Abstract
Purpose
To demonstrate the anatomic relationship of the internal jugular vein (IJV) with the common carotid artery (CCA) in order to avoid inadvertent puncture of the CCA during percutaneous central venous access or transjugular interventional procedures.
Methods
One hundred and eighty-eight consecutive patients requiring either central venous access or interventional procedures via the IJV were included in the analysis. The position of the IJV in relation to the CCA was demonstrated by portable ultrasonography. The IJV location was recorded in a clock-dial system using the carotid as the center of the dial and the angles were measured. Outcomes of the procedure were also recorded.
Results
The IJV was lateral to the CCA in 187 of 188 patients and medial to the CCA in one patient. The left IJV was at the 12 o’clock position in 12 patients (6%), the 11 o’clock position in 17 patients (9%), the 10 o’clock position in 142 patients (75%) and at the 9 o’clock position in 17 patients (9%). The right IJV was at the 12 o’clock position in 8 patients (4%), the 1 o’clock position in 31 patients (16%), the 2 o’clock position in 134 patients (71%) and the 3 o’clock position in 17 patients (9%). In one patient the left IJV was located approximately 60° medial to the left CCA; this was recorded as 2 o’clock on the left since it is opposite to the 10 o’clock position.
Conclusion
Knowledge of the IJV anatomy and relationship to the CCA is important information for the operator performing an IJV puncture, to potentially reduce the chance of laceration of the CCA and avoid placement of a large catheter within a critical artery, even when ultrasound guidance is used.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Percutaneous transjugular procedures are now routine in interventional radiology practice. The growth of central venous access procedure numbers, as well as transjugular liver biopsies and TIPS, has increased the need for the interventional radiologist to become familiar with the internal jugular vein (IJV) access. Anatomic landmarks have been used for IJV punctures for decades, such as the classic Sedillot triangle formed by the clavicle and both heads of the sternocleidomastoid, but in the last 10 or 15 years ultrasound-guided IJV puncture has been the standard of practice in the interventional radiology environment. Although the general anatomy, landmarks and relationship of the IJV with the common carotid artery (CCA) are known and have been described in anatomy texts [1], there are variations in position and relationship with the artery that may lead to inadvertent carotid artery punctures which may be disastrous [2]. The aim of the study was to demonstrate and report the anatomic relationship of the IJV with the CCA in order to help reduce the chances of inadvertent puncture of the CCA during central venous access or transjugular interventional procedures.
Materials and Methods
One hundred and eighty-eight consecutive patients requiring either central venous access (40%) or interventional procedures (60%) such as transjugular liver biopsies via the IJV were included in the study. There were 120 female and 68 male patients, ranging in age from 5 to 93 years (mean 52 years). Portable ultrasonography (SiteRite 2 and 3, 7.5 MHz transducer; Dymax, Pittsburgh, PA, USA) was used to collect information on the bilateral IJV anatomic position in relation to the CCA in a prospective study. Institutional Review Board review was not performed. Transverse scans at the thyroid isthmus level at the Sedillot triangle, about 2 cm from the clavicle, were performed holding the probe perpendicular to the skin and to the tracheal axis, without significant compression, to maintain the normal shape and location of the vessel. Some degree of extension of the head was used to record IJV location, with the head tilted approximately 30° to the opposite side in order to simulate real puncture. Location of the IJV was recorded using a clock-dial system with the CCA as the center of the dial. During examination of the neck vessels all patients were lying on the angiographic table with the operator standing by the patient’s head, looking at the patient from head to toe, as when performing an IJV puncture. Therefore the right side of the patient coincided with the right side of the operator and the clock-dial location of the IJV translates to the same disposition of the right IJV at the same side of the operator’s right hand. All procedures were performed by an interventional radiology fellow under supervision of an attending physician.
Regardless of the puncture site, right and left IJV positions were registered as in a clock-dial disposition. The center of the clock dial was the center of the CCA, and an imaginary line was drawn to the direction of the center of the IJV. For instance, if the IJV was just above (0°) the common carotid artery, this position was registered as 12 o’clock either right or left. If the IJV was true lateral (90°) to the CCA, it was registered as 9 o’clock on the left and 3 o’clock on the right. If the right IJV was at 30° lateral to the CCA, this was recorded as 1 o’clock position on the right and 11 o’clock on the left. If the right IJV was at 60° lateral to the CCA, this position was recorded as 2 o’clock on the right and 10 o’clock on the left. Periprocedural and postprocedural complications were recorded, as well as catheterization success rate and outcomes. Statistical analysis was performed using the chi-square test for comparison of proportions.
Results
Among the 188 consecutive patients, the IJV position was lateral to the common carotid artery, as expected, in 187 patients. The IJV location was medial to the left common carotid artery in one patient. Anatomic information of the IJV was as follows: The right IJV was at the 12 o’clock position in 8 patients (4%), the 1 o’clock position in 31 patients (16%), the 2 o’clock position in 134 patients (71%), and the 3 o’clock position in 17 patients (9%). The left IJV was at the 12 o’clock position in 12 patients (6%), the 11 o’clock position in 17 patients (9%), the 10 o’clock position in 142 patients (75%), and the 9 o’clock position in 17 patients (9%). In one patient the left IJV was located approximately 60° medial to the left CCA; this was recorded as 2 o’clock on the left since it is opposite to the 10 o’clock position (Fig. 1).
Schematic drawing of the anatomical relationship of the internal jugular veins and the common carotid artery, viewed with the patient in head-to-toe position, with the operator positioned at the head of the patient and ready to get internal jugular access. The distribution of the location of the vein in relation to the artery is given in a clock dial configuration and in percentages as seen in 188 patients, candidates for an internal jugular procedure.
Cannulation of the IJV was successfully achieved in the 184 patients with a patent IJV, 75% on the right and 25% on the left. Single stick vein puncture was achieved in 141 patients (77%), while multiple attempts were needed in 43 patients (23%). Bilateral IJV were thrombosed in 4 of the 188 patients, and alternative approaches were used. Recorded periprocedural and postprocedural complications included 2 inadvertent CCA punctures, which were immediately recognized due to the bright red color of the blood, as well as pulsatile flow. The IJV in these cases was positioned at 1 o’clock and at 2 o’clock respectively. The needle was immediately pulled out and appropriate pressure was held until hemostasis was achieved. Successful venous access followed the inadvertent arterial puncture. No neurologic or vascular sequelae were encountered in the follow-up of these 2 patients. One of the patients with a tunneled IJV hemopheresis catheter presented with numbness of the supraclavicular region near the catheter tunnel. This patient had a history of multiple sclerosis and also had numbness of the left foot. It was unclear whether loss of sensation was procedure-related or due to multiple sclerosis. One patient experienced swelling around the IJV site following placement of a tunneled dialysis catheter on the seventh day after the procedure. The patient was admitted to hospital and eventually required surgical evacuation of the hematoma when no arterial injury was identified.
Chi-square test for comparison of proportions with four degrees of freedom showed nonsignificant differences (p = 0.171) for all the comparisons.
Discussion
The IJV approach for central venous access is widely used by ICU physicians, surgeons and interventional radiologists. In the interventional radiology field, the transjugular approach is also used for TIPS, transjugular liver and kidney biopsy, and placement of inferior vena cava filters. Laceration of neck vessels, inadvertent arterial puncture, hematoma, catheter malposition, fragment embolization, air embolism, venous thrombosis and infection are the most common central venous access complications. The subclavian vein approach is now less popular due to increased risk of pneumothorax and difficulties in the technique, and the current trend is to use ultrasound guidance, even among nonradiologist practitioners [3, 4]. Normally, the IJV exits the skull base at the jugular foramen posterior to the internal carotid artery. The IJV follows the vascular bundle, down the neck, and most commonly becomes anterior and lateral to the CCA [3]. Even after surgery such as carotid endarterectomy, the IJV maintains its course and location [5, 6].
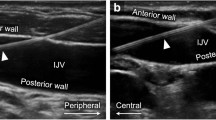
The IJV size may change with changes in intra-abdominal and thoracic pressures such as the Valsalva maneuver, Trendelenburg position, inspiration and expiration [7]. Ultrasound transducer positioning and pressure may modify the relative position of the IJV but may also allow selection of the best and safest puncture angle by redirection of the needle tip orientation [4, 8] (Fig. 2).
Ultrasound transducer positioning and pressure may modify the relative position of the IJV but may also allow selection of the best and safest puncture angle by redirection of the needle tip orientation. Note the lateral angulation of the needle, as the left internal jugular vein presents more anteriorly (at 12 o’clock) in relation to the common carotid artery.
Knowledge of the anatomy of the IJV and its variations may improve the success and safety of punctures, though it is currently accepted that ultrasonography helps in the puncture of the IJV and is likely to reduce the risks of arterial punctures [3, 9, 10]. However, there are several additional techniques that can be used for location or to facilitate the access of the IJV, such as rotation of the head, extension of the neck, breath-holding, and identification of anatomic landmarks. No maneuver is truly superior to others [11]. Experienced operators can use some or multiple maneuvers during the procedure to achieve success, especially in association with ultrasound guidance.
Since most of the interventional procedures performed via the transjugular route use the head tilted to the opposite side of puncture, as well as some degree of extension, we recorded the IJV location with the head tilted approximately 30° to the opposite side in order to simulate real puncture. Experience is important to reduce periprocedural complications, but there is always a learning curve, especially in teaching institutions. Despite the use of ultrasound, two inadvertent CCA punctures were performed by an interventional radiology fellow at the beginning of training.
Although ultrasound may decrease the rate of inadvertent CCA puncture to zero, as demonstrated in the literature [10], location of the IJV just above the CCA (12 o’clock), even slightly lateral to CCA, increases the risk of inadvertent arterial puncture. Ultrasound guidance maneuvers such as head tilting, use of a smaller size needle, ultrasound transducer manipulation, and single-wall puncture techniques may decrease the risk of undesired arterial puncture. One of the complications of inadvertent carotid artery puncture is thromboembolism in the cerebral circulation. A simple venous access procedure may actually cause debilitating or fatal stroke [11]. Inadvertent arterial puncture is not limited to CCA puncture. Inadvertent vertebral artery puncture during IJV cannulation and fatal brainstem stroke has also been reported in the literature [12]. During jugular vein cannulation tracheal tube cuff puncture was also reported [13]. In order to avoid inadvertent vertebral artery, carotid artery or surrounding organ puncture the single-wall technique is useful. The conservative single-wall technique also reduces the risk of hematoma in patients with coagulopathy, especially those with end-stage liver disease, requiring transvenous liver biopsy.
Jugular vein cannulation using the traditional blind technique, guided by external landmarks, can be extremely hazardous in patients with distorted anatomy of the neck and in coagulopathic individuals. We had one experience of growing hematoma at the same side of the puncture, in a case unrelated to this series, despite normal arterial imaging. Some of these incidents may be related to punctures of an adjacent vascular organ such as the thyroid with a goiter [14].
Since the size of the IJV varies from patient to patient during inspiration or expiration [7], we did not measure the diameter of the IJV. Our IJV cannulation was usually in a relatively high position, at the level of the cricoid cartilage, rather than the much lower puncture using the reference of the Sedillot triangle, to minimize the risk of pneumothorax or hemothorax. No pneumothorax or hemothorax complications were encountered in this series.
Use of the SiteRite ultrasound machine during interventional procedures has been very successful, as it is small and very portable, with no need for an external power source, and provides fairly good resolution for IJV puncture.
IJV cannulation using the traditional blind technique, guided by external landmarks, can be extremely hazardous in patients with distorted anatomy of the neck [14]. Awareness of the expected location of the IJV and anatomic variation is also important [15]. The left IJV was in the conventional position, or at 10 o’clock (30°), in 75% of the cases, and on the right the IJV was in the conventional position, or at 2 o’clock (30°) in 71% of the cases.
Ultrasonographic guidance gives additional valuable information to the operator when performing IJV puncture. Ultrasound technique is important to locate the IJV and for guidance of single-wall puncture of the IJV; however, occasionally ultrasound is unavailable, such as in emergency settings and for bedside venous access needs. These situations have kept the traditional blind technique in use, despite the advances in imaging. We believe that knowledge of the anatomic location and variations of position of the IJV are important to help physicians in those situations when imaging is not available. We have reported our clinical and anatomic data in order call the attention of practitioners to the potential problems of what are now fairly common procedures, and to inform them about the expected locations and anatomic variations of the IJV in the proximity of the CCA.
References
R Uflacker (1997) Veins of the head and neck R Uflacker (Eds) Atlas of vascular anatomy: An angiographic approach Williams and Wilkins Baltimore 81–112
D Dolla F Cavatorta S Galli et al. (2001) ArticleTitleAnatomical variations of the internal jugular vein non-uremic outpatients J Vasc Access 2 60–63
JG Caridi IF Hawkins SuffixJr BN Wiechmann et al. (1998) ArticleTitleSonographic guidance, when using the right internal jugular vein for central vein access AJR Am J Roentgenol 171 1259–1263 Occurrence Handle1:STN:280:DyaK1M%2Fhtlajsw%3D%3D Occurrence Handle9798857
SE Mitchell RA Clark (1979) ArticleTitleComplications of central venous catheterization AJR Am J Roentgenol 133 467–476 Occurrence Handle1:STN:280:CSaB38fntlM%3D Occurrence Handle111506
VP Khatri S Wagner-Sevy MH Espinosa et al. (2001) ArticleTitleThe internal jugular vein maintains its regional anatomy and patency after carotid endarterectomy: A prospective study Ann Surg 233 282–286 Occurrence Handle10.1097/00000658-200102000-00019 Occurrence Handle1:STN:280:DC%2BD3M7ls1Slsg%3D%3D Occurrence Handle11176136
JC Horrow S Metz D Thickman et al. (1987) ArticleTitlePrior carotid surgery does not affect the reliability of landmarks for location of the internal jugular vein Anesth Analg 66 452–456 Occurrence Handle1:STN:280:BiiB3M7htlI%3D Occurrence Handle3555165
PJ Armstrong R Sutherland DH Scott (1994) ArticleTitleThe effect of position and different manoeuvres on internal jugular vein diameter size Acta Anaesthesiol Scand 38 229–231 Occurrence Handle1:STN:280:ByuB1MrjslY%3D Occurrence Handle8023661
B Docktor CB So JC Saliken et al. (1996) ArticleTitleUltrasound monitoring in cannulation of the internal jugular vein: Anatomic and technical considerations Can Assoc Radiol J 47 195–201 Occurrence Handle1:STN:280:BymB3Mjls10%3D Occurrence Handle8640417
ML Skolnick (1994) ArticleTitleThe role of sonography in the placement and management of jugular and subclavian central venous catheters AJR Am J Roentgenol 163 291–295 Occurrence Handle1:STN:280:ByuA3M7htVE%3D Occurrence Handle8037017
Conz PA, Dissegna D, Rodighiero MP, et al.(1997) Cannulation of the internal jugular vein: Comparison of the classic Seldinger technique and an ultrasound guided method. J Nephrol 311–313
KJ Heath J Woulfe S Lownie et al. (1998) ArticleTitleA devastating complication of inadvertent carotid artery puncture Anesthesiology 89 1273–1275 Occurrence Handle10.1097/00000542-199811000-00035 Occurrence Handle1:STN:280:DyaK1M%2FjslyitQ%3D%3D Occurrence Handle9822023
MA Sloan JD Mueller LS Adelman et al. (1991) ArticleTitleFatal brainstem stroke following internal jugular vein catheterization Neurology 41 1092–1095 Occurrence Handle1:STN:280:By6B1Mnht1c%3D Occurrence Handle2067639
CD Blitt WA Wright (1974) ArticleTitleAn unusual complication of percutaneous internal jugular vein cannulation: Puncture of an endotracheal tube cuff Anesthesiology 40 306–307 Occurrence Handle1:STN:280:CSuC3cjhs1E%3D Occurrence Handle4814255
FS Silva (2003) ArticleTitleNeck haematoma and airway obstruction in a patient with goiter: Complication of internal jugular vein cannulation Acta Anaesthesiol Scand 47 626–629 Occurrence Handle10.1034/j.1399-6576.2003.00106.x Occurrence Handle1:STN:280:DC%2BD3s7otV2juw%3D%3D Occurrence Handle12699526
BS Lin CW Kong DC Tarng et al. (1998) ArticleTitleAnatomical variation of the internal jugular vein and its impact on temporary haemodialysis vascular access: An ultrasonographic survey in uraemic patients Nephrol Dial Transplant 13 134–138 Occurrence Handle10.1093/ndt/13.1.134 Occurrence Handle1:STN:280:DyaK1c7kt1Ohug%3D%3D Occurrence Handle9481729
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Turba, U.C., Uflacker, R., Hannegan, C. et al. Anatomic Relationship of the InternalJugular Vein and the Common Carotid Artery Applied to Percutaneous Transjugular Procedures. Cardiovasc Intervent Radiol 28, 303–306 (2005). https://doi.org/10.1007/s00270-004-0039-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-004-0039-z