Abstract
Purpose
To assess outcomes after microcoil embolization for active lower gastrointestinal (GI) bleeding.
Methods
We retrospectively studied all consecutive patients in whom microcoil embolization was attempted to treat acute lower GI bleeding over 88 months. Baseline, procedural, and outcome parameters were recorded following current Society of Interventional Radiology guidelines. Outcomes included technical success, clinical success (rebleeding within 30 days), delayed rebleeding (>30 days), and major and minor complication rates. Follow-up consisted of clinical, endoscopic, and pathologic data.
Results
Nineteen patients (13 men, 6 women; mean age ± 95% confidence interval = 70 ± 6 years) requiring blood transfusion (10 ± 3 units) had angiography-proven bleeding distal to the marginal artery. Main comorbidities were malignancy (42%), coagulopathy (28%), and renal failure (26%). Bleeding was located in the small bowel (n = 5), colon (n = 13) or rectum (n = 1). Technical success was obtained in 17 patients (89%); 2 patients could not be embolized due to vessel tortuosity and stenoses. Clinical follow-up length was 145 ± 75 days. Clinical success was complete in 13 (68%), partial in 3 (16%), and failed in 2 patients (11%). Delayed rebleeding (3 patients, 27%) was always due to a different lesion in another bowel segment (0 late rebleeding in embolized area). Two patients experienced colonic ischemia (11%) and underwent uneventful colectomy. Two minor complications were noted.
Conclusion
Microcoil embolization for active lower GI bleeding is safe and effective in most patients, with high technical and clinical success rates, no procedure-related mortality, and a low risk of bowel ischemia and late rebleeding.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Active lower gastrointestinal (GI) bleeding (i.e., hemorrhage originating below the ligament of Treitz) is often a dramatic condition that, fortunately, can be managed conservatively in most cases [1]. When medical and endoscopic management fails to equilibrate the patient’s hemodynamics and the number of units of packed red blood cells exceeds 5 [2] or 10 [3], invasive treatment is required. In such emergent settings, surgery with partial colectomy is associated with a perioperative mortality rate around 30% [4–6], typically ranging between 9% [7] and 47% among series, but sometimes up to 100% [8]. Therefore, transcatheter alternatives including intra-arterial vasopressin infusion and embolization have found their place in the therapeutic armamentarium.
In the late 1980s, technical progress occurred with transcatheter embolization, first with the use of microcatheters introduced coaxially through the main carrier catheter, allowing more distal catheterization [9, 10], and then with the arrival of microcoils suitable for embolization through these microcatheters [3, 11, 12]. Since then, microcoil embolization has gained increasing acceptance in the treatment of active lower GI bleeding. However, there remains a paucity of level I evidence to compare the results of (1) microcoils versus intra-arterial vasopressin infusion and, among publications using embolization via microcatheters, (2) microcoils versus other agents such as polyvinyl alcohol (PVA) and Gelfoam [13].
We report here the results of our experience with microcoil embolization for active lower GI hemorrhage and review it within the perspective of the existing literature [2, 3, 9–12, 14–41].
Materials and Methods
Study Group
We retrospectively studied all consecutive patients in our department in whom transcatheter arterial embolization was attempted using microcoils to control active lower GI hemorrhage over an 88 month period (January 1997 to May 2004). Our institutional review board approved the study.
Inclusion Criteria
We ran an initial query in our patient database which provided the details of all patients who underwent mesenteric arteriograms for lower GI bleeding during the study period. Then we kept only those patients in whom microcoil embolization was performed primarily (i.e., we excluded patients treated initially by vasopressin infusion, Gelfoam or other embolic agents). We included all patients in whom active bleeding was proven angiographically at the level of the lower GI tract (i.e., between the ligament of Treitz and the rectum). Transcatheter embolization was attempted with curative intent in all patients, with the purpose of treating the acute bleeding in a single procedure. Diagnostic arteriography was performed using digital subtraction imaging and selective contrast injections into the superior (SMA) and/or inferior (IMA) mesenteric arteries with the use of standard 5 Fr catheters. Additional superselective arteriograms were obtained as needed on a case-by-case basis.
Baseline characteristics included patient demographics, decrease in hematocrit that motivated the angiographic procedure, number of units of packed red blood cells transfused, and presence of five risk factors for embolization (multiorgan failure, malignancy, coagulation disorder, sepsis, and renal failure). We also recorded the segmental location of bleeding along the GI tract, the corresponding vascular territory (SMA versus IMA), and how distal the bleeding source was (either in the vasa recta or proximal to them). The likely cause of bleeding was determined on the basis of the clinical and imaging findings.
Treatment Technique
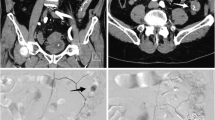
Once the bleeding site was identified, superselective catheterization was performed with the use of a 3 Fr microcatheter (Fast Tracker, Target Therapeutics, Fremont, CA; or Renegade HI-FLO, Boston Scientific, Natick, MA) inserted coaxially through the 5 Fr angiographic catheter. A steerable 0.018-inch wire was used coaxially through the microcatheter to direct its selective positioning in the small distal branch arteries of the mesenteric tree. Attempts were made to position the catheter just proximal to the bleeding site, allowing for superselective arteriography and embolization. The embolic agent was positioned either (1) at the level of the distal intestinal/colonic branches or the marginal artery of Drummond or its jejunoileal equivalent, or (2) beyond that level (i.e., microcoil deposition in the vasa recta or more distal mural branches) when possible. Embolization was performed using MRI-compatible 0.018-inch platinum Hilal embolization microcoils (Cook, Bloomington, IN) (i.e., no 0.035-inch coils were used) that were fluoroscopically guided into the bleeding vessel with a Coil Pusher (Target Therapeutics, Fremont, CA) via the coaxial microcatheter. A secondary embolic agent was used in addition to the microcoils in 2 cases, consisting of PVA particles (710–1000 μm in diameter) in patient 10 and Gelfoam slurry in patient 5 (i.e., pieces of a Gelfoam sheet fragmented mechanically in a three-way stopcock system).
Several additional procedural parameters were recorded including the type of anesthesia, use of intravenous conscious sedation, type and amount of radiographic contrast agent given, and fluoroscopy and total procedure time.
Patient Follow-up and Outcome Ascertainment
We defined outcome criteria following the guidelines of the Society of Interventional Radiology (SIR) [42].
Technical success was defined by immediate cessation of extravasation on repeat angiography at the end of the embolization procedure.
Clinical success was defined as the absence of recurrent bleed or hemodynamic instability within 30 days after embolization, as shown by close patient follow-up: patients were monitored immediately after the embolization procedure for symptoms and signs of intestinal ischemia or infarction (abdominal pain/tenderness, fever, nausea, peritoneal signs). Clinical success was subdivided into total success (i.e., resolution of signs or symptoms that prompted the embolization procedure), partial success (i.e., significant improvement of signs or symptoms after the embolization procedure and positive impact on the clinical course of the patient and/or the subsequent need for reintervention), or failure. Any lower GI rebleeding occurring later than 30 days after embolization was defined as delayed.
Complications were divided into minor and major events. Events during follow-up without long-term consequences and that required nominal or no therapy were defined as minor complications. Major complications were those that required therapy and minor hospitalization (<48 hr), or that required major therapy and an unplanned increase in the level of care, prolonged hospitalization (>48 hr), or that resulted in permanent adverse sequelae or death.
Data Acquisition and Analysis
Data were encoded simultaneously by two investigators (P.S., B.J.O.) and analyzed on standard spreadsheet software. Discrepancies in encoded data or data definition were resolved by consensus between the co-investigators. Data are presented as the average and 95% confidence intervals (CI). A p value < 0.05 was considered significant in all analyses. Fisher’s exact test was used for bivariate analyses. Subgroup analyses of outcomes during the follow-up period were based on the log rank test.
Results
Description of the Study Cohort and Baseline Parameters
The study cohort and its baseline characteristics are detailed in Tables 1 and 2. The source of bleeding was always located between the ligament of Treitz and the rectum. The area of contrast extravasation was located distal to the level of the marginal artery of Drummond or its equivalent. In cases of small bowel hemorrhage, the cause of bleeding remained undetermined in 4 of 5 patients (80%). Colorectal hemorrhages were related to diverticula in 7 of 14 patients (50%).
Procedure Description and Technical Success
Procedural parameters are described in Table 3. Nonionic contrast was given in all but one patient. Because embolization was performed in urgent settings, preliminary bowel preparation or antibiotic therapy was typically not given.
In all 19 patients, transcatheter embolization was the primary attempt at therapy and was the treatment of choice. Transcatheter embolization could be performed in 17 of 19 patients (89%), and immediate hemostasis was seen angiographically in all 17 patients after embolization. For colonic bleeding sources, embolization was performed at the level of the marginal artery or its equivalent in 75% of patients, while microcoils were positioned beyond that level in the remaining 25%. Embolization could not be achieved in 2 patients due to difficulties in performing superselective catheterization related to vessel tortuosity and stenosis (technical failures), and both eventually underwent partial colectomy.
Follow-up Period
Outcomes are here reported for all 19 patients together, even though 2 patients did not undergo embolization. Clinical follow-up information was available in all 19 patients for variable periods of time. The length of the clinical follow-up period, pooled over the study cohort and averaged per patient, and its 95% CI were 145 days ± 75 days (range 2–417 days). As none of our patients experienced a given event more than once during follow-up, the calculated person-time was 145 person-days. Each patient was examined clinically and followed until hospital discharge, which occurred 2–20 days after the embolization procedure. After discharge, 11 patients (58%) were followed clinically for the recurrence of lower GI bleeding and for signs and symptoms of intestinal ischemia/stricture. One of these patients died 35 days after embolization due to an unrelated cause.
Colonoscopic follow-up was available in 7 patients (37%). Five patients had colonoscopy performed following the embolization procedure, in order to evaluate the etiology of hemorrhage and search for post-embolization ischemic changes. In 3 of them, diverticular disease was found to be the source of bleeding and there was no evidence of ischemic changes. A fourth patient had normal follow-up colonoscopy. The fifth patient had ulcers at the hepatic flexure on colonoscopy 7 months after successful embolization. The exact cause of the ulcer was unclear, and ischemia could not be formally ruled out. The mean time between embolization and colonoscopy was 90 days (range 2–364 days).
Pathologic analysis of surgical specimens was available in 6 patients (32%). The 2 patients (11%) (patients 12 and 19) who had technically unsuccessful transcatheter embolization went to surgery within 48 hr of the angiographic procedure and their surgical resection specimens underwent pathologic examination. In addition, 4 patients (21%) (patients 1, 3, 15, and 18) underwent ileal or colic resection after technically successful embolization with pathologic examination of surgical specimens.
Outcomes During the Follow-up Period
Totalclinical success during the first month of follow-up (i.e., complete resolution of signs or symptoms that prompted the embolization procedure) was obtained in 13 of 19 patients (68%) (Table 4).
Five patients (26%) experienced clinical signs of early rebleeding. In 2 of them (patients 5 and 8), imaging studies (angiography at 12 hr post-embolization in one, bleeding nuclear scan at day 5 in the other) did not show any bleeding; conservative management was then continued successfully until hospital discharge; these 2 patients were thus considered as partial clinical successes (2/19, 11%). In the 3 other patients with early rebleeding (patients 2, 13, and 18), repeat arteriography showed rebleeding in the same, previously embolized site. One (patient 2) had recurrent jejunal hemorrhage a few hours after the initial procedure and underwent technically successful repeat embolization; however, further hemorrhage occurred 3 days later and was then treated by jejunal resection and primary anastomosis (thus considered as clinical failure of embolization), with uneventful follow-up after this surgery. Pathologic examination of the resection specimen revealed diffuse hemorrhagic mucosal erosions, microscopic foci of necrosis, and organizing thrombi in small submucosal vessels. Another patient (patient 13), who had a remote history of hemicolectomy and ileocolic anastomosis, experienced rebleeding on day 4 post-embolization. During repeat arteriography, bleeding was identified from a small branch of the middle colic artery; numerous attempts at selecting the target vessel were unsuccessful due to anatomic factors and resulted in spasm and thrombus in the middle colic artery. However, angiographic evidence of bleeding had disappeared at the end of this procedure. The patient remained stable for the next 7 days and was then discharged in good condition. This patient was considered as a partial clinical success of embolization. The third patient with local recurrence of hemorrhage at the embolized site (patient 18) rebled 3 days after embolization and underwent successful surgical resection of a proximal ileal loop and temporary ileostomy (clinical failure of embolization). Examination of the surgical specimen showed chronic serositis, satellite reactive lymph nodes, and two mucosal polypoid lesions (one mucosal surface erosion and one lymphangioma). The bleeding source could not be formally identified.
Thus, overall, 3 of 19 patients (16%) experienced partial clinical success within these 30 days (i.e., significant improvement of signs or symptoms after the embolization procedure in addition to positive impact on the clinical course of the patient and/or the subsequent need for reintervention), and 2 patients (11%) eventually underwent surgical bowel resection for continuing hemorrhage or early rebleeding (clinical failures). After adjusting for the variable lengths of follow-up periods in the patient cohort, these 5 patients (26%) corresponded to an early rebleeding rate of 1.27% per day, or 38% per month, for this first month after embolization, giving a rate of complete clinical success of 62% at 1 month. Overall, there was no statistically significant association (p ≥ 0.51) between early rebleeding and any of the five risk factors (multiorgan failure, malignancy, coagulopathy, sepsis, renal failure).
Delayed rebleeding occurred in 3 of the 11 patients (27%) in whom follow-up was longer than 30 days, but in all 3 was located in a different bowel segment from the initial embolization site. The late rebleeding rate in the embolized segment was, therefore, 0. In 2 of these patients (patients 1 and 10), these delayed hemorrhages subsided with conservative management. The third patient (patient 3) first experienced recurrent bleeding at 6 months of follow-up, which subsided with conservative management. She had another episode of late rebleeding at 10 months from another diverticular source. Because of the three successive bleedings in 1 year, known diffuse diverticulosis, prior transcatheter embolization, and occurrence of chest pain and hypotension during intra-arterial vasopressin infusion, this patient eventually underwent subtotal colectomy and ileostomy. Pathologic examination of the surgical specimen revealed no evidence of colon ischemia. The patient was stable thereafter with no further GI bleeding.
There were few complications. The only major complications consisted of early colonic ischemia experienced by 2 of the 19 patients (11%), typically within the first 48 hr following embolization. Both patients underwent immediate hemicolectomy and had satisfactory postoperative outcome. In 1 (5%) of these patients in whom elective colon surgery was already scheduled before the embolization (patient 1), sigmoid colectomy was performed electively 2 days after embolization, given the persistence of significant bleeding and fear of causing ischemia by repeat coiling. Transmural colonic infarction was found by pathologic examination of the resected surgical specimen. The second patient (patient 15) developed peritoneal signs on the first day after embolization and underwent right hemicolectomy (showing an ischemic colic segment at the hepatic flexure) with uneventful postoperative course. He had none of the five risk factors for bleeding described earlier, but had a prior history of coronary artery disease, hypertension and Billroth II surgery. He was the patient who was embolized with the largest number of microcoils (6) in the present cohort, and could be embolized at the level of the marginal artery only, not more distally. Overall, the occurrence of colonic ischemia in the patient cohort was not associated with the presence of sepsis (p = 0.221), malignancy (p = 0.322), coagulation disorder or renal failure (p = 0.510). It was not associated either with the level of embolization (at or beyond the marginal artery) (p = 0.436), the additional use of particles or Gelfoam (p = 0.614), or immediate technical success (p = 0.795).
There were two minor complications. In 1 patient (5%), migration of a microcoil into an anterior tibial artery occurred during the embolization procedure and did not result in any early symptom or long-term sequelae after 54 days of follow-up. In another patient (5%), transient elevation in serum creatinine was observed with subsequent normalization within days after the intervention.
Discussion
The present series supports the existing literature in demonstrating the safety and efficacy of microcoil embolization for curative treatment of active lower GI bleeding. Our observed technical success (89%) rate fell in the range observed in series based on microcatheters and coaxial technique (81–100%). Similarly, the present series was in line with the literature for several other dimensions of success: our rates of early rebleeding (26% without time adjustment, 38% with) and late rebleeding (0) and the incidence rate of bowel ischemia (12%) were within ranges published with the coaxial technique (0–40%, 0–33%, and 0–22%, respectively). However, the extent of these comparisons is limited to the ranges reported in the literature and we cannot compare our rates with summary estimates from existing reports, as explained below.
Table 5 places the present report within the perspective of the existing literature. Of 312 patients embolized for lower GI bleeding (i.e., 34 articles including the present one), 238 (78%) were treated by means of coaxial insertion of a microcatheter since the introduction of this technique in 1992. Of these 238 cases, 186 (76%) were embolized with microcoils, most other cases being treated by PVA and/or Gelfoam. The present series qualifies as the third largest in terms of the number of patients embolized by microcoils, after the series of Funaki et al. [37] and Kuo et al. [41]. Among smaller series of microcoil embolization, the largest ones (n = 6) reported sample sizes between 10 and 17 patients [27, 28, 33, 34, 38, 39]. In addition to the limited number of patients reported overall, our knowledge is further limited by the fact that no true meta-analytic summary is available that could establish summary thresholds for the rates of success, complications, and rebleeding. Some of the reasons include the small sample sizes of existing series and the variability in reporting standards, although improvement is notable over time, with larger series reported more recently and the creation of reporting guidelines [42]. However, sample sizes remain small and the misclassification of even a single patient (e.g., success versus failure) would produce a relatively large change in success or complication rates. In addition, small sample sizes result in wider confidence intervals around summary estimates. Also, only a few articles [27] have reported their results on an intention-to-treat basis. Furthermore, many articles have described the results of embolization in general without isolating the outcomes for microcoils only. Thus, comparisons between microcoils and other embolic agents would require going back to individual patient data for each of the selected reports. Probably the major obstacle to a meta-analysis of the field is that, in general, existing publications have described rates of success or complications that were not adjusted for the duration of patient follow-up. If, for any reason, the group of censored patients had the worst rebleeding rate, the unadjusted rates from the existing literature (i.e., not corrected for follow-up length) would overestimate the success of embolization. This is exemplified by our unadjusted rate of early rebleeding of 26% that rose to 38% after adjusting for the duration of early follow-up.
Thus, for all these reasons, weighted averages [13, 41] should not be considered as pooled summary estimates of a true meta-analysis and, therefore, cannot provide absolute thresholds for guidelines. Only the ranges observed in the individual studies may, in some cases, be useful [43]. Thus, the comparison proposed above of our results with those observed in prior articles should be understood in that context, and we have limited our comparisons here to reported ranges only, rather than weighted averages or thresholds.
Another issue that might benefit from further studies is the best location for deposition of embolic agents in lower GI bleeding. Before the use of coaxial systems, embolization for lower GI bleeding was associated with a rate of bowel ischemia ranging between 0 and 15% only, which is surprisingly not much different from that observed with newer coaxial technology and microcoils. However, as mentioned above, comparisons between the observed ranges at two different time periods are difficult, notably because of the concomitant evolution of reporting standards. Our patients experienced 12% major and 12% minor complications, but these numbers do not reflect the fact that intestinal ischemia may be of variable severity (mucosal ischemia versus transmural infarction) and its clinical relevance may depend on the particular circumstances. For example, some patients may already be scheduled to undergo elective surgery on the day following embolization. In such cases, the clinical significance of pathologic findings of ischemia is questionable and is typically not associated with unfavorable prognosis or postoperative complications. This has been shown by others [21] and is supported by our experience with one of our two patients with intestinal ischemia. In fact, embolization in some cases could be considered as a preoperative measure to limit intraoperative bleeding.
Few experimental data are available on the topic of the prevention of bowel ischemia during embolization. However, several important points have already been collected empirically, some of them dating from the time when only 0.035-inch coils were available. First, when using coils it is usually recommended that no more than one main branch (first- or second-order) of the SMA or IMA be embolized. Simultaneous proximal blockage of the right colic and ileocolic arteries, or of the middle colic artery and IMA, should always be avoided [23]. Second, even though embolization may be an effective therapy after failed vasopressin infusion, the opposite should probably be avoided: the infusion of vasoconstrictors after embolization decreases the collateral arterial supply to the bowel, which increases the risk of significant bowel ischemia [2, 18]. Third, empirical experience suggests that the site of coil placement should be distal [23]. Proximal embolization of a main branch of the SMA or IMA may not lead to bowel infarction in many cases, but it is also often insufficient to stop bleeding from a distal source. This point had already been noted at a time when only macrocoils (i.e., 0.035-inch caliber) were available [23]. Since the advent of microcoils (i.e., 0.018-inch caliber) and microcatheters (3 Fr or smaller) in the late 1980s to early 1990s, most series have been aiming at blocking the artery as close as possible to the bleeding point, usually in the vasa recta or distal arteries, or—by default—in the marginal artery or just proximal to it [27, 30, 32, 33, 35, 36, 40, 41, 44, 45]. When this was not technically possible, several described alternatives have included (1) deposition of the embolic agent in the marginal artery of Drummond or in the distal intestinal arcades [28, 29, 33, 41, 45], (2) flow-directed deposition of the embolic agent in cases where PVA was used [36], and (3) the avoidance of any embolization [27, 35].
The findings of the present study need to be understood within the context of the study design, which was retrospective in nature. Also, due to the small sample size, measures of association between predictors and outcomes were based on Fisher’s exact test, with the advantage of providing exact p values but the inconvenience of not providing a measure of the effect nor the confidence interval around it. Also, we did not adjust for follow-up length in our calculations of the incidence rate of acute bowel ischemia, because this complication typically occurs almost immediately (i.e., within 48 hr) after the embolization procedure. After these first 48 hr have elapsed, bowel ischemia would appear rather in its chronic presentation (i.e., months or years after the embolization procedure).
In conclusion, transcatheter arterial microcoil embolization is a safe and effective procedure to curatively treat active lower GI bleeding, with technical and clinical success observed in most patients and low procedure-related mortality. When delayed rebleeding occurred, it was related to another bleeding source in a separate location, for which embolization and/or other therapies can be attempted. Ischemic complications are observed in a minority of cases and do not always result in a worsened overall prognosis and clinical course. Future studies with larger sample sizes and based on current reporting guidelines will be helpful to refine summary estimates of rebleeding and complication rates.
References
Lefkovitz Z, Cappell MS, Lookstein R, et al (2002) Radiologic diagnosis and treatment of gastrointestinal hemorrhage and ischemia. Med Clin North Am 86:1357–1399
Palmaz JC, Walter JF, Cho KJ (1984) Therapeutic embolization of the small-bowel arteries. Radiology 152:377–382
Encarnacion CE, Kadir S, Beam CA, et al (1992) Gastrointestinal bleeding: Treatment with gastrointestinal arterial embolization. Radiology 183:505–508
Taylor FW, Epstein LI (1969) Treatment of massive diverticular hemorrhage. Arch Surg 98:505–508
Behringer GE, Albright NL (1973) Diverticular disease of the colon. A frequent cause of massive rectal bleeding. Am J Surg 125:419–423
Leitman IM, Paull DE, Shires GT, 3rd (1989) Evaluation and management of massive lower gastrointestinal hemorrhage. Ann Surg 209:175–180
Giffin JM, Butcher HR, Jr, Ackerman LV (1967) Surgical management of colonic diverticulitis. Arch Surg 94:619–626
Noer RJ (1955) Hemorrhage as a complication of diverticulitis. Ann Surg 141:674–685
Kusano S, Murata K, Ohuchi H, et al (1987) Low-dose particulate polyvinylalcohol embolization in massive small artery intestinal hemorrhage. Experimental and clinical results. Invest Radiol 22:388–392
Okazaki M, Higashihara H, Yamasaki S, et al (1990) Arterial embolization to control life-threatening hemorrhage from a Meckel’s diverticulum. AJR Am J Roentgenol 154:1257–1258
Guy GE, Shetty PC, Sharma RP, et al (1992) Acute lower gastrointestinal hemorrhage: Treatment by superselective embolization with polyvinyl alcohol particles. AJR Am J Roentgenol 159:521–526
Sharma VS, Valji K, Bookstein JJ (1992) Gastrointestinal hemorrhage in AIDS: Arteriographic diagnosis and transcatheter treatment. Radiology 185:447–451
Darcy M (2003) Treatment of lower gastrointestinal bleeding: Vasopressin infusion versus embolization. J Vasc Interv Radiol 14:535–543
Goldberger LE, Bookstein JJ (1977) Transcatheter embolization for treatment of diverticular hemorrhage. Radiology 122:613–617
Bookstein JJ, Naderi MJ, Walter JF (1978) Transcatheter embolization for lower gastrointestinal bleeding. Radiology 127:345–349
Chuang VP, Wallace S, Zornoza J, et al (1979) Transcatheter arterial occlusion in the management of rectosigmoidal bleeding. Radiology 133:605–609
Matolo NM, Link DP (1979) Selective embolization for control of gastrointestinal hemorrhage. Am J Surg 138:840–844
Jander HP, Russinovich NA (1980) Transcatheter gelfoam embolization in abdominal, retroperitoneal, and pelvic hemorrhage. Radiology 136:337–344
Walker WJ, Goldin AR, Shaff MI, et al (1980) Per catheter control of haemorrhage from the superior and inferior mesenteric arteries. Clin Radiol 31:71–80
Tadavarthy SM, Castaneda-Zuniga W, Zollikofer C, et al (1981) Angiodysplasia of the right colon treated by embolization with ivalon (polyvinyl alcohol). Cardiovasc Intervent Radiol 4:39–42
Rosenkrantz H, Bookstein JJ, Rosen RJ, et al (1982) Postembolic colonic infarction. Radiology 142:47–51
Chalmers AG, Robinson PJ, Chapman AH (1986) Embolisation in small bowel haemorrhage. Clin Radiol 37:379–381
Uflacker R (1987) Transcatheter embolization for treatment of acute lower gastrointestinal bleeding. Acta Radiol 28:425–430
Choo IW, Sproat IA, Cho KJ. (1994) Transcatheter embolization of the marginal artery of Drummond as treatment for life-threatening retroperitoneal hemorrhage complicating heparin therapy. Cardiovasc Intervent Radiol 17:161–163
Howlett DC, Farrugia MM, Irvine AT (1995) Case report: Therapeutic transcatheter embolotherapy in the control of recurrent haemorrhage from lymphoma of the small bowel. Br J Radiol 68:431–434
Curzon IL, Nicholson AA, Dyet JF, et al (1996) Transcatheter coil embolotherapy for major colonic hemorrhage (abstract). Cardiovasc Intervent Radiol 19 [Suppl 2]:S83
Gordon RL, Ahl KL, Kerlan RK, et al (1997) Selective arterial embolization for the control of lower gastrointestinal bleeding. Am J Surg 174:24–28
Nicholson AA, Ettles DF, Hartley JE, et al (1998) Transcatheter coil embolotherapy: A safe and effective option for major colonic haemorrhage. Gut 43:79–84
Peck DJ, McLoughlin RF, Hughson MN, et al (1998) Percutaneous embolotherapy of lower gastrointestinal hemorrhage. J Vasc Interv Radiol 9:747–751
Ledermann HP, Schoch E, Jost R, et al (1998) Superselective coil embolization in acute gastrointestinal hemorrhage: Personal experience in 10 patients and review of the literature. J Vasc Interv Radiol 9:753–760
Bulakbasi N, Kurtaran K, Ustunsoz B, et al (1999) Massive lower gastrointestinal hemorrhage from the surgical anastomosis in patients with multiorgan trauma: Treatment by subselective embolization with polyvinyl alcohol particles. Cardiovasc Intervent Radiol 22:461–467
Dobson CC, Nicholson AA (1999) Treatment of rectal hemorrhage by coil embolization. Cardiovasc Intervent Radiol 22:143–146
Evangelista PT, Hallisey MJ (2000) Transcatheter embolization for acute lower gastrointestinal hemorrhage. J Vasc Interv Radiol 11:601–606
Luchtefeld MA, Senagore AJ, Szomstein M, et al (2000) Evaluation of transarterial embolization for lower gastrointestinal bleeding. Dis Colon Rectum 43:532–534
Bandi R, Shetty PC, Sharma RP, et al (2001) Superselective arterial embolization for the treatment of lower gastrointestinal hemorrhage. J Vasc Interv Radiol 12:1399–1405
Defreyne L, Vanlangenhove P, De Vos M, et al (2001) Embolization as a first approach with endoscopically unmanageable acute nonvariceal gastrointestinal hemorrhage. Radiology 218:739–-748
Funaki B, Kostelic JK, Lorenz J, et al (2001) Superselective microcoil embolization of colonic hemorrhage. AJR Am J Roentgenol 177:829–863
Patel TH, Cordts PR, Abcarian P, et al (2001) Will transcatheter embolotherapy replace surgery in the treatment of gastrointestinal bleeding? Curr Surg 58:323–327
DeBarros J, Rosas L, Cohen J, et al (2002) The changing paradigm for the treatment of colonic hemorrhage: Superselective angiographic embolization. Dis Colon Rectum 45:802–808
Yoon W, Kim JK, Kim HK, et al (2002) Acute small bowel hemorrhage in three patients with end-stage renal disease: Diagnosis and management by angiographic intervention. Cardiovasc Intervent Radiol 25:133–136. Epub 2002 Feb 2019
Kuo WT, Lee DE, Saad WE, et al (2003) Superselective microcoil embolization for the treatment of lower gastrointestinal hemorrhage. J Vasc Interv Radiol 14:1503–1509
Drooz AT, Lewis CA, Allen TE, et al (2003) Quality improvement guidelines for percutaneous transcatheter embolization. J Vasc Interv Radiol 14:S237–242
Egger M, Smith GD, Altman DG (2001) Systematic reviews in health care: Meta-analysis in context, 2nd edn. London: BMJ
Ledermann HP, Schoch E, Jost R, Zollikofer CL (1999) Embolization of the vasa recta in acute lower gastrointestinal hemorrhage: A report of five cases. Cardiovasc Intervent Radiol 22:315–320
Funaki B (2002) Endovascular intervention for the treatment of acute arterial gastrointestinal hemorrhage. Gastroenterol Clin North Am 31:701–713
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/s00270-007-9183-6.
Rights and permissions
About this article
Cite this article
d’Othée, B.J., Surapaneni, P., Rabkin, D. et al. Microcoil Embolization for Acute Lower Gastrointestinal Bleeding. Cardiovasc Intervent Radiol 29, 49–58 (2006). https://doi.org/10.1007/s00270-004-0301-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-004-0301-4