portal vein and neoplasms both native and metastatic to the liver derive blood through the arterial conduits, radioembolic therapies exploiting this difference have effectively targeted tumor without adversely affecting noncancerous liver tissue. Various investigators have shown microspheres depositing preferentially around the periphery of the tumor with minimal distribution to normal hepatic tissue [21–23]. Although the exact mechanism of the uptake remains unclear, it is believed that the hypervascularity of tumor preferentially directs the microspheres into its vascular bed.
Given that glass microspheres are denser than the 99mTc MAA particles used at preplanning angiography, a theoretical concern has been its distribution and tumor coverage when used for treatment purposes [24, 25]. There has also been some speculation about the higher likelihood of glass microspheres refluxing into the gastrointestinal supplying vasculature [26, 27]. Additionally, there has been informal debate regarding glass microspheres accumulating in the dependent (i.e., posterior segments VI and VII) regions of the liver, given its specific gravity.
The suggestion that use of glass microspheres results in suboptimal tumor coverage has not been demonstrated. Histopathologic studies have found a disproportionate accumulation of 90Y microspheres embedded within the tumor arteriolar bed [28]. Kennedy et al. analyzed the microsphere distribution in four explanted livers treated with either radioactive glass or resin [23]. The authors observed that both glass and resin microspheres dispersed in a preferential and heterogeneous manner along the periphery of the tumor, although there was still some speculation about glass possibly accumulating the in the dependent regions. In 2001, Araki et al. reported on the distribution of nonradioactive glass microspheres following its intrarenal artery infusion in animal kidneys [29]. On postprocedural microscopic imaging, glass microspheres were found in the renal afferent arterioles and uniformly distributed in the renal cortices. Other studies have also correlated the distribution of microspheres with blood flow [30].
Although there have been no direct comparisons between the efficacies of the two Y90 devices, Wong et al. reported on 46 patients with metastatic liver disease who were treated with either glass (n = 27) or resin-based (n = 19) microspheres [31]. The use of either device resulted in a statistically significant standard uptake value (SUV) change on PET. There were also no differences in the mean percentage reduction of tumor metabolism between the two agents (p = 0.38), suggesting no significant difference in tumor response between the two devices. The authors concluded that Y90 microspheres, irrespective of agent used, resulted in a significant mean reduction in tumor load.
The posttherapeutic gastrointestinal complications reported in the literature are likely related to the inadvertent deposition (e.g., unrecognized gastric vessels, underembolization of extrahepatic vessels, operator error) of microspheres into the extrahepatic visceral branches of the gastrointestinal tract, and not the physical characteristics of either device. A previous assumption that glass microspheres have a higher likelihood of refluxing into the gastrointestinal circulation has never been validated. Although resin microspheres have a similar density profile relative to the pretreatment planning 99mTc MAA and should theoretically mimic its distribution pattern, gastrointestinal ulcerations continue to be reported [32–45]. Murthy et al. reported on the gastrointestinal complications associated with Y90 radioembolization [46]. The authors attributed the complication to unrecognized variants, operator error, collateral circulation, and changes in flow dynamics during infusion.
The study reported herein was designed to test the hypothesis of dependent flow of glass microspheres. Since we were unable to quantify glass microsphere deposition at the arteriolar level, we used the differential tumor response in the anterior and posterior segments as a surrogate. To test this hypothesis, we carried out two separate statistical analyses. In order to eliminate interpatient variability and to account for the heterogeneity of the tumors, the statistical analyses were carried out in only those patients with lesions in both anterior and posterior segments.
There were no statistically significant differences between the pretreatment and posttreatment tumor response in 42 patients with lesions in both anterior and posterior segments of the right lobe. Given that the radiosensitivity of tumors vary widely among different types of cancers, we further analyzed these patients by stratifying them into three categories: (i) colorectal; (ii) neuroendocrine; and (iii) noncolorectal, nonneuroendocrine (NCNN). The induced tumor responses did not differ between anterior and posterior tumors for any cancer type. Tables 1 and 2 summarize these findings. Table 3 categorizes the tumor responses into CR, PR, SD, and PD for the 42 patients.
To gain further insight, we evaluated 193 discrete metastatic lesions of the liver. Ninety-seven anterior (segments V and VIII) and 96 posterior (segments VI and VII) posttreatment tumor responses were categorized into response categories using both RECIST and WHO criteria. Table 4 summarizes these findings. The results demonstrate similar tumor response trends for both anterior and posterior segment tumors. Additionally, the results suggest that, irrespective of lesion size, heterogeneity of the primary lesion, or location of the metastatic lesions, whole-right-lobe treatments with glass microspheres results in preferential distribution of the microparticles to areas of the highest vascularity (i.e., tumor). This study does not find evidence of a preferential tumor response for metastatic lesions confined to the posterior liver segments. Our findings further support the published 30–50% PR rates consistently demonstrated with use of either glass or resin microspheres [47].
There were several important limitations to our study. First, this was a heterogeneous sample treated under an open-label cohort study, limiting the ability to generalize findings. Second, tumor heterogeneity was not fully accounted for in our analyses, tumors by primary tumor type were limited to colorectal, neuroendocrine, and NCNN. Third, tumor responses were assessed using RECIST and WHO criteria only. The response rates may have been different had we utilized other classification schemes such as European Association for the Study of the Liver (EASL) recommendations [48]. Fourth, these findings were carried out using glass microspheres (3.2 mg/cm3), and therefore the results may not be extrapolated to microspheres of higher density. Finally, this study represents the experience from a single tertiary care center and warrants further independent investigation.
Conclusion
Although we acknowledge that dependent flow exists, we did not find evidence of preferential radiographic tumor response in posterior versus anterior hepatic metastatic lesions following whole-right-lobe treatments with Y90 glass microspheres. Our findings do not support the assumption that radioactive glass microsphere infusions result in suboptimal tumor coverage. Flow dynamics and hypervascularity, rather than the particle density of glass microspheres, appear to be significant predictors of therapeutic effectiveness.
References
Bartolozzi C (ed) (2003) Liver malignancies, 1st edn. Springer, New York
Carr BI (2004) Hepatic arterial 90Yttrium glass microspheres (therasphere) for unresectable hepatocellular carcinoma: interim safety and survival data on 65 patients. Liver Transpl 10:S107–S110
Geschwind JF, Salem R, Carr BI et al (2004) Yttrium-90 microspheres for the treatment of hepatocellular carcinoma. Gastroenterology 127:S194–S205
Gray B, Van Hazel G, Hope M et al (2001) Randomised trial of SIR-Spheres plus chemotherapy vs. chemotherapy alone for treating patients with liver metastases from primary large bowel cancer. Ann Oncol 12:1711–1720
Lewandowski RJ, Sato KT, Atassi B et al (2007) Radioembolization with (90)y microspheres: angiographic and technical considerations. CardioVasc Interv Radiol 30:571–592
Salem R, Lewandowski RJ, Atassi B et al (2005) Treatment of unresectable hepatocellular carcinoma with use of 90Y microspheres (therasphere): safety, tumor response, and survival. J Vasc Interv Radiol 16:1627–1639
Van Hazel G, Blackwell A, Anderson J et al (2004) Randomised phase 2 trial of SIR-Spheres plus fluorouracil/leucovorin chemotherapy versus fluorouracil/leucovorin chemotherapy alone in advanced colorectal cancer. J Surg Oncol 88:78–85
Breedis C, Young G (1954) The blood supply of neoplasms in the liver. Am J Pathol 30:969–977
Lien WM, Ackerman NB (1970) The blood supply of experimental liver metastases. II. A microcirculatory study of the normal and tumor vessels of the liver with the use of perfused silicone rubber. Surgery 68:334–340
Murthy R, Nunez R, Szklaruk J et al (2005) Yttrium-90 microsphere therapy for hepatic malignancy: devices, indications, technical considerations, and potential complications. Radiographics 25(Suppl 1):S41–S55
Nordion MDS (2004) Therasphere Yttrium-90 microspheres package insert. MDS Nordion, Kanata, Canada
Salem R, Thurston KG (2006) Radioembolization with 90yttrium microspheres: a state-of-the-art brachytherapy treatment for primary and secondary liver malignancies. Part 1: technical and methodologic considerations. J Vasc Interv Radiol 17:1251–1278
Welsh JS, Kennedy AS, Thomadsen B (2006) Selective internal radiation therapy (SIRT) for liver metastases secondary to colorectal adenocarcinoma. Int J Radiat Oncol Biol Phys 66:S62–S73
Welsh JS (2007) Radiographically identified necrosis after 90Y microsphere brachytherapy: a new standard for oncologic response assessment? AJR 188:765–767
Sato KT, Lewandowski RJ, Mulcahy MF, Atassi B, Ryu RK, Gates VL, Nemcek AA, Jr., Barakat O, Benson A, III, Mandal R, Talamonti M, Wong CY, Miller FH, Newman SB, Shaw JM, Thurston KG, Omary RA, Salem R (2008) Unresectable chemorefractory liver metastases: radioembolization with 90Y microspheres–safety, efficacy, and survival. Radiology 247:507–515
Lewandowski RJ, Thurston KG, Goin JE et al (2005) 90Y microsphere (therasphere) treatment for unresectable colorectal cancer metastases of the liver: response to treatment at targeted doses of 135–150 Gy as measured by [18F]fluorodeoxyglucose positron emission tomography and computed tomographic imaging. J Vasc Interv Radiol 16:1641–1651
Dancey JE, Shepherd FA, Paul K et al (2000) Treatment of nonresectable hepatocellular carcinoma with intrahepatic 90Y-microspheres. J Nucl Med 41:1673–1681
Salem R, Thurston KG, Carr BI, Goin JE, Geschwind JF (2002) Yttrium-90 microspheres: radiation therapy for unresectable liver cancer. J Vasc Interv Radiol 13:S223–S229
Russell JL, Carden JL, Herron HL (1988) Dosimetry calculations for yttrium-90 used in the treatment of liver cancer. Endocuriether/Hypertherm Oncol 4:171–186
Therasse P, Arbuck SG, Eisenhauer EA et al (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Campbell AM, Bailey IH, Burton MA (2000) Analysis of the distribution of intra-arterial microspheres in human liver following hepatic yttrium-90 microsphere therapy. Phys Med Biol 45:1023–1033
Campbell AM, Bailey IH, Burton MA (2001) Tumour dosimetry in human liver following hepatic yttrium-90 microsphere therapy. Phys Med Biol 46:487–498
Kennedy AS, Nutting C, Coldwell D, Gaiser J, Drachenberg C (2004) Pathologic response and microdosimetry of (90)Y microspheres in man: review of four explanted whole livers. Int J Radiat Oncol Biol Phys 60:1552–1563
Helmberger TK (2007) Percutaneous tumor ablation in medical radiology, 1st edn. Springer, Berlin/Heidelberg
Ho S, Lau JW, Leung TW (2001) Intrahepatic (90)Y-microspheres for hepatocellular carcinoma. J Nucl Med 42:1587–1589
Herba MJ, Illescas FF, Thirlwell MP et al (1988) Hepatic malignancies: improved treatment with intraarterial Y-90. Radiology 169:311–314
Ho S, Lau WY, Leung TW, Johnson PJ (1998) Internal radiation therapy for patients with primary or metastatic hepatic cancer: a review. Cancer 83:1894–1907
Kulik LM, Atassi B, van Holsbeeck L et al (2006) Yttrium-90 microspheres (therasphere(R)) treatment of unresectable hepatocellular carcinoma: downstaging to resection, RFA and bridge to transplantation. J Surg Oncol 94:572–586
Araki N, Nagata Y, Fujiwara K et al (2001) Evaluation of glass microspheres for intra-arterial radiotherapy in animal kidneys. Int J Radiat Oncol Biol Phys 49:459–463
Beck KC (1987) Regional trapping of microspheres in the lung compares well with regional blood flow. J Appl Physiol 63:883–889
Wong CY, Savin M, Sherpa KM et al (2006) Regional yttrium-90 microsphere treatment of surgically unresectable and chemotherapy-refractory metastatic liver carcinoma. Cancer Biother Radiopharm 21:305–313
Herba MJ, Thirlwell MP (2002) Radioembolization for hepatic metastases. Semin Oncol 29:152–159
Lim L, Gibbs P, Yip D et al (2005) Prospective study of treatment with selective internal radiation therapy spheres in patients with unresectable primary or secondary hepatic malignancies. Intern Med J 35:222–227
Neff R, Abdel-Misih R, Khatri J et al (2008) The toxicity of liver directed yttrium-90 microspheres in primary and metastatic liver tumors. Cancer Invest 26:173–177
Popperl G, Helmberger T, Munzing W, Schmid R, Jacobs TF, Tatsch K (2005) Selective internal radiation therapy with SIR-Spheres in patients with nonresectable liver tumors. Cancer Biother Radiopharm 20:200–208
Kennedy AS, Coldwell D, Nutting C, Murthy R, Wertman DE Jr, Loehr SP, Overton C, Meranze S, Niedzwiecki J, Sailer S (2006) Resin 90Y-microsphere brachytherapy for unresectable colorectal liver metastases: modern USA experience. Int J Radiat Oncol Biol Phys 65:412–425
Lau WY, Ho S, Leung TW, Chan M, Ho R, Johnson PJ, Li AK (1998) Selective internal radiation therapy for nonresectable hepatocellular carcinoma with intraarterial infusion of 90yttrium microspheres. Int J Radiat Oncol Biol Phys 40:583–592
Lau WY, Leung WT, Ho S, Leung NW, Chan M, Lin J, Metreweli C, Johnson P, Li AK (1994) Treatment of inoperable hepatocellular carcinoma with intrahepatic arterial yttrium-90 microspheres: a phase I and II study. Br J Cancer 70:994–999
Murthy R, Xiong H, Nunez R, Cohen AC, Barron B, Szklaruk J, Madoff DC, Gupta S, Wallace MJ, Ahrar K, Hicks ME (2005) Yttrium 90 resin microspheres for the treatment of unresectable colorectal hepatic metastases after failure of multiple chemotherapy regimens: preliminary results. J Vasc Interv Radiol 16:937–945
Popperl G, Helmberger T, Munzing W, Schmid R, Jacobs TF, Tatsch K (2005) Selective internal radiation therapy with SIR-Spheres in patients with nonresectable liver tumors. Cancer Biother Radiopharm 20:200–208
Stubbs RS, Cannan RJ, Mitchell AW (2001) Selective internal radiation therapy (SIRT) with 90Yttrium microspheres for extensive colorectal liver metastases. Hepato-gastroenterology 48:333–337
Stubbs RS, Cannan RJ, Mitchell AW (2001) Selective internal radiation therapy with 90yttrium microspheres for extensive colorectal liver metastases. J Gastrointest Surg 5:294–302
Van Hazel G, Blackwell A, Anderson J, Price D, Moroz P, Bower G, Cardaci G, Gray B (2004) Randomised phase 2 trial of SIR-Spheres plus fluorouracil/leucovorin chemotherapy versus fluorouracil/leucovorin chemotherapy alone in advanced colorectal cancer. J Surg Oncol 88:78–85
Yip D, Allen R, Ashton C, Jain S (2004) Radiation-induced ulceration of the stomach secondary to hepatic embolization with radioactive yttrium microspheres in the treatment of metastatic colon cancer. J Gastroenterol Hepatol 19:347–349
Stubbs RS, O’Brien I, Correia MM (2006) Selective internal radiation therapy with 90Y microspheres for colorectal liver metastases: single-centre experience with 100 patients. ANZ J Surg 76:696–703
Murthy R, Brown DB, Salem R et al (2007) Gastrointestinal complications associated with hepatic arterial yttrium-90 microsphere therapy. J Vasc Interv Radiol 18:553–561; quiz 562
Salem R, Thurston KG (2006) Radioembolization with yttrium-90 microspheres: a state-of-the-art brachytherapy treatment for primary and secondary liver malignancies. Part 3: comprehensive literature review and future direction. J Vasc Interv Radiol 17:1571–1593
Bruix J, Sherman M, Llovet JM et al (2001) Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL conference. European Association for the Study of the Liver. J Hepatol 35:421–430
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: R.S. is a consultant for MDS Nordion and has disclosed a potential conflict of interest. None of the other authors have disclosed a conflict. The data were controlled by all authors. No industry support for this study was provided.
Rights and permissions
About this article
Cite this article
Ibrahim, S.M., Lewandowski, R.J., Ryu, R.K. et al. Radiographic Response to Yttrium-90 Radioembolization in Anterior Versus Posterior Liver Segments. Cardiovasc Intervent Radiol 31, 1124–1132 (2008). https://doi.org/10.1007/s00270-008-9348-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-008-9348-y