Abstract
The purpose of this report is to discuss the different mechanisms of reperfusion of pulmonary arteriovenous malformations (PAVMs) after embolization. Transcatheter embolotherapy is currently the first-line treatment of PAVMs to prevent neurologic complications or pulmonary hemorrhage. Initial good results can be expected but we report three cases of reperfusion of complex large PAVMs after coil embolization. After adequate embolization, reperfusion of PAVMs may occur by several mechanisms including recanalization of embolized arteries, recruitment of normal arterial branches, growth or enlargment and development of a systemic arterial supply.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Percutaneous transcatheter embolotherapy is currently accepted as the treatment of choice to prevent neurologic complications or pulmonary hemorrhage in patients with pulmonary arteriovenous malformations (PAVMs) [1, 2, 3, 4, 5, 6, 7, 8, 9]. PAVMs are commonly associated with hereditary hemorrhagic telangiectasia (HHT), also known as Rendu-Osler-Weber disease [1, 2, 3, 10]. Regardless of the technique used, embolization using coils or detachable balloons is safe, well tolerated and associated with excellent symptomatic improvement [5, 11, 12, 13, 14]. Reperfusion of accurately embolized PAVMs is considered as a rare event, predominantly affecting large PAVMs [15]. Conversely, contrast-enhanced magnetic resonance (MR) angiography detects a high incidence of persistent signal within treated PAVMs after embolotherapy [16]. This may be related to recanalization of the feeding vessel or reperfusion of the PAVM by an accessory artery or by systemic branches [13, 17, 18]. We report here three cases of reperfusion of complex large PAVMs after coil embolization and discuss the different mechanisms of reperfusion.
Case Reports
Case 1
An 18-year-old man with HHT had an exercise intolerance, cyanosis, hippocratic nails and epistaxis. Spiral computed tomography (CT) demonstrated a large complex PAVM located in the right lower lobe (Fig. 1A). Both lungs were involved by diffuse small or tiny PAVMs whose afferent arteries had a diameter less than 2 mm. Three feeding pedicles of the complex PAVM were confirmed by selective pulmonary angiography. Embolization of all the feeding arteries was successfully performed with a 5 Fr vertebral catheter using 45 steel coils with diameters ranging from 12 to 3 mm (Mreye embolization coils, Cook, Bjaeverskov, Denmark). All coils were carefully packed in order to prevent recanalization (Fig. 1B). The catheter tip was advanced to a point beyond any normal branches and immediately proximal to the venous sac. Before embolization the supine PaO2 was 47 mmHg on room air and the supine arterial oxygen saturation (SaO2) was 83%. After embolization a transitory right pleural effusion was noticed.
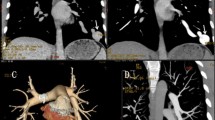
Preprocedure CT, embolization procedure and follow-up CT in an 18-year-old man with HHT. A Spiral CT (mediastinal window settings) reveals a large PAVM located in the right lower lobe. B Postembolization angiogram reveals no filling of the PAVM with satisfactory coil packing. C Follow-up spiral CT (lung window settings) shows significant enlargement of a small PAVM involving the middle lobe (arrow). D Selective catheterization of a large inferior phrenic artery demonstrated transpleural supply to the previously embolized PAVM of the right lower lobe.
At 18 months after embolization, the patient’s clinical status had improved, but both PaO2 and SaO2 were suboptimal (68 mmHg and 93%, respectively). On follow-up spiral CT, reperfusion of the previously embolized PAVM was detected. In addition, significant enlargement of a small PAVM involving the middle lobe and a large inferior right phrenic artery were observed (Fig. 1C). The angiographic procedure was then repeated. Embolization of the recanalized complex PAVM and of the recently enlarged PAVM of the middle lobe was carried out using six coils. Selective catheterization of a large inferior phrenic artery demonstrated transpleural supply to the previously embolized PAVM (Fig. 1D). No additional embolization was performed. After embolization, the PO2 and SaO2 increased to 82 mmHg and 98%, respectively. The patient is still asymptomatic 10 months after the second embolization and has not presented hemoptysis.
Case 2
A 6-year-old boy had dyspnea, cyanosis and hippocratic nails. He presented a hypoxic syncope while riding his bicycle. His PaO2 and SaO2 on room air were 52 mmHg and 79%, respectively. Spiral CT demonstrated a single complex PAVM of the right lower lobe (Fig. 2A). Pulmonary angiography demonstrated a complex large PAVM involving four different pedicles (Fig. 2B). Embolization of all the feeding arteries was successfully performed with a 5 Fr right coronary catheter using a total of 32 coils with diameters ranging from 8 to 5 mm (Fig. 2C). At 3 months after embolization, his clinical status improved and his PaO2 and SaO2 increased to 99 mmHg and 93%, respectively.
Preprocedure CT, embolization procedure and follow-up CT in a 6-year-old boy with a single complex PAVM of the right lower lobe. A Spiral CT (lung window settings) demonstrates a large complex PAVM located in the right lower lobe. B Right pulmonary angiogram reveals a large complex PAVM of the right lower lobe. C Embolization of all the feeding arteries was successfully performed using a total of 32 coils. D Follow-up spiral CT at 12 months after embolization shows incomplete regression of the previously embolized PAVM. E During a second embolization procedure, obvious reperfusion of the PAVM was related to partial recanalization of the main feeding artery. F Recruitment of adjacent initially normal arteries is also visible.
At 12 months after embolization, incomplete regression of the previously embolized PAVM was noticed on spiral CT (Fig. 2D). A second embolization procedure was performed. Reperfusion of the PAVM was related to partial recanalization of the main feeding pedicle and recruitment of adjacent initially normal arteries (Fig. 2E,F). A total of 23 coils were used to ensure complete occlusion of the PAVM. After embolization, his SaO2 increased from 93% to 98%. His clinical status improved with complete disappearance of cyanosis and hippocratic nails. With a 54 month follow-up, the patient remains asymptomatic. On contrast-enhanced spiral CT, permanent occlusion of PAVM was confirmed. Enlargement of bronchial and right inferior phrenic arteries was noticed but no embolization has been planned in this asymptomatic young boy.
Case 3
A 22-year-old woman was admitted after a car accident caused by sudden syncope. On arrival, she was cyanotic and had hippocratic nails. She had never presented epistaxis and no telangiectasia was found. Her arterial saturation and PaO2 on room air were 82% and 47 mmHg, respectively. She was diagnosed with two PAVMs: one large complex PAVM of the right lower lobe and one simple small PAVM of the left lower lobe (Fig. 3A). Large right bronchial arteries were also detected from the aortic arch to the level of the right inferior pulmonary vein (Fig. 3B). Pulmonary angiography demonstrated a complex PAVM involving multiple pedicles. Embolization of the six feeding arteries was successfully performed using 44 coils with diameters ranging from 5 to 3 mm. All coils were carefully packed in order to prevent recanalization. The simple PAVM of the left lower lobe was easily embolized using three coils (5 to 3 mm).
Preprocedure and postembolization CT in a 22-year-old woman with two PAVMs. A Spiral CT (lung window settings) reveals a large complex PAVM situated in the right lower lobe. B Large right bronchial arteries are visible at the level of the right inferior pulmonary vein (arrow). C On follow-up contrast-enhanced spiral CT (mediastinal window settings), a localized reperfusion is identified within the large PAVM (arrow). D The diameter of the right bronchial arteries has decreased (arrows).
At 20 months after embolization, her clinical status improved and the PaO2 and SaO2 increased to 93 mmHg and 98%, respectively. On follow-up contrast-enhanced spiral CT, a localized reperfusion was identified within the large PAVM (Fig. 3C). On the left side, enlargement of a small PAVM, not diagnosed initially, was noticed whereas the embolized PAVM had regressed. Surprisingly, the diameter of the bronchial arteries had decreased (Fig. 3D). The patient remains asymptomatic with disappearance of hippocratic nails and normal arterial blood gases and shunt studies.
Discussion
PAVMs are potentially dangerous because of the risk of rupture, bleeding or paradoxical emboli resulting in stroke or cerebral abscess [1, 2, 3, 19]. PAVMs can be classified as either simple or complex [1]. A simple PAVM consists of single or multiple feeding arteries originating from a single segmental artery [1, 5, 20]. In complex PAVMs, feeding arteries originate from two or more segmental arteries [1, 5, 20]. In patients with diffuse or large PAVMs, neurologic symptoms are almost inevitable [1, 2]. Transcatheter embolization prevents stroke and neurologic damage and is usually indicated in the presence of feeding arteries larger than 3 mm in diameter [8, 20]. It is thought that the arterial occlusion of a simple PAVM is technically easier and less time-consuming than that of a complex type [20].
The method of embolization has been extensively described [5, 6, 8, 9]. In essence it involves catheterization of the feeding vessels to a malformation, advancement of the catheter tip to a point beyond any branches to normal lung and immediately proximal to the dilated venous portion, followed by arterial occlusion using coils or balloons [5, 8, 11, 12, 13, 14]. When the feeding artery is too short to be safely embolized, occlusion of the aneurysmal sac of the PAVM itself should be considered [21, 22]. There are some differences in technique between centers, some catheterizing the feeding artery using 6 Fr or 7 Fr catheters, others performing catheterization mainly with a coaxial technique [5, 14, 22]. In addition, there is no consensus concerning the choice of embolization agent [5, 11, 12, 13, 14, 22].
Embolization can be performed using detachable balloons or steel coils. Most groups favor steel or platinum coils as the primary embolization agent. The choice of a coil of a correct size is critical: if it is too small, the coil may pass through the venous portion of the PAVM into the systemic circulation with potential disastrous consequences [14], while if it is too large, the coil may cause occlusion of proximal normal pulmonary arterial branches or may elongate leading to recanalization [11]. After placement of the first coil, additional coils must be positioned until blood flow to the PAVM has ceased [5, 14]. Packing of smaller coils in the center of the first-placed coil is mandatory to prevent recanalization. If the number of coils is not sufficient recanalization may also occur because of insufficient thrombosis formation [17, 18, 23]. Despite an appropriately packed coil embolization, recanalization was observed in our three patients. Cure of the PAVM is usually defined by the involution (thrombosis and regression) of the aneurysm with a residual fibrous scar on spiral CT [24]. The rate of recanalization is probably underestimated if the follow-up of patients includes only chest radiography [7, 17, 24].
Accessory abnormal pulmonary artery branches to the PAVM can be missed during the initial evaluation with CT or even at the time of embolization because of preferential flow to the PAVM. Postprocedural pulmonary angiography may allow a better detection of accessory branches supplying the PAVM. Another potential mechanism explaining reperfusion of embolized PAVMs is the recruitment of normal branches adjacent to the PAVM, as illustrated in our second case [7]. Persistent perfusion of a complex PAVM was not a clinically relevant problem in our patient, but the long-term morbidity is unknown. However, some patients have suffered a stroke because of recanalized PAVMs [15].
Imaging follow-up of treated patients as well as physiologic evaluation should be performed in order to document involution of embolized PAVMs but also to detect growth or enlargement of small PAVMs as demonstrated in cases 1 and 3 [24]. Small PAVMs can over time reach the threshold size for complications. In most patients with diffuse PAVMs, improvement of dyspnea, oxygenation and shunt fraction is often not complete. The residual shunt is believed to represent the shunt through small PAVMs [1]. Small branches supplying the embolized PAVM may be also missed during follow-up CT evaluation, particularly in the absence of contrast enhancement or because of coil-related artifacts [24]. Even if clinical and radiological evaluation is necessary, oxygen saturation tests are equally important to predict recurrence. Conversely, contrast echocardiography is probably too sensitive and remains positive in the majority of patients with successful occlusion of all angiographically visible vessels [25, 26].
With MR perfusion imaging, the residual enhancement of a treated PAVM is frequent (58% of cases) and considered as bronchial-artery-to-pulmonary-artery collateral flow [16]. Thus, bronchial artery hypertrophy has been identified as a cause of reperfusion of small residual aneurysm after embolization [17]. Bronchial-to-pulmonary artery anastomoses may enter the pulmonary circulation distal to the embolized artery supplying the scarred region of the obliterated PAVM and may lead to future recanalization [17]. The formation of systemic collaterals may place patients at risk for future hemoptysis [17, 27, 28]. A large phrenic artery was a transpleural supply to a previously embolized PAVM in our first two patients. Systemic supply to the PAVM may be a pre-existing condition revealed by the relative ischemia induced by the shunt, as demonstrated in our third patient. Surprisingly, regression of pre-existing systemic supply to the complex PAVM was observed in this patient. To our knowledge, such an observation has never previously been reported. Large systemic arteries may also develop after radiological or surgical treatment of PAVMs to supply the residual scar [24, 27, 28]. Although the incidence of a systemic supply to PAVM is low, its frequency is probably underestimated. Arteriography is not commonly performed in these patients and most patients are evaluated using unenhanced CT examinations [27]. CT angiography, particularly with the use of multidetector technology, allows characterization of the bronchial arterial system and improves detection of even tiny arteries [28]. The clinical impact of this left-to-left shunt of oxygenated blood is considered to be low but the risk of hemoptysis is unknown [18, 21, 26]. Systemic supply to the PAVM is highly significant during pregnancy or when the technique of pulmonary flow redistribution is used [3, 29, 30]. However, the strategy of bronchial artery embolization in patients with recurrent hemoptysis is yet to be determined [29, 31]. A case of hemoptysis persisting despite successful occlusion of a single PAVM has been reported [29]. The patient refused embolization of the bronchial arteries supplying the embolized PAVM and underwent right lower lobectomy. The risks of parenchymal necrosis following systemic embolization should be carefully evaluated, and the type and size of embolization agents carefully discussed [32].
Although embolization is a safe and effective treatment in the management of PAVMs, long-term follow-up of patients is mandatory to document aneurysmal regression of treated lesions and to detect growth of small PAVMs reaching the threshold size for neurologic emboli. Reperfusion and recurrence of treated PAVMs may occur because of recanalization of embolized arteries, recruitment of normal branches or development of a systemic arterial supply. When coils are used, it is important to perform the embolization as distally as possible in the feeding vessel to a PAVM, close to the venous sac, to avoid the occlusion of branches to normal lung and to reduce the rate of reperfusion. The value of spiral CT with dynamic contrast enhancement should be discussed during the follow-up of patients with large complex PAVMs.
References
JR Gossage G Kanj (1998) ArticleTitlePulmonary arteriovenous malformations: A state of the art review Am J Respir Crit Care Med 158 643–661 Occurrence Handle1:STN:280:DyaK1czmsFGlsA%3D%3D Occurrence Handle9700146
M Moussoutas P Fayad M Rosenblatt et al. (2000) ArticleTitlePulmonary arteriovenous malformation: Cerebral ischemia and neurological manifestations Neurology 55 959–964
ME Faughnan YW Lui JA Wirth et al. (2000) ArticleTitleDiffuse pulmonary arteriovenous malformations: Characteristics and prognosis Chest 117 31–38
RI White SuffixJr (1992) ArticleTitlePulmonary arteriovenous malformations: How do we diagnose them and why is it important to do so? Radiology 182 633–635
RI White SuffixJr A Lynch-Nylan P Terry et al. (1988) ArticleTitlePulmonary arteriovenous malformations: Technique and long-term outcome of embolotherapy Radiology 169 663–669 Occurrence Handle3186989
JMB Hugues DJ Allison (1990) ArticleTitlePulmonary arteriovenous malformations: The radiologist replaces the surgeon Clin Radiol 41 297–298
M Remy-Jardin L Watinne J Remy (1991) ArticleTitleTranscatheter occlusion of pulmonary arterial circulation and collateral supply: Failures, incidence and complications Radiology 180 699–705 Occurrence Handle1:STN:280:By6A3svns1A%3D Occurrence Handle1871280
TJ Haitjema TT Overtoom CJ Westerman JW Lammers (1995) ArticleTitleEmbolisation of pulmonary arteriovenous malformations: Results and follow-up in 32 patients Thorax 50 719–723 Occurrence Handle1:STN:280:BymD3MvmslQ%3D Occurrence Handle7570404
RI White SuffixJr JS Pollak JA Wirth (1996) ArticleTitlePulmonary arteriovenous malformations: Diagnosis and transcatheter embolotherapy J Vasc Interv Radiol 7 787–804
CL Shovlin JM Hugues (1996) ArticleTitleHereditary hemorrhagic telangiectasia N Engl J Med 334 330–332
JS Pollak (1994) ArticleTitleClinical results of transvenous systemic embolotherapy with a neuroradiologic detachable balloon Radiology 191 477–482
PB Terry RI White SuffixJr KH Barth SL Kaufman SE Mitchell (1983) ArticleTitlePulmonary arteriovenous malformations: Physiologic observations and results of therapeutic balloon embolization N Engl J Med 308 1197–1200
S Saluja I Sitko DW Lee J Pollak RI White SuffixJr (1999) ArticleTitleEmbolotherapy of pulmonary arteriovenous malformations with detachable balloons: Long-term durability and efficacy J Vasc Interv Radiol 10 883–889 Occurrence Handle1:STN:280:DyaK1Mzmt1Smug%3D%3D Occurrence Handle10435705
JAE Dutton JE Jackson JMB Hugues et al. (1995) ArticleTitlePulmonary arteriovenous malformations: Results of treatment with coil embolization in 53 patients AJR Am J Roentgenol 165 1119–1125 Occurrence Handle1:STN:280:BymD387ptl0%3D Occurrence Handle7572487
DW Lee RI White SuffixJr TK Egglin et al. (1997) ArticleTitleEmbolotherapy of large pulmonary arteriovenous malformations: Long-term results Ann Thorac Surg 64 930–940
Y Ohno H Hatabu D Takenaka S Adachi S Hirota K Sugimura (2002) ArticleTitleContrast-enhanced MR perfusion imaging and MR angiography: Utility for management of pulmonary arteriovenous malformations for embolotherapy Eur J Radiol 41 136–146
K Sagara N Miyazono H Inoue K Ueno H Nishida M Nakajo (1998) ArticleTitleRecanalization after coil embolotherapy of pulmonary arteriovenous malformations: Study of long-term outcome and mechanism for recanalization AJR Am J Roentgenol 171 1704
RI White SuffixJr (1998) ArticleTitleRecanalization after embolotherapy of pulmonary arteriovenous malformations: significance? Outcome? [letter] AJR Am J Roentgenol 170 727–730 Occurrence Handle1:STN:280:DyaK1c7ltFKlsQ%3D%3D Occurrence Handle9490963
BA Ference TM Shannon RI White SuffixJr M Zavin CM Burdge (1994) ArticleTitleLife-threatening pulmonary hemorrhage with pulmonary arteriovenous malformations and hereditary hemorrhagic telangiectasia Chest 106 1387–1390
RI White SuffixJr SE Mitchell KH Barth et al. (1983) ArticleTitleAngioarchitecture of pulmonary arteriovenous malformations: An important consideration before embolotherapy AJR Am J Roentgenol 140 681–686
MG Tal S Saluja KJ Henderson RI White SuffixJr (2002) ArticleTitleVein of Galien technique for occluding the aneurysmal sac of pulmonary arteriovenous malformations J Vasc Interv Radiol 13 1261–1264
HP Dinkel J Triller (2002) ArticleTitlePulmonary arteriovenous malformations: Embolotherapy with superselective coaxial catheter placement and filling of venous sac with Guglielmi detachable coils Radiology 223 709–714
JA Clark RA Pugash (1998) ArticleTitleRecanalization after coil embolization of pulmonary arteriovenous malformations [letter] AJR Am J Roentgenol 171 1426
J Remy M Remy-Jardin L Watinne C Deffontaines (1992) ArticleTitlePulmonary arteriovenous malformations: Evaluation with CT of the chest before and after treatment Radiology 182 809–816 Occurrence Handle1:STN:280:By2C2MbjvVU%3D Occurrence Handle1535899
B Barzilai AD Waggoner C Spessert D Picus D Goodenberger (1991) ArticleTitleTwo-dimensional contrast echocardiography in the detection and follow-up of congenital pulmonary arteriovenous malformations Am J Cardiol 68 1507–1510
WL Lee AF Graham RA Pugash et al. (2003) ArticleTitleContrast echocardiography remains positive after treatment of pulmonary arteriovenous malformations Chest 123 351–358
KJ Laffey B Thomashow A Jaretzki SuffixIII EC Martin (1985) ArticleTitleSystemic supply to a pulmonary arteriovenous malformation: A relative contraindication to surgery AJR Am J Roentgenol 145 720–722
I Hasegawa P Boiselle H Hatabu (2004) ArticleTitleBronchial artery dilatation on MDCT scans of patients with acute pulmonary embolism Radiology 182 67–72
JF Wispelaere ParticleDe JP Trigaux P Weynants M Delos B Coene ParticleDe (1996) ArticleTitleSystemic supply to a pulmonary arteriovenous malformation: Potential explanation for recurrence Cardiovasc Intervent Radiol 19 285–287
T Shannon J Pollak RI White SuffixJr (1992) ArticleTitleRedistribution of pulmonary blood flow by embolotherapy: A new method for improving oxygenation in patients with diffuse pulmonary arteriovenous malformations [abstract] Am Rev Respir Dis 145 600A
W Yoon JK Kim YH Kim TW Chung HK Kang (2002) ArticleTitleBronchial and nonbronchial systemic artery embolization for life-threatening hemoptysis: A comprehensive review Radiographics 22 1395–1409
KH Do JM Goo JG Im KW Kim JW Chung JH Park (2001) ArticleTitleSystemic arterial supply to the lungs in adults: Spiral CT findings Radiographics 21 387–402
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lacombe, P., Lagrange, C., Hajjam, M.E. et al. Reperfusion of Complex Pulmonary Arteriovenous Malformations After Embolization: Report of Three Cases. Cardiovasc Intervent Radiol 28, 30–35 (2005). https://doi.org/10.1007/s00270-003-0263-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-003-0263-y