Abstract
The aim of this study was to show the feasibility, safety, imaging appearance, and short-term efficacy of image-guided percutaneous radiofrequency ablation (RFA) of adrenal metastases (AM). Seven imaging-guided percutaneous RFA treatments were performed in six patients (two men and four women; mean age, 67.2 years; range, 55–74 years) with six AM who were referred to our institution from 2003 to 2006. One patient was treated twice for recurrence after first treatment. The average diameter of the treated AM was 29 mm (range, 15–40 mm). In all patients, the diagnosis was obtained with CT current protocols in use at our institution and confirmed by pathology with an image-guided biopsy. No major complications occurred. In one patient shortly after initiation of the procedure, severe hypertension was noted; another patient developed post-RFA syndrome. In five of six lesions, there was no residual enhancement of the treated tumor. In one patient CT examination showed areas of residual enhancement of the tumor after treatment. Our preliminary results suggest that imaging-guided percutaneous RFA is effective for local control of AM, without major complications and with a low morbidity rate related to the procedure. Long-term follow-up will need to be performed and appropriate patient selection criteria will need to be determined in future randomized trials.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The adrenal gland is a common site of metastases [1–3]. Adrenal metastases (AM) have been the subject of only a few studies, however, their optimal treatment remains unclear. Chemotherapy with mitotane has shown limited efficacy, and radiation therapy has little significant effect on the natural course of this disease [1–4]. Various methods of managing this condition have been tried, including surgical resection [5], transarterial chemoembolization (TACE) [6, 7], percutaneous ethanol injection and acetic acid injection [8–12], and external-beam radiation therapy [13].
Surgical resection for an isolated adrenal mass has been advocated by some authors, although this treatment remains controversial [14–16]. Many patients have been demonstrated to benefit from surgical resection of AM and long-term survival can be achieved [14]. There is accumulating evidence that resection of isolated adrenal metastasis offers a survival benefit [17]. In a single-institution review of all adrenalectomies for isolated AM, Sarela et al [18] noted a median survival of 28 months. Oncologically, patients with a solitary adrenal metastasis are candidates for adrenal metastasectomy given the good rate of freedom from disease after surgery and the acceptable survival rates compared with those for patients who have multiple metastases [19].
The effect of TACE on AM theoretically should be good, because metastatic lesions are hypervascular. However, TACE is hardly performed, as catheterization of the adrenal arteries and complete embolization of the adrenal gland are anatomically difficult because the adrenal glands are supplied by three different arteries, usually with the origin at different levels.
Percutaneous ethanol injection and acetic acid injection may be useful for small lesions, but they are not sufficiently effective for larger tumors.
RFA is being increasingly used for cure or palliation of cancer. Ablations have been performed on tumors in many different organs and tissues in the body, including liver, kidney, lung, musculoskeletal system, and adrenal glands. However, imaging-guided percutaneous RFA of adrenal tumors is still a relatively new procedure [20, 21] compared with the more widespread application of RFA for the treatment of hepatic [22–24] and renal [25–28] tumors.
The purpose of our study was to evaluate the feasibility, safety, imaging appearance, and short-term efficacy of imaging-guided percutaneous RFA of AM.
Materials and Methods
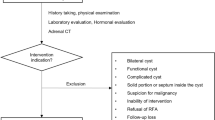
Six patients (two men and four women; mean age, 67.2 years; 55–74 years) with six AM were referred to our institution from 2003 to 2006 for imaging-guided percutaneous RFA (Table 1). Inclusion criteria were (1) the patients were not surgical candidates, (2) the imaging-guided procedure was feasible, (3) the lesion was <5 cm in diameter, and (4) there were no extra-adrenal metastases. The average diameter of the treated adrenal metastasis was 29 mm (range, 15–40 mm). In all patients, confirmation of the diagnosis was obtained with current CT protocols (wash-in and washout curves) in use at our institution [29, 30]. Before RFA an imaging-guided biopsy was performed and the frozen specimen sent to the Anatomy Pathology Laboratory to obtain confirmation of malignancy. In all patients, biopsy was performed through a 19-G coaxial needle just before the ablation session.
Referred patients were not surgical candidates; four patients had comorbidities (American Society of Anesthesiologists [ASA] class III or higher), and two patients refused to undergo surgery.
The procedures were performed in the interventional radiology room or in the CT scanning suite. Informed consent was obtained from all patients before the procedure. All patients had normal coagulation parameters and normal baseline pressure. Cefazolin, 2 g (Totacef; GlaxoSmithKline, Research Triangle Park, NC), was administered intravenously for antibiotic prophylaxis.
Treatments were performed using routine protocols for conscious sedation. Patients received intravenous midazolam, intravenous fentanyl, or subcutaneous bupivacaine or lidocaine at the site of the percutaneous needle insertion. CT guidance (Light Speed Plus R/GE Medical Systems, Milwaukee, WI; Aquilion 64; Toshiba, Tokyo) was performed for accurate localization of the tumor in RFA of four tumors, with the patient in the prone position. The other two lesions were treated under ultrasound guidance (Technos MPX; Esaote, Genoa, Italy) via transhepatic approach.
Heart rate, electrocardiographic tracing, oxygen saturation, and respiratory rate were continuously monitored, and blood pressure was determined every 2 min.
In one patient, RFA was performed soon after the embolization obtained in the same session. Selective embolization was performed via transfemoral approach, where a 5-Fr sheath (Terumo, Tokyo) was positioned and the renal artery was catheterized with a 5–Fr Cobra catheter (Cordis, Miami, FL); afterward superselective catheterization of the inferior adrenal artery was obtained with a 2.7-Fr microcatheter (Progreat, Terumo) and embolization was obtained injecting 300- to 500-μm PVA microparticles (Bead Block, Terumo).
All RFA treatments were performed using a coaxial LeVeen needle probe with an active diameter of 3 or 4 cm (Boston Scientific, Natick, MA) connected to a radiofrequency generator RF 3000 (Boston Scientific). Ablations were performed according to former protocols for LeVeen Needle Electrode sizes 3, 3.5, and 4 cm. RF power started at 40–80 W until an increase in tissue impedance (i.e., “rolloff”) was observed, signaling tumor coagulation. Rolloff in the first ablation phase was achieved after 8–19 min (media), reaching a maximum power of 90–180 W. These were followed after 30 s by a second ablation phase on the same lesion starting at approximately 70% of the power reached in the first phase, held constant again until automatic shutoff. Rolloff in the second ablation phase was achieved 5–15 min after reaching the maximum power. All treatments were performed by one of two radiologists, each with more than 5 years of experience in the performance of RFA.
Five patients were admitted for overnight observation and discharged home the following day. The patient who underwent both embolization and RFA was discharged after 3 days.
Technical success is defined as the correct position of needle in the lesion and the ability to fully expand the tines. Technical effectiveness is defined as complete ablation at first follow-up.
The follow-up was performed by CT at 1, 3, and 6 months and then yearly. Complete treatment was defined as no enhancement or enlargement of the treated adrenal gland, and this finding is consistent with local control; any focal enhancement in the ablated lesion should be considered indicative of residual or recurrent tumor.
Results
A technical success rate of 100% was obtained. No major complications occurred. In one patient shortly after initiation of ablation of the right adrenal mass, severe hypertension was noted (249/140 mm Hg) and treated with Brevibloc (esmolol; 100 mg total; 1.25 mg/kg). However, the RFA session was carried out with success. One patient developed post-RFA syndrome with pain and fever, treated with acetaminophen (500 mg/day for 3 days soon after the procedure). In five of six lesions, there was no residual enhancement in the treated tumor, indicative of complete tumor ablation. In one lesion a small area of residual enhancement of the tumor after the treatment was identified at the first CT control, and this finding indicated residual disease; the patient was re-treated after 10 days with another RFA session, with complete ablation of the lesion obtained (Fig. 1).
A 70-year-old woman with right adrenal gland metastasis. (A) Contrast-enhanced CT image obtained 1 month after RFA of the lesion, localized at the right adrenal gland, shows enhancement of the ablated lesion indicative of residual tumor (arrow). (B) Contrast-enhanced CT image obtained 1 month after the second treatment shows complete ablation of the right adrenal gland lesion (arrow)
At the 3- and 6-month follow-ups there was no evidence of residual enhancement or adrenal enlargement. These findings were confirmed by the subsequent controls (mean follow-up, 21 months; range, 6–36 months) (Fig. 2). In only one patient did we observe a shrinking of the treated lesion at 1-year follow-up.
A 74-year-old woman with left adrenal gland metastasis. (A) Contrast-enhanced CT image (basal, arterial and venous phases) shows the mass (arrow). (B) Transverse CT fluoroscopic image obtained with the patient in the prone position during RFA shows the correct deployment of needle tines into the adrenal mass. (C) CT images obtained 6 months after RFA: no enhancement of the lesion indicative of complete ablation (arrow) could be measured after injection of the contrast agent
Discussion
Metastatic tumor is the most common lesion in the adrenal gland at autopsy, and this is related to its rich sinusoidal blood supply. In previous reports, all documented adrenal ablation procedures involved a solitary unilateral adrenal tumor ablated in a single treatment session [11, 20, 21, 31, 32], for bilateral adrenal metastases ablated over the course of two or more sessions [21]. These case series documented the efficacy of ethanol [11, 31], acetic acid [12, 32], and RFA [20, 21] in local control of adrenal tumors <5 cm in diameter, at least in the short term (maximum follow-up in these studies was 46 months) [21].
Although we treated only metastases in the adrenal gland, our findings are similar to the results described by Mayo-Smith and Dupuy [21] and Wood et al. [20], who treated primary and metastatic adrenal cortical carcinomas. They found that RFA had minimal morbidity and was effective for local control of adrenal cortical lesions, particularly those <5 cm in diameter.
In our experience too, larger lesions may be associated with a higher incidence of residual tumor: this finding is due to the local effect of RFA in tumor control, since with the current electrodes, we can only treat a lesion with a diameter of ≤4 cm with each application. In fact in a patient with a 4-cm lesion we associated RFA and embolization with enlargement of the necrosis volume. Only the inferior adrenal artery was selectively catheterized and embolized because our intent was not to destroy the entire tumor with embolization but to increase the RFA effect of reducing heat dispersion by arterial flow.
We never treated bilateral metastases because all patients in our series had a unilateral solitary tumor, as the majority of adrenal lesions reported in the literature. Lo et al. [33] described a case of RFA for bilateral AM in which both masses were treated in a single session. The results were notable for the absence of endocrine and hemodynamic sequelae and for the marked improvement of the patient’s subjective symptoms of pain and discomfort. Rhim et al. [34] prevented adrenal insufficiency with adrenocorticoid and minerocorticoid replacement therapy.
Like Wood [20] and Mayo-Smith and Dupuy [21], we can confirm in our preliminary experience that RFA treatment of the adrenal gland can be performed on an outpatient basis with minimal morbidity: in fact we observed only a hypertensive crisis, treated with 70 mg of β-blockers without interruption of the procedure. In a previous report Chini et al. [35] suspended the procedure because they observed severe hypertension (249/140 mm Hg) associated with complex tachycardia (140 bpm) and frequent multifocal premature ventricular contractions. In a recent publication Onik et al. [36] reported hypertensive crises in two patients who underwent RFA of a liver metastasis adjacent to a normal right adrenal gland. Probably, the increasing catecholamine concentration during RFA is due to the absence of adrenal vein ligation during RFA while ligation of the adrenal vein after surgical exposure of the adrenal gland is achieved. Ligation of the adrenal vein will prevent the release of catecholamines into the systemic circulation [37].
Atwell et al. [38] have reported a case of hypertensive crisis during cryoablation of an adrenal metastasis, treated with intravenous sodium nitroprosside in 100- to 200-μg increments (for a total dose of 800 μg) and a 100-mg bolus of esmolol; based on their experience the authors suggest that it may be prudent to pretreat this patient population with α-adrenergic blocking medications (e.g., phenoxybenzamine, 10–20 mg orally twice daily for 10–14 days before ablation). The rationale for using α-adrenergic blocking medications is to mitigate or prevent catecholamine-mediated vasoconstriction during or after tumor manipulation. In accordance with Mayo-Smith and Dupuy [21], we recommend the use of multitines rather than a single electrode because greater areas of tumor necrosis can be achieved with a single application.
We found that CT is the preferred imaging modality for performing adrenal RFA; ultrasound guidance is feasible via transhepatic route in accordance with Mayo-Smith and Dupuy, and it is helpful, as in our case, when RFA is associated with embolization in the same session to enlarge the volume of necrosis. CT is also the preferred imaging modality to follow-up the RFA treatment. PET may now be the most commonly used surveillance tool in patients with cancer. Numerous studies report a high sensitivity and specificity of PET for identifying metastatic and recurrent cancer. PET/CT has emerged as a powerful tool for evaluation of adrenal masses and may have great potential for improving the sensitivity and accuracy of adrenal imaging [17]. We did not use PET scan for our patients because it is not available at our institution.
Conclusion
In conclusion, our preliminary results suggest that imaging-guided percutaneous RFA is effective for local control of AM, without major complications and with a low morbidity rate related to the procedure. Long-term follow-up on larger series will need to be performed and appropriate patient selection criteria will need to be determined in future randomized trials.
References
Abrams HL, Spiro R, Goldstein N (1950) Metastasis in carcinoma: analysis of 1000 autopsied cases. Cancer 3:74–85
Bullock WK, Hirst AE Jr (1953) Metastatic carcinoma of the adrenal. Am J Med Sci 226:521–524
Cedermark BJ, Blumenson LE, Pickren JW et al (1977) The significance of metastases to the adrenal glands in adenocarcinoma of the colon and rectum. Surg Gynecol Obstet 144:537–546
Momoi H, Shimahara Y, Terajima H et al (2002) Management of adrenal metastasis from hepatocellular carcinoma. Surg Today 32:1035–1041
Sakamoto Y, Kubota K, Mori M et al (1999) Surgical management for adrenal gland metastasis of hepatocellular carcinoma. Hepato-Gastroenterology 46:1036–1041
Taniai N, Egami K, Wada M et al (1999) Adrenal metastasis from hepatocellular carcinoma: report of 3 cases. Hepato-Gastroenterology 46:2523–2528
Hokotate H, Inoue H, Baba Y et al (2003) Aldosteronomas: experience with superselective adrenal arterial embolization in 33 cases. Radiology 227:401–406
Inoue H, Nakajo M, Miyazono N et al (1997) Transcatheter arterial ablation of aldosteronomas with high-concentration ethanol: preliminary and long-term results. AJR 168:1241–1245
Miyazono N, Ueno K, Nakajo M et al (1996) Transcatheter arterial and adrenal embolization with iohexol-ethanol solutions: animal experimental study and clinical application. Invest Radiol 31:755–760
Shibata T, Maetani Y, Ametani F et al (2000) Percutaneous ethanol injection for treatment of adrenal metastasis from hepatocellular carcinoma. AJR 174:333–335
Maki DD, Haskal ZJ, Matthies A et al (2000) Percutaneous ethanol ablation of an adrenal tumor. AJR 174:1031–1032
Liang HL, Pan HB, Lee YH et al (1999) Small functional adrenal cortical adenoma: treatment with CT-guided percutaneous acetic acid injection—report of three cases. Radiology 213:612–615
Takada K, Nakamura K, Usuki N et al (1989) Adrenal arterial embolization and radiotherapy of a case with metastatic adrenal tumor and its tumor thrombus in inferior vena cava from hepatocellular carcinoma. Rinsho Hoshasen 34(12):1529–1532
Paul CA, Virgo KS, Wade TP et al (2000) Adrenalectomy for isolated adrenal metastases from non-adrenal cancer. Int J Oncol 17:181–187
Lo CY, Van Heerden JA, Soreide JA et al (1996) Adrenalectomy for metastatic disease to the adrenal glands. Br J Surg 83:528–531
Kim SH, Brennan MF, Russo P et al (1998) The role of surgery in the treatment of clinically isolated adrenal metastasis. Cancer 82:389–394
Mitchell IC, Nwariaku FE (2007) Adrenal masses in the cancer patient: surveillance or excision. Oncologist 12:168–174
Sarela AI, Murphy I, Coit DG et al (2003) Metastasis to the adrenal gland: the emerging role of laparoscopic surgery. Ann Surg Oncol 10:1191–1196
Antonelli A, Cozzoli A, Simeone C et al (2006) Surgical treatment of adrenal metastasis from renal cell carcinoma: a single-centre experience of 45 patients. BJU Int 97:505–508
Wood BJ, Abraham J, Hvizda JL et al (2003) Radiofrequency ablation of adrenal tumors and adrenocortical carcinoma metastases. Cancer 97:554–560
Mayo-Smith WW, Dupuy DE (2004) Adrenal neoplasms: CT-guided radiofrequency ablation—preliminary results. Radiology 231:225–230
Lo HW, Tsai YJ, Chen PH et al (2003) Radiofrequency ablation for treatment of hepatocellular carcinoma with cirrhosis. Hepatogastroenterology 50:645–650
Curley SA (2003) Radiofrequency ablation of malignant liver tumors. Ann Surg Oncol 10:338–347
Lencioni R, Cioni D, Bartolozzi C (2001) Percutaneous radiofrequency thermal ablation of liver malignancies: techniques, indications, imaging findings, and clinical results. Abdom Imaging 26:345–360
Gervais DA, McGovern F, Arellano RS et al (2003) Renal cell carcinoma: clinical experience and technical success with radiofrequency ablation of 42 tumors. Radiology 226:417–424
Farrell MA, Charboneau WJ, DiMarco DS et al (2003) Imaging-guided radiofrequency ablation of solid renal tumors. AJR 180:1509–1513
Breen DJ, Rutherford EE, Stedman B et al (2007) Managment of renal tumors by image-guided radiofrequency ablation: experience in 105 tumors. CardioVasc Interv Radiol 30(5):936–942
Sabharwal R, Vladica P (2006) Renal tumors: technical success and early clinical experience with radiofrequency ablation of 18 tumors. CardioVasc Interv Radiol 29(2):202–209
Boland GW, Lee MJ, Gazelle GS et al (1998) Characterization of adrenal masses using unenhanced CT: an analysis of the CT literature. AJR 171(1):201–204
Fugazzola C, Carrafiello G, Laganà D et al (2003) Neoplasie del surrene. Diagnostica per Immagini. Radiologia. In: Olivetti L, Chiesa A (eds) Neoplasie del rene, surrene e retroperitoneo: dalla diagnosi alla terapia. Ed Poletto, Milano, pp 113–130
Rossi R, Savastano S, Tommaselli AP et al (1995) Percutaneous computed tomography-guided ethanol injection in aldosterone-producing adrenocortical adenoma. Eur J Endocrinol 132:302–305
Liang HL, Pan HB, Lee YH et al (1999) Small functional adrenal cortical adenoma: treatment with CT-guided percutaneous acetic acid injection—report of three cases. Radiology 213:612–615
Lo WK, van Sonnenberg E, Shankar S et al (2006) Percutaneous CT-guided radiofrequency ablation of symptomatic bilateral adrenal metastases in a single session. J Vasc Interv Radiol 17:175–179
Rhim H, Dodd GD III, Chintapalli KN et al (2004) Radiofrequency thermal ablation of abdominal tumors: lessons learned from complications. Radiographics 24:41–52
Chini EN, Brown MJ, Farrell MA et al (2004) Hypertensive crisis in a patient undergoing percutaneous radiofrequency ablation of an adrenal mass under general anestesia. Anesth Analg 99:1867–1869
Onik G, Onik C, Medary I et al (2003) Life-threatening hypertensive crises in two patients undergoing hepatic radiofrequency ablation. AJR 181:495–497
Gulla N, Patriti A, Fabbri B et al (2003) Surgical technique and haemodynamic changes in adrenalectomy for secreting neoplasia: personal experience and review of the literature. Minerva Chir 58:87–92
Atwell TD, Wass CT, Charboneau JW et al (2006) Malignant hypertension during cryoablation of an adrenal gland tumor. J Vasc Interv Radiol 17:573–575
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carrafiello, G., Laganà, D., Recaldini, C. et al. Imaging-Guided Percutaneous Radiofrequency Ablation of Adrenal Metastases: Preliminary Results at a Single Institution with a Single Device. Cardiovasc Intervent Radiol 31, 762–767 (2008). https://doi.org/10.1007/s00270-008-9337-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-008-9337-1