Abstract
We report a rare case of late transjugular intrahepatic portosystemic stent shunt (TIPSS) occlusion due to progressive stent protrusion into the periportal liver parenchyma, which was a result of delayed liver shrinkage 2 years after TIPSS. The initial TIPSS procedure had been carried out in a 52-year-old man as a bridge for liver transplantation because of post-alcoholic liver cirrhosis. We describe the applied TIPSS recanalization and revision technique. Immediately after TIPSS revision acute liver failure developed, which required emergency liver transplantation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The minimally invasive transjugular intrahepatic portosystemic stent shunt (TIPSS) is a well-accepted method in the management of liver cirrhosis-associated variceal bleeding, ascites, and Budd-Chiari syndrome [1, 2]. Despite its therapeutic success, TIPSS can be associated with clinical and technical complications including mechanical stent-specific problems such as stent fracture, protrusion, and migration [3]. Even after a technically successful TIPSS procedure, up to 33–50% patients still require percutaneous interventions for shunt malfunction [3–6].
A clinically relevant worsening of liver function after TIPSS procedure or revision has been reported infrequently [6–9]. In TIPSS revision, to the best of our knowledge, such an emergency has not previously been reported. If TIPSS-associated liver failure occurs, the morbidity and mortality of this complication are very high: 95% of these patients die or require liver transplantation within 90 days after TIPSS creation [10, 11].
Case Report
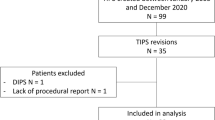
The 52-year-old man presented here had been listed for liver transplantation since January 2004 because of post-alcoholic liver cirrhosis Child B complicated by therapy-refractory ascites (Fig. 1) but without variceal bleeding episodes.
A, B. Before TIPSS placement in 2004, the preinterventional baseline CT scan (venous phase) showed typical signs of liver cirrhosis with ascites (arrowheads), relative atrophy of the right lobe, and a nodular liver contour. We found a technically simple anatomic situation with a prominent right portal vein. (A) MIP projection created from axial contrast-enhanced venous slices and (B) a three-dimensional volume-rendered reconstruction
A TIPSS procedure was performed in October 2004 using the standard technique [1, 8]. The initial portosystemic gradient measured 25 mmHg and decreased after implantation of a 10/60 mm Palmaz Genesis stent (Cordis Europe, The Netherlands) to 8 mmHg (Fig. 2). Postinterventional total heparinization for 48 hr was carried out. Liver-specific laboratory parameters remained normal after TIPSS (Table 1) and ascites decreased shortly after TIPSS creation.
In January 2005, the patient reported increasing abdominal width. Instead of scheduled routine invasive TIPSS controls in our institution, which he refused, ultrasonography was performed in a peripheral hospital over a period of 2 years, which was always considered normal.
In September 2006, the patient—still listed for liver transplantation and showing normal liver-specific laboratory tests (Table 1)—was referred to our institution for an emergency umbilical hernia operation. Because the periumbilical skin was so malperfused, complete excision of the navel had to be performed. During postoperative follow-up, ascites was detected and punctured daily. Ultrasound findings in our institution were interpreted as a stenosis of the TIPSS. Invasive portography was performed using a transjugular approach. Despite the easy introduction of a 7 Fr guiding catheter (Angiomed Bard, Germany) and a 5 Fr vertebralis catheter (Terumo Europe, Belgium) into the TIPSS outflow tract, it was not possible to catheterize the proximal TIPSS and reach the portal vein. Pushing the catheter tip against the proximal portion of the stent, portography was carried out (Fig. 3A).This revealed almost complete TIPSS tract occlusion without regular venous outflow. The proximal stent portion was protruding out of the lacerated portal vessel wall into the periportal liver parenchyma. However, contrast extravasation was not present around the stent (Fig. 3A).
(A) Portography showed protrusion of the proximal stent ending into the periportal liver parenchyma (arrowhead) without contrast extravasation around the portal vein (arrow). (B) The vertebralis catheter (arrow) positioned in the main trunk of the portal vein through a TIPSS mesh (arrowhead). (C) Dilatation of the TIPSS mesh (arrowhead) with a 10/40 mm balloon. (D) Creation of a TIPSS neo-tract with a 10/68 mm self-expanding Wallstent (arrowheads). (E, F) After postdilatation with a 12/40 mm balloon dilatation catheter there was a normal angiographic appearance of the TIPSS tract but still a portosystemic pressure gradient of 17 mmHg. (G) Extension of the TIPSS tract into the liver vein using a balloon-expanding stent (arrowheads). Portography demonstrated a regular TIPSS tract with a portosystemic pressure gradient of 9 mmHg
Because direct shunt revascularization was impossible, it was decided to perform a TIPSS obliteration by creating an end-to-side shunt through a stent mesh into the portal vein to maintain normal anatomy. The portal vein was reached through a stent mesh using a Terumo wire and a vertebralis catheter (Fig. 3B). Subsequently, the stent mesh was dilated with a 10/40 mm balloon dilatation catheter (Powerflex, Cordis Europe, The Netherlands; Fig. 3C). After pushing a 10 Fr sheath (Superflex, Arrow International, USA) through the widened stent mesh, a 10/68 mm self-expanding Wallstent-uni endoprosthesis (Boston Scientific, USA) was implanted (Fig. 3D). Despite postdilatation of the entire neo-tract with a 12/40 mm balloon catheter, the portosystemic pressure gradient was 17 mmHg (Fig. 3F). It was found that the TIPSS outflow (Fig. 3F) into the liver vein was another problem. The shunt tract was further extended into the liver vein by a balloon-expandable 10/40 mm Genesis Stent (Cordis Europe, The Netherlands) which was dilated up to 12 mm diameter. Control portography documented proper stent positions without stenosis or thrombosis. The final portosystemic pressure gradient measured 9 mmHg (Fig. 3G). The intervention was performed under analgo-sedation with 1.25 mg midazolam (Hoffmann–La Roche, Grenzach-Wyhlen, Germany) and 75 mg pethidine (Aventis Pharma, Bad Soden, Germany). For peri-interventional anticoagulation, a total of 8,000 IU heparin was given.
One day later, massive elevation of liver enzymes (GPT, >800 U/l; GOT, >1000 U/l) was recognized (Table 1) and the MELD (model for end-stage liver disease) score [12] rose from 7 to 14 points. A contrast-enhanced (150 ml Imeron 300, Altana Pharma, Germany) multiphase (native, arterial phase, portocaval phase, late phase) CT scan (Somatom 4, Siemens, Germany) was carried out. This detected no abnormalities in either the shunt tract (Fig. 4B) or the liver arteries. However, multiple small filling defects in the superior mesenteric vein were identified suggesting partial thrombosis, which was previously unknown (Fig. 4C). Pre-TIPSS and post-TIPSS liver volumes and cranio-caudal diameters were compared. For that purpose, the data of the baseline and post-TIPSS revision CT studies were analyzed by a three-dimensional liver volumetry program (Volume Viewer Plus, AW Suite 5.5.3b, General Electric, USA).
(A) CT after TIPSS revision showed that the TIPSS tract is perfused (black arrowhead); the liver is cirrhotic, and in the venous phase slightly inhomogeneous (white arrows). (B) The three-dimensional volume-rendered reconstruction showed a standard location and perfusion of the TIPSS tract (black arrowhead marks inflow, white arrowhead marks outflow). (C) Coronally orientated MIP projection demonstrated partial thrombosis of the superior mesenteric vein (white arrowheads) as a complication of the recent herniotomy
Because this situation was summarized as acute liver failure, emergency liver transplantation was performed 1 day later, without complications and using a modified piggy-back technique according to Belghiti [13]. Pathologic examination of the explanted liver showed complete cirrhotic conversion with distinct perisinusoidal fibrosis due to the known post-alcoholic liver cirrhosis without signs of necrotic liver parenchyma as a possible embolic complication of the partial thrombosis of the superior mesenteric vein. Furthermore, the partial thrombosis of the superior mesenteric vein was removed during the transplantation using a Fogarty maneuver.
After an uneventful postoperative follow-up with normalization of the liver function, the patient was transferred from the intensive care unit to a regular ward 10 days after transplantation. He died 4 months later due to a massive pulmonary embolism.
Discussion
Liver Failure after Portal Decompression
Even after the primary use of covered stent-grafts for TIPSS, occlusions (2–6%) and hemodynamically significant stenoses (4.5–11%) can occur [5, 14]. Therefore, up to 33–50% patients still require percutaneous shunt revision in the first year after TIPSS [3–6].
Although TIPSS revisions are routine procedures, intervention-associated acute liver failure is a rare complication [7–9]. Neither liver-specific laboratory parameters (Table 1) nor the portosystemic pressure gradient, both comparable after primary TIPSS and after TIPSS revision, served as predictive factors for the acute onset of liver failure in our patient. However, the three-dimensional volumetric analysis demonstrated liver shrinkage from 2,130 ml before TIPSS creation to 2,018 ml before TIPSS revision (–5.3%) and a decrease of around 5.1% in the craniocaudal diameter as a distinct sign of progression of liver cirrhosis. Diversion of portal flow away from the hepatic sinusoids [15] and insufficient compensation by the hepatic arteries, both due to cirrhotic progression [16], might lead to reduced sinusoidal perfusion with hepatic ischemia resulting in acute liver failure.
Harrod-Kim et al. retrospectively reviewed TIPSS procedures carried out for the treatment of refractory ascites. Sixteen of 99 patients died shortly after TIPSS creation (mean survival of 1.9 months). During follow-up, these patients showed a significant increase in their MELD scores and a significant decrease in their portosystemic pressure gradients after TIPSS creation in comparison with the survivors [17]. The authors concluded that an excessive reduction of the portosystemic pressure gradient due to TIPSS in patients with severe liver dysfunction is associated with increased mortality.
The newly diagnosed partial thrombosis of the superior mesenteric vein in our patient was attributed to the recent herniotomy following a perioperative thrombosis of the umbilical vein. Postinterventionally, the patient was anticoagulated with intravenous heparin and there were no clinical symptoms or signs of bowel edema. After liver transplantation, histopathologic examination showed no signs of necrotic liver parenchyma due to possible portal embolization.
Stent Protrusion
Because of the concerns of our transplantation surgeons, and in contrast to Maleux et al. [18], we do not use covered stent-grafts such as the Viatorr endoprosthesis in patients receiving TIPSS as a bridge for planned liver transplantation. Major reasons for stent protrusion out of the portal vein into liver parenchyma could be the combination of residual rigid strength of the implanted Genesis stent, its relatively short portion within the portal vein, and the progression of liver shrinkage since TIPSS creation.
Therapeutic Alternatives
Interventional techniques to reduce the blood flow through a TIPSS tract have been described in a number of patients suffering from TIPSS-induced hepatic encephalopathy and TIPSS-induced liver failure [19–22]. Wolf et al. performed therapeutic shunt occlusion in 7 cases of acute liver failure in the early post-TIPSS period [23]. In these cases the TIPSS tract was occluded using a 10 mm balloon catheter, which was kept inflated in the TIPSS until permanent shunt occlusion was obtained. Applying this technique, Wolf et al. were able to reverse the liver failure, with survival of 3 patients.
In the patient presented in this report, liver transplantation was regarded as the only reasonable therapeutic option because there were serious concerns about severe liver necrosis suggested by the rapid increase in both bilirubin (from 0.8 to 4.2 mg/dl) and liver transaminases (Table 1). Our appraisal is endorsed by the report by Rouillard et al. [10], who demonstrated, that severe hyperbilirubinemia occurring after TIPSS creation is associated with progressive hepatic deterioration as well as high mortality with the need for liver transplantation [10]. Ninety-five percent of the patients who developed severe hyperbilirubinemia within 1 month after TIPSS placement, died or required liver transplantation within 90 days.
In conclusion, acute liver failure following TIPSS revision is an extremely rare but potentially disastrous complication. Retrospectively, we were unable to identify any prognostic parameters predicting its onset. The diagnosis of acute liver failure after either a primary TIPSS procedure or a TIPSS revision must occur as soon as possible to allow proper emergency salvage treatment.
References
Richter GM, Noeldge G, Palmaz JC, Roessle M (1990) The transjugular intrahepatic portosystemic stent-shunt (TIPSS): Results of a pilot study. Cardiovasc Intervent Radiol 13:200–207
Richter GM, Noeldge G, Palmaz JC, Roessle M, Slegerstetter V, Franke M, Gerok W, Wenz W, Farthman E (1990) Transjugular intrahepatic portacaval stent shunt: Preliminary clinical results. Radiology 174:1027–1030
Tesdal IK, Jaschke W, Buhler M, Adamus R, Filser T, Holm E, Georgi M (1997) Transjugular intrahepatic portosystemic shunting (TIPS) with balloon-expandable and self-expanding stents: Technical and clinical aspects after 3½ years’ experience. Cardiovasc Intervent Radiol 20:29–37
Textor HJ, Brensing KA, Wilhelm K, Strunk H, Block W, Raab P, Hofer U, Muller-Miny H, Layer G, Schiedermeier P, Schuller H, Sauerbruch T, Schild HH (1998) TIPSS: Technical and clinical results after 4 years. Röntgenfortschritte 168:361–368
Charon JP, Alaeddin FH, Pimpalwar SA, Fay DM, Olliff SP, Jackson RW, Edwards RD, Robertson IR, Rose JD, Moss JG (2004) Results of a retrospective multicenter trial of the Viatorr expanded polytetrafluoroethylene-covered stent-graft for transjugular intrahepatic portosystemic shunt creation. J Vasc Interv Radiol 15:1219–1230
Tripathi D, Redhead D (2006) Transjugular intrahepatic portosystemic stent-shunt: Technical factors and new developments. Eur J Gastroenterol Hepatol 18:1127–1133
LaBerge JM, Ring EJ, Gordon RL, Lake JR, Doherty MM, Somberg KA, Roberts JP, Ascher NL (1993) Creation of transjugular intrahepatic portosystemic shunts with the Wallstent endoprosthesis: Results in 100 patients. Radiology 187:413–420
Noeldge G, Richter GM, Roessle M, Haag K, Katzen BT, Becker GJ, Palmaz JC (1992) Morphologic and clinical results of the transjugular intrahepatic portosystemic stent-shunt (TIPSS). Cardiovasc Intervent Radiol 15:342–348
Somberg KA, Lake JR, Tomlanovich SJ, LaBerge JM, Feldstein V, Bass NM (1995) Transjugular intrahepatic portosystemic shunts for refractory ascites: Assessment of clinical and hormonal response and renal function. Hepatology 21:709–716
Rouillard SS, Bass NM, Roberts JP, Doherty CA, Gee L, Bacchetti P, Somberg KA (1998) Severe hyperbilirubinemia after creation of transjugular intrahepatic portosystemic shunts: Natural history and predictors of outcome. Ann Intern Med 128:374–377
Barton RE RJ, Saxon RR, Lakin PC, Petersen BD, Keller FS (1995) TIPS: Short and long-term results: a survey of 1750 patients. Semin Interv Radiol 12:364–369
Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, D’Amico G, Dickson ER, Kim WR (2001) A model to predict survival in patients with end-stage liver disease. Hepatology 33:464–470
Belghiti J (1994) Preservation of portacaval flow in liver transplantation: A technical progress originating from hepatic surgery. Ann Chir 48:989–990
Maleux G, Nevens F, Wilmer A, Heye S, Verslype C, Thijs M, Wilms G (2004) Early and long-term clinical and radiological follow-up results of expanded-polytetrafluoroethylene-covered stent-grafts for transjugular intrahepatic portosystemic shunt procedures. Eur Radiol 14:1842–850
Rosemurgy AS, Zervos EE, Goode SE, Black TJ, Zwiebel BR (1997) Differential effects on portal and effective hepatic blood flow. A comparison between transjugular intrahepatic portosystemic shunt and small-diameter H-graft portacaval shunt. Ann Surg 225:601–607
Burchell AR, Moreno AH, Panke WF, Nealon TF Jr (1976) Hepatic artery flow improvement after portacaval shunt: A single hemodynamic clinical correlate. Ann Surg 184:289–302
Harrod-Kim P, Saad W, Waldman D (2006) Predictors of early mortality after transjugular intrahepatic portosystemic shunt creation for the treatment of refractory ascites. J Vasc Interv Radiol 17:1605–1610
Maleux G, Pirenne J, Vaninbroukx J, Aerts R, Nevens F (2004) Are TIPS stent-grafts a contraindication for future liver transplantation? Cardiovasc Intervent Radiol 27:140–142
Hauenstein KH, Haag K, Ochs A, Langer M, Rossle M (1995) The reducing stent: Treatment for transjugular intrahepatic portosystemic shunt-induced refractory hepatic encephalopathy and liver failure. Radiology 194:175–179
Kaufman L, Itkin M, Furth EE, Stewart C, Trerotola SO (2003) Detachable balloon-modified reducing stent to treat hepatic insufficiency after transjugular intrahepatic portosystemic shunt creation. J Vasc Interv Radiol 14:635–638
Madoff DC, Perez-Young IV, Wallace MJ, Skolkin MD, Toombs BD (2003) Management of TIPS-related refractory hepatic encephalopathy with reduced Wallgraft endoprostheses. J Vasc Interv Radiol 14:369–374
Quaretti P, Michieletti E, Rossi S (2001) Successful treatment of TIPS-induced hepatic failure with an hourglass stent-graft: A simple new technique for reducing shunt flow. J Vasc Interv Radiol 12:887–890
Wolf DC, Siddiqui S, Rayyan Y, Rozenblit G (2005) Emergent stent occlusion for TIPS-induced liver failure. Dig Dis Sci 50:2356–2358
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Radeleff, B., Sommer, CM., Schawo, S. et al. Acute Liver Failure After a Late TIPSS Revision. Cardiovasc Intervent Radiol 31, 209–214 (2008). https://doi.org/10.1007/s00270-007-9215-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-007-9215-2