Abstract
The purpose of the study was to determine simultaneously the temporal changes in luminal vessel area, blood flow, and wall shear stress (WSS) in both the anastomosed artery (AA) and vein (AV) of arteriovenous polytetrafluoroethylene (PTFE) grafts. PTFE grafts were placed from the iliac artery to the ipsilateral iliac vein in 12 castrated juvenile male pigs. Contrast-enhanced magnetic resonance angiograpgy with cine phase-contrast magnetic resonance imaging was performed. Luminal vessel area, blood flow, and WSS in the aorta, AA, AV, and inferior vena cava were determined at 3 days (D3), 7 days (D7), and 14 days (D14) after graft placement. Elastin von Gieson staining of the AV was performed. The average WSS of the AA was highest at D3 and then decreased by D7 and D14. In contrast, the average WSS and intima-to-media ratio of the AV increased from D3 to D7 and peaked by D14. Similarly, the average area of the AA was highest by D7 and began to approximate the control artery by D14. The average area of the AV had decreased to its lowest by D7. High blood flows through the AA causes a decrease in average WSS and increase in the average luminal vessel area, whereas at the AV, the average WSS and intima-to-media ratio both increase while the average luminal vessel area decreases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
In 1893, Thoma [1] observed that the arterial diameter increases in response to elevated blood flow, resulting in normalization of wall shear stress (WSS) [2, 3]. As expected, this type of enlargement occurs in arteries that supply hemodialysis grafts because high blood flows are sustained while grafts remain patent. However, outflow veins (through which blood exits and returns to the heart) instead of enlarging to the increased flows become stenotic at the venous anastomosis.
The clinical relevance of this problem is quite significant. More than 200,000 patients in the United States have end-stage renal disease requiring hemodialysis with expanded polytetrafluoroethylene (PTFE) grafts placed for dialysis access [4]. Most grafts fail because of a stenosis at the vein-to-graft anastomosis or in the proximal outflow vein, which is believed to cause graft thrombosis [5]. A recent prospective study found primary patency (time from graft placement to the first intervention) of PTFE hemodialysis grafts to be only 23% at 1 year and 4% at 2 years [6]. To maintain graft patency, an estimated 1.22 procedures on average are needed: 0.54 angioplasties, 0.51 thrombectomies, and 0.17 surgical revisions. Therefore, greater than 200,000 procedures using PTFE hemodialysis grafts are performed annually [6]. This problem is further compounded by the expected doubling of the hemodialysis population during the next decade. Despite the increased morbidity associated with PTFE grafts and their rising costs, little is known about the etiology of hemodialysis graft failure.
Factors contributing to formation of the venous stenosis are not well understood, but likely include such factors as changes in WSS [7–9], turbulent flow [10], compliance mismatch [7, 9, 11], eddy currents [12], or the separation of boundary layers [7]. Changes in blood flow will also affect changes in compliance of the blood vessel wall as well as release factors from endothelial cells that have been stimulated by various mechanical and chemical stimuli such as oxygenated arterial blood and deoxygenated venous blood resulting from mixing of arterial and venous blood at the venous anastomosis.
Little is known about the temporal relationship of changes in blood flow and mechanical changes in the anastomosed artery and vein following placement of PTFE grafts such as would be used for hemodialysis. The purpose of this study was to assess simultaneously the temporal changes in both the anastomosed artery (AA) and the anastomosed vein (AV) of hemodialysis grafts. This information is needed in order to understand how mechanical forces are related to anatomical changes in grafted blood vessels in order to develop novel therapeutic interventions aimed at improving hemodialysis graft patency. Luminal vessel area, WSS, and blood flow changes were determined using cine phase-contrast magnetic resonance imaging (MRI) and contrast-enhanced magnetic resonance angiography (MRA). In addition, the intima-to-media ratio was determined. Phase-contrast MRI with MRA is a noninvasive technique that qualifies anatomy, flow, and velocity measurements simultaneously and reproducibly in a very short period of time [13, 14].
Materials and Methods
Placement of Arteriovenous Grafts
Approval of the Institutional Animal Care and Use Committee was obtained before any procedures were conducted on laboratory animals. The animals were housed and handled in accordance with the guidelines of the National Institutes of Health [15]. Polytetrafluoroethylene grafts (PTFE; 4 mm wide × 2 cm long; IMPRA, Tempe, AZ) were placed to connect either the right or the left iliac artery to the ipsilateral iliac vein in 12 castrated juvenile male pigs weighing 30–40 kg (Fig. 1). Sham operations were performed on the contralateral iliac vessels in order to serve as controls. The night before the procedure, each pig was administered an oral dose of aspirin (325 mg), and this dose was continued daily until the animals were killed. Before every surgical procedure, food was withheld from the pigs for 12 h. Pigs were anesthetized intramuscularly with a combination of 5 mg/kg tiletamine hydrochloride (50 mg/mL) and zolazepam hydrochloride (50 mg/mL), 2 mg/kg xylazine (Bayer, Shawnee Mission, KS), and 0.06 mg/kg glycopyrrolate. An intravenous fluid line was placed in an ear vein for administration of 5 mg/kg zolazepam hydrochloride for induction. Pigs were intubated and placed on a positive-pressure ventilator delivering oxygen (3–5 mL/kg) and isoflurane (1–3%). The end-tidal CO2 volume, oxygen saturation, heart rate, electrocardiogram, and blood pressure were monitored throughout the graft procedure.
The grafts were placed using a retroperitoneal approach. The iliac artery and vein were accessed and dissected from the surrounding tissue. A bolus of heparin (100 U/kg) was given intravenously, and the activated clotting time was monitored hourly and maintained at 250–300 sec. The iliac vein was clamped, a venotomy (0.5–1 cm) was made, and an end-to-side PTFE graft-to-vein anastomosis was created using 8-0 expanded PTFE sutures. The artery was clamped, an arteriotomy (5–7 mm) was made, and an end-to-side PTFE graft-to-artery anastomosis was created using 8-0 expanded PTFE sutures. The fascia was closed with a running 2-0 polypropylene suture, and the skin was closed with a running 4-0 polyglactin subcuticular suture. The contralateral iliac vessels were isolated only, not clamped, and served as controls. Each pig was extubated and monitored postoperatively.
Cine Phase-Contrast MRI and Contrast-Enhanced MRA
Cine phase-contrast MRI and contrast-enhanced MRA was conducted 12 h before the animal was killed. The flow, velocity, and area measurements were obtained on the grafted iliac vessels and on the contralateral nongrafted iliac vessels at 20 different phases of the cardiac cycle. Using the cine phase-contrast MRI and contrast-enhanced MRA data, the following parameters were calculated: WSS, Reynolds number (R e ), luminal vessel area, and change in vessel area during the cardiac cycle. All MR examinations used a Signa CVi 1.5Tesla system (GE Medical Systems, Milwaukee, WI) with a torso-phased array coil positioned over the pelvis. After an initial three-plane localizing scan, a test bolus of gadopentetate dimeglumine (1–2 mL) was given (Magnevist; Berlex Laboratories, Wayne, NJ), followed by a 20 mL saline flush injected at 3 mL/sec. A single slice overlying the lower abdominal aorta was scanned repeatedly about once per second and the time delay was noted between the injection of the contrast medium and its arrival in the lower aorta. In animals with patent grafts, contrast medium was visualized in the inferior vena cava (IVC) at the same time or within 1 sec of visualization in the aorta.
Gadolinium-enhanced three-dimensional (3-D) MRA was performed in a coronal oblique plane that included the lower aorta and iliac arteries. The scan parameters were TR = 5 msec, TE = 1.7 msec, flip angle = 35°, 0.75 excitations, 0.75 phase field-of-views (FOVs), 62.5 kHz receiver bandwidth, elliptic-centric phase-encoding, 256 × 192 scan matrix, and 20 cm × 15 cm FOV, giving an in-plane resolution of 0.78 mm × 0.78 mm. Thirty to 40 sections (1.2–1.4 mm) were obtained with 50% overlapping reconstruction in the z direction. The scan time was 20–25 sec. Contrast medium (30 mL) was injected at 3 mL/sec, followed by a 20 mL saline flush at the same rate. An appropriate scan delay derived from the test bolus sequence was chosen to ensure that the acquisition of the central portion of k-space corresponded with peak arterial enhancement.
The two-dimensional cine phase-contrast MRI sequences were conducted immediately after the 3-D MRA. Acquisitions were positioned perpendicular to the appropriate vessels at locations selected from maximum-intensity projection images and reformatted images from the 3-D MRA (Fig. 1), as follows: (1) iliac artery 2 cm proximal to the arterial anastomosis of the PTFE hemodialysis graft (AA); (2) iliac vein 2 cm cephalad to the venous anastomosis (AV); (3) distal abdominal aorta and IVC at 2 cm proximal to the bifurcation; and (4) contralateral control iliac vein (CV) and contralateral iliac artery (CA) at the point of the grafted arterial iliac inflow. Scan variables were TR = 13.2 ms, TE = 4.9 ms, flip angle 30°, one excitation, receiver bandwidth 15.6 kHz, 256 × 224 matrix, and 14-cm FOV, for an in-plane resolution of 0.55 mm × 0.62 mm. Slice thickness was 5 mm. The velocity-encoding gradient was set to 100 cm/sec, unless aliasing was identified on initial acquisitions. Electrocardiogram triggering was provided by a peripheral pulse oximeter. Acquisition times generally were 20–30 sec. Imaging planes (slices) were placed perpendicular to the artery or vein, with positioning guided by MRA images. Using retrospective gating and view sharing, the images were reconstructed to 20 evenly spaced time points in the cardiac cycle. Segmented k-space acquisition produced eight views per segment. Quantitative flow information was obtained only in the direction perpendicular to the slice. All flow calculations were made on an Advantix Windows workstation (Cardiac and Flow Analysis Tools, AW Release 4.0; GE Medical Systems). This was performed by a dedicated radiologist who is fellowship trained in MRI (JFG). Because, visually, turbulence was observed at the AV, the flow measurements were repeated twice within 5 mm of each other at the venous anastomosis and the averaged values from these two measurements were used.
Validation of Flow Measurements Using a Phantom Model
The accuracy of contrast-enhanced MRA and cine phase-contrast MRI was determined using a flow phantom constructed with 2-, 4-, and 5-mm-diameter plastic tubing attached to a cardiac bypass pump to generate an arterial flow waveform as reported previously from this institution [16]. Briefly, flow was measured with a cine phase-contrast sequence using segmented k-space acquisition at true flow rates of 145 mL/min, 315 mL/min, or 540 mL/min with 14-, 20-, 26-, or 32-cm FOVs, respectiely. Three different observers conducted flow measurements using PC MRA.
The average iliac artery measured 6 mm, and the average iliac vein measured 10 mm. The 5 mm-diameter tubing with an FOV of 14 cm (nine pixels) had less than a 2% rate of error at flow rates of 315 mL/min or 540 mL/min. For an FOV of 20 cm (six pixels), less than a 1.5% rate of error occurred at 315 mL/min, and a 2–4% rate of error occurred at 540 mL/min. The accuracy of the graft with a 4 mm diameter was the same as that for the graft with a 5 mm diameter. For 2 mm-diameter tubing at a flow of 145 mL/min, the rate of error was 2–14% with a 14 cm FOV (four pixels) or 2–23% with a 20 cm FOV (three pixels).
Reynolds Number
At every point, where flow was laminar rather than turbulent, the R e was calculated as R e = (r<v>d)/m, where r is the vessel diameter, <v> is the average velocity of blood, d is the density of blood, and m is the viscosity. The viscosity and density of blood were estimated as 3.45 cP and 1.0 g/mL respectively. A R e of less than 1000 generally indicates the lack of turbulence. At every point measured within the venous stenosis, the R e was 5-20. Thus, laminar flow was assumed to exist for all WSS calculations.
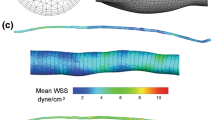
Calculation of WSS
The average WSS throughout the cardiac cycle was determined using Poiseuille’s law. For steady laminar flow in a tube, the WSS in dynes per square centimeters can be calculated directly from the average velocity (<v>) in centimeters per second with the formula WSS = 4<v>a/R, where a is the viscosity and R is the tube radius (in cm).
Postoperative Care
Analgesics included aspirin (325 mg orally) or buprenorphine (0.05 mg/kg intramuscularly) every 12 h on the basis of a pain determined by the animal’s activity and interest in food. Before graft placement, cefazolin (25 mg/kg intravenously) (GlaxoSmithKline, Philadelphia, PA) was given, and after graft placement, Cefardroxil (15 mg/kg orally) (Fort Dodge Laboratories) was given twice daily for 5 days as prophylaxis against infection.
Tissue Preparation and Morphometric Analysis
Grafts were explanted on day 3 (D3; n = 4), day 7 (D7; n = 3), and day 14 (D14; n = 5) after surgery. Pigs were medicated and anesthesia was started as described earlier. Both iliac vessels were dissected free of the surrounding soft tissue. A heparin bolus of 250 units/kg intravenous was given. The iliac artery supplying the graft was cannulated proximal to the graft and ligated beyond it. The recipient vein was dissected free beyond the anastomosis and ligated above and below. Drainage was allowed through an incision in this vessel, whereas the graft was perfused at physiologic pressure (100 mm Hg) with lactated Ringer’s solution until blood was cleared. This was performed simultaneously on the contralateral side, and these unmanipulated and unoperated iliac vessels were used as controls. The artery-to-graft-to-vein anastomosis, approximately 2 cm proximal and cephalad to the stenosis, was removed (Fig. 1). Tissues were divided into alternating 10-mm sections (AV and CV) along the specimen. The specimens were fixed in 10% formalin for 24 h, placed in 70% ethanol, and, finally, embedded in paraffin wax for morphometric analysis using Elastin von Gieson stain. These sections were then viewed with an Axioplan 2 Microscope (Zeiss, Oberkochen, Germany) equipped with a Neo-Fluor ×20/0.50 objective and digitized to 1030 × 1300 pixels using a Axiocam camera (Zeiss). Images covering one entire cross section from each section (V1 and CV1) of each vein-to-PTFE anastomosis were acquired and analyzed using KS 400 Image Analysis software (Zeiss). The thickness of the intima and media were manually traced from these slides (Fig. 2A and 2B). The intima was defined as the area above the internal elastic lamina that could be easily determined from the media because of the disorganized structure of the intimal cells. This was performed by only one operator (JH). The measurements were repeated a minimum of four times and the average measurement for each section per animal was used.
Statistical Analysis
Wall shear stress and R e were calculated for each animal from the data using phase-contrast MRI with MRA and averaged for the cardiac cycle including the values at the AV that were averaged for each animal at each time point. These values as well as the velocity, luminal vessel area, and flow obtained from the phase-contrast MRI with MRA were averaged for D3, D7, and D14 times for each vessel, including the intima-to-media ratio. Values were expressed as means ± standard deviations. Paired t-tests were used to compare vessels (grafted artery and control artery) overall and within each group (D3, D7, or D14). One-way analysis of variance (ANOVA) was used for comparisons among the four groups for a particular vessel. If a significant difference was found among the three groups pairwise, then two-sample t-tests were used to identify groups that were significantly different. A p-value of 0.05 or less was considered statistically significant. SAS version 8.0 (SAS Institute Inc., Cary, SC) was used for all statistical analyses.
Results
Graft Patency
Eight of the 12 grafts remained patent over the course of the study period. Analysis was conducted on the eight patent grafts. Thus statistical analysis included three grafts at D3, two grafts at D7, and three grafts at D14.
Luminal Vessel Area
As shown in Table 1, the average area of the AA in the D3 group was 36.79 mm2, in the D7 group it increased to 57.27, and it decreased in the D14 group to 42.07. This was a statistically significant change among the groups for the mean area. The average area of the aorta in the D3 group was 87.36, in the D7 group it was 99.87, and in the D14 group it was 96.16. This was statistically significant for the D3 and D7 groups. In the D3 group, the average area of the AV was 42.37, in the D7 group it was 42.49, and in the D14 group it was 38.3. In all three groups, the average area of the AV was statistically less than the average area of the control vein. The average area of the AA when normalized to the average of the control artery was 1.23 at D3, rose to 1.58 by D7, and decreased to 1.31 by D14. The normalized average area of the AV was 0.82 by D3, decreased to 0.63 by D7, and stayed at 0.65 by D14.
Blood Flow Measurements
As expected (Table 2), the average blood flow through the AV decreased from the D3 group to the D7 group and D14 group (p = NS). However, the average blood flow thorough the AA remained elevated at four to five times higher than the control artery for all three time points (p = NS).
Wall Shear Stress
In all three groups, the average WSS of the AA was statistically greater than the aorta and control artery. The average WSS of the aorta and control artery did not change significantly in the D3, D7, and D14 groups. The average WSS of the AA was statistically greater than the control artery at D3, decreased by 50% by D7 (p = NS) and by D14 (p = 0.05) as it approximated the average WSS of the control artery (Fig. 3a). In contrast, the average WSS of the AV was greater than that of the control vein at D3 but remained significantly greater than that of the control vein at D7 and D14 (Fig. 3b). In all three groups, the average WSS of the AV was statistically greater than the control vein and the IVC (p < 0.05). The average WSS of the AA when normalized to the control artery was 3.56 at D3, decreased by approximately 50% to 1.92 by D7, and was 2.47 by D14. The average WSS of the AV when normalized to the control vein was 2.09 in the D3 group and continued to increase by D7 (2.80) and D14 (4.20).
Intima-to-Media Ratio
As shown in Figure 4, the average intima-to-media ratio by D3 was 21.4. Although not statistically significant, by D14 the average intima-to-media ratio had increased to 25.2.
Discussion
This study is the first to report the simultaneous and sequential changes in WSS, blood flow, and luminal vessel area in AAs and AVs following placement of PTFE grafts using cine phase-contrast MRI with MRA. Following the placement of PTFE grafts, AAs and AVs respond to increased blood flow differently with respect to WSS, luminal vessel area change, and blood flow. As shown in previous studies, the mean luminal vessel area and the mean WSS increased in both the aorta and AA supplying the PTFE grafts [17, 18]. However, in the AV, the opposite occurred as the mean luminal vessel area decreased and the mean WSS and mean intima-to-media ratio increased over time.
One limitation of the current study is that mean WSS was calculated with the law of Poiseuille, which assumes that the vessels are circular. For most arteries, this is a reasonable assumption, but it does not hold true for veins, as they are elliptical. In addition, this law also assumes that there is steady laminar flow within a uniformly shaped tubular structure, which is not entirely true, particularly within venous stenosis, where local turbulent flow might occur. Visually, turbulent flow was observed at the AV during the phase-contrast MRI measurements. In order to increase accuracy, two measurements were made at the AV within 5 mm of each other and the average velocity and area measurements were used for the final calculation of WSS and Re.
A major implication of our findings is that the etiology of venous stenosis formation in hemodialysis grafts cannot be assumed to be similar to that of arterial remodeling. In the AV, high blood flow results in increased mean WSS and decreased mean luminal vessel area. The decrease in the mean area results from neointimal hyperplasia, which might result from platelet-mediated processes, inflammation, and release of migration factors from the endothelium. Interestingly, the mean IVC area decreased over time, whereas the mean blood flow remained unchanged, suggesting that the vascular remodeling response of the IVC to increased blood flow might be different that of the AV. The vascular remodeling process is a continuum beginning immediately after surgery, and future experiments will be conducted to evaluate the immediate WSS response after graft placement and prior to graft removal to better understand the venous vascular remodeling.
References
Thoma R (1893) Untersuchungen über die Histogenese and Histomechanik desGefässsystems. Vol. IV. Stuttgart: F. Enke
Kamiya A, Togawa T (1980) Adaptive regulation of wall shear stress to flow change in the canine carotid artery. Am J Physiol 239:H14–H21
Langille BL, Bendeck MP, Keeley FW (1989) Adaptations of carotid arteries of young and mature rabbits to reduced carotid blood flow. Am J Physiol 256:H931–H939
Shu MC, Hwang NH (1991) Haemodynamics of angioaccess venous anastomoses. J Biomed Eng 13103–112
Shu MC, Noon GP, Hwang NH (1987) Flow profiles and wall shear stress distribution at a hemodialysis venous anastomosis: Preliminary study. Biorheology 24:723–735
Fillinger MF, Reinitz ER, Schwartz RA, et al. (1989) Beneficial effects of banding on venous intimal–medial hyperplasia in arteriovenous loop grafts. Am J Surg 158:87–94
Hofstra L, Bergmans DC, Hoeks AP, et al. (1994) Mismatch in elastic properties around anastomoses of interposition grafts for hemodialysis access. J Am Soc Nephrol 5:1243–1250
Hofstra L, Bergmans DC, Leunissen KM, et al. (1995) Anastomotic intimal hyperplasia in prosthetic arteriovenous fistulas for hemodialysis is associated with initial high flow velocity and not with mismatch in elastic properties. J Am Soc Nephrol 6:1625–1633
Shu MC, Noon GP, Hwang NH (1987) Phasic flow patterns at a hemodialysis venous anastomosis. Biorheology 24:711–722
Pelc NJ, Herfkens RJ, Shimakawa A, et al. (1991) Phase contrast cine magnetic resonance imaging. Magn Reson Q 7:229–254
Pelc NJ, Sommer FG, Li KC, et al. (1994) Quantitative magnetic resonance flow imaging. Magn Reson Q 10:125–147
Loscalzo J (2000) Vascular matrix and vein graft failure. Circulation 101:221
Bendeck MP, Zempo N, Clowes AW, et al. (1994) Smooth muscle migration and matrix metalloproteinase expression after arterial injury in the rat. Circ Res 75:539–545
Zempo N, Kenagy RD, Au YPT, et al. (1994) Matrix metalloproteinases of vascular wall cells are increased in balloon-injured carotid artery. J Vasc Surg 20:209–217
Committee on Care and Use of Laboratory Animals of the Institute of Laboratory Animal Resources, National Research Council. Guide for the Care and Use of Laboratory Animals (rev). Washington, DC: Government Printing Office, 1996
King BF, Torres VE, Brummer ME, et al. (2003) Magnetic resonance measurements of renal blood flow as a marker of disease severity in autosomal-dominant polycystic kidney disease. Kidney Int 64(6):2214–21
Miller VM, Aarhus LL, Vanhoutte PM (1986) Modulation of endothelium-dependent responses by chronic alterations of blood flow. Am J Physiol 251:H520–H527
Zarins CK, Zatina MA, Giddens DP, et al. (1987) Shear stress regulation of artery lumen diameter in experimental atherogenesis. J Vasc Surg 5:413–420
Acknowledgments
This work was funded by the American Heart Association Beginning Grant in Aid (SM), the Cardiovascular and Interventional Radiology Research and Education Foundation (SM) and the Mayo Foundation (SM)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Misra, S., Woodrum, D.A., Homburger, J. et al. Assessment of Wall Shear Stress Changes in Arteries and Veins of Arteriovenous Polytetrafluoroethylene Grafts Using Magnetic Resonance Imaging. Cardiovasc Intervent Radiol 29, 624–629 (2006). https://doi.org/10.1007/s00270-005-0168-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-005-0168-z