Abstract
This study was done to compare antegrade punctures with a retrograde puncture technique for infrainguinal angioplasty. A group of 100 consecutive patients (71 men, 29 women) were randomized for antegrade puncture or retrograde puncture of the common femoral artery. Following retrograde puncture the guidewire was ‘turned’ and placed into the superficial femoral artery. The time for gaining access, screening time, radiation dose, patient height, weight and complications were recorded. All patients were reviewed the day after the procedure and within 3 months. Data from 46 patients (34 males and 12 females) in the retrograde group and 44 (28 males and 16 females) in the antegrade group were available for analysis. Mean procedure time, screening time, radiation dose, height and weight were 8.3 minutes (range 3–22), 2.1 minutes (0.3–6.5), 7950 mGy cm−2 (820–71250), 169 cm (149–204) and 79 kg (32–108) for retrograde puncture and 8 min (2–60), 0.7 min (0.0–3.2), 1069 mGy cm−2 (0–15400), 169 cm (152–186) and 75 kg (39–125) for antegrade punctures, respectively. An average of 1.2 (1–2) punctures was required for retrograde and 1.75 (1–8) for antegrade. Seven small hematomas occurred with antegrade and three for retrograde puncture. Retrograde puncture is technically easier with a tendency to fewer complications but results in a higher radiation dose. This technique should be used in difficult patients at high risk of haematoma formation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Interventional radiological procedures to revascularize the lower limbs are usually performed via a puncture in the common femoral artery. Techniques employed include antegrade puncture and contralateral retrograde puncture (up and over approach) [1]. At our institution we also use an ipsilateral retrograde puncture technique (turning the catheter in the ipsilateral iliac system or distal aorta) in difficult patients. The majority of these are very obese patients with a large ‘apron’ but also include patients who have had an ileostomy or colostomy.
These approaches present different technical challenges and may affect the success rate of the procedure, radiation exposure to the patient and complication rates. The publication of standards for interventional radiology [2 3] has focused attention on strategies to minimize complication rates. Apart from better training and more experienced operators to achieve the best results, any technique that makes intervention easier, including arterial puncture, would be advantageous. Some centers advocate the use of ultrasound to assist in arterial punctures but this is not widely available [4 5]. The purpose of this study was to compare the outcomes, including the safety, of antegrade and retrograde puncture for infrainguinal angioplasty access. The effect of these approaches upon procedure time and radiation dose was also assessed.
Materials and Methods
Patients
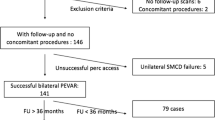
One hundred consecutive patients (69 men and 31 women; mean age 70) were enrolled from January 2000 to July 2001. One patient record was lost to the study, one patient with a high INR and six repeat studies were excluded. No patients were excluded from the study because of previous surgical procedures or previous groin punctures. All patients gave written informed consent. Patients were randomized to receive either antegrade (n = 44) or retrograde puncture (n = 46). Following successful access, a 6 French (F) vascular sheath (Bard, UK) was inserted and 4,000 units of unfractionated heparin sodium (CP Pharmaceuticals UK) were administered intraarterially. Antibiotics were not administered and no patient received a vascular closure device during the study period.
Technique
Antegrade.
Following skin preparation and draping, 10 ml 1% lidocaine (Braun, Germany) was injected into the skin and soft tissues. For antegrade puncture, a high puncture site was chosen to facilitate entry of the common femoral artery and passage of the guidewire down the superficial femoral artery. The Seldinger needle was introduced at a sufficiently steep angle to the skin surface, pointing caudally, so as to puncture the common femoral artery, avoiding puncture of the profunda femoris. This also facilitated the passage of the guidewire down the superficial femoral artery and allowed effective compression against the pelvis at the end of the procedure. A satisfactory puncture was confirmed by passage of the guidewire down the SFA or by contrast injection where necessary (Iohexol, Nycomed, Norway) and an 6F vascular sheath (Bard, UK) was inserted. Following inadvertent profunda puncture, the needle was withdrawn and manual compression was applied before further attempts at puncture.
Retrograde.
The retrograde to antegrade femoral cannulation technique has been previously described [6]. A summary of this is given below.
For retrograde puncture, a lower puncture site was chosen at a level 1–2 cm above the inguinal skin crease and the needle angled more vertically, at approximately 60° to the skin surface pointing cranially. As the angle of puncture required is more vertical than usual to facilitate turning of the catheter, a slightly higher puncture site is required compared to punctures for diagnostic angiography. A satisfactory puncture was confirmed by easy passage of the guidewire or by contrast injection. A standard 5 mm J guidewire (Cooks, UK) was then passed into the lower aorta and the needle was removed. Following this, a curved vascular catheter (sos Omni or Simmons 1 Cordis UK) was introduced until the tip extended beyond the guidewire and formed in the lower aorta. The guidewires was then exchanged for an angled terumo (0.035” Glidewire, Meditech, Watertown, MA, USA). The angled glidewire was then advanced back down the ipsilateral iliac system (Fig. 1a) and both wire and catheter were withdrawn into the common femoral artery and the guidewire then further advanced until a position in the SFA was achieved (Fig. 1b). The loop in the guidewire was then reduced by further withdrawal of the catheter until it was just traversing the arterial puncture site. Finally, the guidewire and catheter were advanced into the SFA until there was sufficient guidewire to allow placement of a 6F vascular sheath (Fig. 1c). Using a angled glidewire allowed negotiation of even the most difficult tortuous and calcified arteries.
At the end of the procedure, all patients underwent compression of the puncture site for a minimum of 10 min. The patients were then kept on strict bedrest for a period of 4 hr. Total time to gain access (i.e., time from injection of lidocaine to sheath placement), screening time for gaining access and the total radiation dose were recorded. Immediate and 30-day complications were also documented with clinical follow-up. As well as calculating a body mass index, a subjective assessment of body habitus was made at the time of the procedure, i.e., thin, average, obese and very obese.
Results
Antegrade Puncture
Data is absent for one patient and who has therefore been excluded from the results and analysis. Arterial access was achieved in 44 of 45 patients, requiring an average of 1.8 punctures and resulting in 7 hematomas at the puncture site (Table 1). There was complete failure to gain access in one patient. There was inadvertent puncture of the profunda femoris artery in 7 patients. None required additional treatment or prolonged hospital stay as a consequence.
The mean procedure time was 8.0 (range 2–60) min and the average screening time was 0.7 (range 0.0–3.2) min, giving an average radiation dose of 1120 mGy cm−2 (range 0–15400). Intravenous contrast was used as an adjunct to puncture in 8 patients (5–35 ml).
Retrograde Puncture
In this group there was complete technical and follow-up data. Successful access was achieved in 46 of the 47 patients, requiring an average of 1.22 punctures (range 1–2) with one complete failure. Retrograde puncture resulted in 3 complications, all hematomas, none of which required treatment or prolonged hospital admission (Table 2). The mean procedure time was 8.3 min (range 3–22) and the average screening time 2.1 min (range 0.3–6.5), resulting in an average radiation dose of 7950 mGy cm−2 (range 820–71250). Intravenous contrast (5–10 ml) was used as an adjunct to puncture in 7 patients.
Complications were not statistically proven to be greater in the antegrade group than in the retrograde (p = 0.25, chi-square). The frequency of contrast use was similar (p = 0.8, chi-square). Screening times (p < 0.0001, unpaired t-test) and radiation dose (p < 0.0002, unpaired t-test) were significantly higher in the retrograde group. The number of patients requiring more than 1 puncture was greater in the antegrade group (p < 0.1, chi-square) and significantly greater for those requiring more than 3 punctures (p < 0.02, chi-square). There was a very mild association between having an overweight/obese BMI (compared to normal BMI) and requiring more than 3 punctures (p = 0.22, chi-square); otherwise, neither BMI nor subjective assessment of habitus showed any association with clinical data. Comparative data between the two groups is shown in Table 3.
On fluoroscopy, mild or moderate femoral artery calcification was seen in the majority of our patients and appeared to occur in equal frequency in both groups (Table 4).
Discussion
In this study we have compared retrograde and antegrade arterial puncture for gaining femoral access in patients requiring infra-inguinal intervention. Because of the proposed difficulty encountered with antegrade punctures, particularly in obese patients, we wished to see if retrograde punctures offered any advantages.
Antegrade puncture is the standard means of obtaining access to the common femoral artery to carry out infra-inguinal intervention. Depending on the number of interventional cases within the unit, the numbers of antegrade punctures carried out by any individual operator can be very small. This access requires a much higher puncture than usual with a longer subcutaneous tract compromised by the abdominal apron, particularly in obese patients and therefore is technically more difficult.
If a sufficiently shallow angle of puncture of the common femoral artery is not obtained then the guidewire preferentially enters the profunda femoris artery requiring additional wire and catheter manipulation and prolonging the procedure. It is important to avoid supra-inguinal puncture of the iliac artery or direct puncture of the SFA which cannot be effectively compressed. Other pitfalls include inadvertent puncture of the profunda femoris artery or femoral vein requiring additional punctures; this is particularly important to avoid in patients for possible thrombolysis.
The technique of conversion from retrograde to antegrade puncture was originally described by Kadir et al. in 1980 [7] and was subsequently modified by Hartnell [6] in 1998. It is this modified technique we have used in this study. This is very simple technique even in tortuous or ulcerated iliac arteries and, as noted by Hartnell, is easy to teach to other staff, residents and fellows. Retrograde punctures are technically easier to perform and most operators have much greater experience with them as they are routinely used for obtaining access for diagnostic angiography. The puncture tracts, except in very obese patients, are usually short. In the absence of severe aorto-iliac disease, turning the catheter into the ipsilateral iliac system and then into the SFA is relatively straightforward and takes a short time to learn. The skin puncture site is lower than the abdominal apron and is therefore easier to palpate with less likelihood of supra-inguinal, direct SFA or inadvertent profunda femoris arterial puncture. Although screening is required in all patients, thus giving a higher average of radiation dose than in antegrade punctures, manipulation of the guidewire and catheter down the SFA is relatively straightforward.
The causes of complications associated with interventions are multifactorial. Identified risk factors include obesity, hypertension, anti-coagulation and uncorrected coagulopathies, large diameter catheters and vessel wall calcification [8 9 10 11 12 13 14 15 16]. Such factors should be identified before the procedure takes place and optimized as far as possible. Multiple punctures and ineffective compression further increase the complication risk. A recent report of the National Confidential Enquiry into Peri-operative deaths stating that “Cannulation of the femoral artery should always be below the inguinal ligament to avoid the danger of retro-peritoneal haematoma” [17] has stimulated discussion about the role of puncture site in hematoma formation [18 19]. As retrograde punctures are often easier to perform, particularly in obese patients, we felt that this approach may potentially reduce the complication rates associated with infra-inguinal intervention.
Although in this small study we have shown that there were fewer immediate complications with the retrograde group, probably because of the fewer punctures that were required, there were no major safety differences between the two techniques. The complications that resulted were minor, not requiring treatment or delay in discharge. Conclusions regarding any differences between the incidences of major complications cannot be drawn without a larger subject group.
There was no significant difference in the time to achieve arterial access between the two groups but the retrograde puncture required a substantially longer screening time and resulted in a higher radiation dose than antegrade puncture. This is due to the necessity of screening of the catheter and wire down from the aorta to the femoral artery in all patients in the retrograde group, through the thickest part of the patient, i.e., abdomen and pelvis. The radiation dose could be reduced by using pulsed fluorography, which was not available to us at the time of the study. We believe that these differences justify antegrade puncture as the technique of choice for the majority of patients. It was surprising that there was not a significant difference in the rate of complications in the overweight patients; a much larger sample size may reveal a difference. The fewer punctures and complications generated by the retrograde approach and its technical ease support its use, especially in those at high risk of hematoma formation.
References
B Kashdan D Trost M Jagust M Rackson T Sos (1992) ArticleTitleRetrograde approach for contralateral iliac and infra-inguinal percutaneous transluminal angioplasty: Experience in 100 patients. JVIR 3 515–521 Occurrence Handle1:STN:280:By2A1crps10%3D Occurrence Handle1387571
Society of Cardiovascular and Interventional Radiology (1997) Clinical Practice Guidelines. SCVIR, Virginia, USA
The Royal College of Radiologists (1999) Standards in vascular radiology BFCR (99)9. The Royal College of Radiologists, London
SL Kaufman (1980) ArticleTitleFemoral puncture using Doppler ultrasound guidance: Aid to transluminal angioplasty and other applications. AJR 134 402 Occurrence Handle1:STN:280:Bi%2BC3cnmtVY%3D
F Wacker KJ Wolf F Fobbe (1997) ArticleTitlePercutaneous vascular access guided by color duplex sonography. Eur Radiol 7 1501–1504 Occurrence Handle10.1007/s003300050324 Occurrence Handle1:STN:280:DyaK1c%2FjvFWhtg%3D%3D Occurrence Handle9369522
George. Hartnell (1998) ArticleTitleAn improved reversal technique from retrograde to antegrade femoral cannulation. Cardiovasc Intervent Radiol 21 512–513 Occurrence Handle10.1007/s002709900315 Occurrence Handle1:STN:280:DyaK1M%2FntVartw%3D%3D Occurrence Handle9853173
S Kadir A Baassir K Barth (1980) ArticleTitleTechnique for conversion of a retrogrqade into an antegrade femoral artery catheterisation. AJR 136 430–431
McDermott J, Crummy A (1994) Complications of Angioplasty. Seminars in Interventional Radiology, Vol. 11, No. 2, pp 145–149
S Duda J Wiskirchen M Erb et al. (1999) ArticleTitleSuture-mediated percutaneous closure of antegrade femoral arterial access sites in patients who have full anticoagulation therapy. Radiology 210 47–52 Occurrence Handle1:STN:280:DyaK1M7gt12ksw%3D%3D Occurrence Handle9885585
AH Cragg N Nakagawa TP Smith KS Berbaum (1991) ArticleTitleHematoma formation after diagnostic angiography: Effect of catheter size. JVIR 2 231–233 Occurrence Handle1:STN:280:By2C1M%2FotFQ%3D Occurrence Handle1799761
M Khoury S Batra R Berg K Rama V Kozul (1992) ArticleTitleInfluence of arterial access sites and interventional procedures on vascular complications after cardiac catheterizations. Am J Surg 164 205–209 Occurrence Handle1:STN:280:ByyD3snhvFw%3D Occurrence Handle1415915
F Kiemeneij J Hofland GJ Laarman DH van der Elst H. van der Lubbe (1995) ArticleTitleCost comparison between two modes of Palmaz Schatz coronary stent implantation: Transradial bare stent technique vs transfemoral sheath-protected stent technique. Cathet Cardiovasc Diagn 35 301–308 Occurrence Handle1:STN:280:BymC387ps1A%3D Occurrence Handle7497502
DW Muller KJ Shamir SG Ellis EJ Topol (1992) ArticleTitlePeripheral vascular complications after conventional and complex percutaneous coronary interventional procedures. Am J Cardiol 69 63–68 Occurrence Handle1:STN:280:By2C3cbitVM%3D Occurrence Handle1729869
FV Aguirre EJ Topol JJ Ferguson et al. (1995) ArticleTitleBleeding complications with the chimeric antibody to platelet glycoprotein IIb/IIIa integrin in patients undergoing percutaneous coronary intervention: EPIC investigators. Circulation 91 2882–2890 Occurrence Handle1:STN:280:ByqA3MnpsFA%3D Occurrence Handle7796496
HZ Friedman DR Cragg SM Glazier et al. (1994) ArticleTitleRandomized prospective evaluation of prolonged versus abbreviated intravenous heparin therapy after coronary angioplasty. J Am Coll Cardiol 24 1214–1219 Occurrence Handle1:STN:280:ByqD3Mrks1A%3D Occurrence Handle7930242
TF Kresowik MD Khoury BV Miller et al. (1991) ArticleTitleA prospective study of the incidence and natural history of femoral vascular complications after percutaneous transluminal coronary angioplasty. J Vasc Surg 13 328–333 Occurrence Handle1:STN:280:By6C3Mnmslc%3D Occurrence Handle1990173
Interventional Vascular Radiology and Interventional Neurovascular Radiology (November 2000). A report of the National Confidential Enquiry into Perioperative Deaths, London WC2A 3PN, UK
F Whimster M Raphael G Hartnell (2001) ArticleTitleFemoral artery catheterisation and retroperitoneal haematoma formation (Letter). Clin Radiol 56 933–934 Occurrence Handle10.1053/crad.2000.0823 Occurrence Handle11603898
J Jackson (2001) ArticleTitleFemoral artery catheterisation and retroperitoneal haematoma formation (Commentary). Clin Radiol 56 934–935 Occurrence Handle10.1053/crad.2001.0824
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nice, C., Timmons, G., Bartholemew, P. et al. Retrograde vs. Antegrade Puncture for Infra-Inguinal Angioplasty . CVIR 26, 370–374 (2003). https://doi.org/10.1007/s00270-003-2721-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-003-2721-y