Abstract
The purpose of this study was to determine the incidence of central vein stenosis and occlusion following upper extremity placement of peripherally inserted central venous catheters (PICCs) and venous ports. One hundred fifty-four patients who underwent venography of the ipsilateral central veins prior to initial and subsequent venous access device insertion were retrospectively identified. All follow-up venograms were interpreted at the time of catheter placement by one interventional radiologist over a 5-year period and compared to the findings on initial venography. For patients with central vein abnormalities, hospital and home infusion service records and radiology reports were reviewed to determine catheter dwell time and potential alternative etiologies of central vein stenosis or occlusion. The effect of catheter caliber and dwell time on development of central vein abnormalities was evaluated. Venography performed prior to initial catheter placement showed that 150 patients had normal central veins. Three patients had central vein stenosis, and one had central vein occlusion. Subsequent venograms (n = 154) at the time of additional venous access device placement demonstrated 8 patients with occlusions and 10 with stenoses. Three of the 18 patients with abnormal follow-up venograms were found to have potential alternative causes of central vein abnormalities. Excluding these 3 patients and the 4 patients with abnormal initial venograms, a 7% incidence of central vein stenosis or occlusion was found in patients with prior indwelling catheters and normal initial venograms. Catheter caliber showed no effect on the subsequent development of central vein abnormalities. Patients who developed new or worsened central vein stenosis or occlusion had significantly (p = 0.03) longer catheter dwell times than patients without central vein abnormalities. New central vein stenosis or occlusion occurred in 7% of patients following upper arm placement of venous access devices. Patients with longer catheter dwell time were more likely to develop central vein abnormalities. In order to preserve vascular access for dialysis fistulae and grafts and adhere to Dialysis Outcomes Quality Initiative guidelines, alternative venous access sites should be considered for patients with chronic renal insufficiency and end-stage renal disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The number of upper extremity peripherally inserted central catheters (PICCs) and venous infusion ports placed by interventional radiologists has grown substantially over the past several years. In many institutions, these devices are replacing neck or chest wall central venous catheters (CVC) as the access of choice for intermediate and long-term intravenous therapy.
There are several reasons for the growing popularity of these devices. Most importantly, peripherally inserted venous access devices (VAD) offer a safe, efficient, and cost-effective alternative to surgically placed CVCs [1 2]. They not only provide reliable and convenient venous access for in-hospital use, but for home therapy as well. VADs are ideal for infusion of toxic, viscous, and irritating substances such as chemotherapeutic agents, total parenteral nutrition, and antibiotics, respectively. These devices are well tolerated by patients and widely accepted throughout the medical community.
At our institution, we currently place, each year, approximately 1,250 PICCs and 200 ports in the upper extremity mainly for protracted intravenous therapy. Because the placement of these devices has become so common, we evaluated patients with prior upper arm VADs by venography to assess for subsequent development of central vein abnormalities.
Materials and Methods
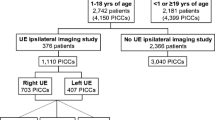
Our radiology department information system was searched for patients who underwent upper extremity venography in conjunction with placement of an upper arm PICC or venous port and subsequently had an ipsilateral venogram prior to additional VAD insertion between July 1995 and May 2000. Only patients with follow-up venograms interpreted by one experienced, CAQ-certified vascular-interventional radiologist (DJE) were selected. The follow-up venograms were interpreted without prior knowledge of the initial venogram findings. Patients were excluded from the study if they had previous dialysis grafts, fistulae, or catheters on the same side as the PICC or port (n = 14). Eighty-four men and 70 women met these criteria and were included in the study. Patient ages ranged from 15 to 96 (mean 53) years. Our department chairman obtained Institutional Review Board approval for all retrospective studies requiring review of medical records.
All upper extremity VADs were placed under fluoroscopic guidance using previously described techniques [3]. From July 1992 to September 1999, upper extremity venograms were routinely performed in all patients with peripheral intravenous access prior to placement of upper arm VADs. Prior to 1993, venograms were performed using iodinated contrast media. After 1993, venograms were primarily performed using carbon dioxide [4 5 6]. Venography was performed by hand injecting contrast or carbon dioxide through a peripheral intravenous line. Beginning in September 1999, venography was reserved for those patients who had a prior central VAD or pacemaker inserted in the same arm or ipsilateral hemithorax. Ultrasound guidance was used for patients without peripheral intravenous access. Patients who had VADs placed under ultrasound guidance were excluded from this study since venography was not performed.
PICCs were placed in four patients who had central vein abnormalities present on initial venography. The three patients with central vein stenosis presumably had a known or high likelihood of having a contralateral central vein abnormality; hence, VAD placement proceeded despite the venographic findings. Likewise, a patient with central superior vena cava (SVC) occlusion had limited options for VAD placement. All VADs were inserted via the upper arm brachial or basilic veins. The catheters were generally placed in the nondominant arm to hopefully reduce morbidity in case a symptomatic central vein stenosis or occlusion would develop. Catheter tips were positioned in the central SVC or at the cavoatrial junction. Because of the retrospective nature of this study, the indications for VAD placement were not known for all patients. However, indications were determined for a subset of patients with normal venograms (n = 31) who were followed by our institution’s home infusion service and for those who developed central vein stenosis or occlusion.
The reports of initial and subsequent venograms were compared to determine the development or progression of central vein stenoses or occlusions following VAD placement. The central veins were defined as the axillary, subclavian, and brachiocephalic veins along with the SVC. The upper arm veins were not evaluated because of the variable venous opacification seen at this site, largely based on the location of the peripheral intravenous access used to inject iodinated contrast or carbon dioxide. The incidence of new or progressive central vein abnormalities was compared to catheter caliber and duration of catheter placement (dwell time).
Catheter dwell time could not be ascertained for all patients in this retrospective study, since many were not treated through our institution’s home infusion service. However, the average catheter dwell time was calculated for a subset of patients with normal venograms who were followed by our institution’s home infusion service (n = 31), and complications were recorded. Medical records, home infusion service records, and radiology reports were reviewed for those patients who developed central vein stenosis and occlusion to determine indications for catheter placement, catheter dwell time, symptoms, and to assess for additional etiologies of central vein abnormalities. Placement of other CVCs or transvenous cardiac pacemakers and extrinsic causes of venous stenosis or occlusion were noted. The Wilcoxon Two-Sample Test was used to evaluate the impact of dwell time on subsequent development of central vein stenosis or occlusion.
Table 1 summarizes the catheter caliber and devices placed in these patients. PICCs were placed in 149 patients. Prior to December 1998, we routinely placed 4 Fr single lumen or 7 Fr double lumen PICCs (Cook Inc., Bloomington, IN). After that date we routinely placed 4 Fr single lumen or 6 Fr double lumen Vaxcel PICCs (Boston Scientific, Natick, MA). An occasional 5 Fr single lumen or double lumen PICC from either manufacturer was placed based on product availability. For the 5 patients in this study who underwent venous port placement, a 5.2F Mini Vital port (Cook) was used. Fischer’s Exact Test was performed to assess significance of catheter caliber on subsequent development of central vein stenosis or occlusion.
Results
One hundred seven left (69%) and 47 right (31%) upper extremity venograms were performed at the time of initial VAD placement. Of these, 150 (97%) were interpreted as normal, 3 (2%) revealed a central vein stenosis, and 1 (1%) demonstrated central SVC occlusion, a widely patent peripheral SVC and a prominent azygous vein (Table 2). The severity of the underlying central vein stenosis was not delineated in the reports for patients 8 and 17 (Table 2), and the images were not available for review.
The interval between initial venography and follow-up venography ranged from 3 days to 54 months (mean 19.4 months). Follow-up venograms (n = 154) at the time of subsequent VAD placement demonstrated abnormalities in 18 patients. There were 8 central vein occlusions and 10 central vein stenoses (Table 2). Two patients with central vein stenosis on initial venography progressed to occlusion. Subsequent venography showed progression of a brachiocephalic vein stenosis from 40% to 90% in another patient. One patient with central SVC occlusion on initial venography developed occlusion of the peripheral SVC and right brachiocephalic and subclavian veins. Four of the 38 (11%) patients with 7 Fr PICCs and 14/102 (13%) patients with 4 Fr PICCs developed central vein stenosis or occlusion. None of the 5 patients with ports developed central vein abnormalities.
Of the 18 patients who developed central vein abnormalities, 13 were men and 5 were women (age range 38–76, mean 57). Eight (44%) patients required PICC placement for infection, 8 (44%) for neoplasm, and 2 (11%) for complications related to renal transplantation (Table 2). In the 31 patients (11 men, 20 women), ages 31–94, mean 52 who did not develop central vein abnormalities following VAD placement, 14 (45%) required PICC placement for infection, 12 (39%) for neoplasm, 2 (7%) for inflammatory bowel disease, 1 (3%) for hemophilia, and 2 (7%) for cardiac disease requiring multiple medications. The indications for VAD placement were similar for both groups of patients.
Following review of patient records, 3 of the 18 patients with abnormal follow-up venograms were found to have potential alternative causes of central vein stenosis or occlusion: 2 had temporary subclavian CVCs between the initial and follow-up venograms and 1 had a transvenous cardiac pacemaker placed via the axillary vein following removal of the initial PICC. All 3 patients had normal initial venograms. We cannot be certain whether the initial upper arm VAD or these subsequent devices were the cause of the central vein abnormalities. However, the ability to place these subsequent devices suggests that the central veins may have been normal at the time of catheter or pacemaker placement. Excluding these 3 patients with potential alternative causes of central vein stenosis and the 4 patients with abnormal initial venograms, the incidence of central vein stenosis or occlusion was 7% (n = 11) in patients with normal venograms prior to VAD placement. Seven (4.8%) patients developed central vein stenosis, and 4 (2.7%) patients developed central vein occlusion.
The catheter dwell time was determined for 15/18 (83%) patients with central vein abnormalities on follow-up venography (Table 2). Dwell times could not be determined for 3 patients who were not followed by our home infusion service. For this group of patients, catheter dwell times ranged from 4 to 424 days (mean 138, median 90, SD 143). The catheter dwell time for 31 (23%) of the patients without central vein abnormalities who were followed by our home infusion service ranged from 6 to 568 days (mean 68, median 33, SD 115). Catheter dwell times were significantly longer (p = 0.03) in patients who developed new or worsened central vein abnormalties suggesting a positive correlation between dwell time and subsequent development of central vein stenosis or occlusion.
At the time of subsequent VAD placement, none of the patients with central vein abnormalities had symptoms of central vein obstruction.
Discussion
VAD complications most commonly reported include infection, catheter malfunction, inadvertent removal and venous thrombosis [1 9 10 11 12 13]. In previous studies, the incidence of venous thrombosis following PICC or port placement has been reported to be between approximately 3% and 38% [2 9 11]. The mechanism behind intravascular thrombosis is best explained by Virchow’s theory of thrombotic pathogenesis, which postulates that intravascular thrombosis is caused by endothelial damage due to local trauma or inflammation of the vessel wall, stasis of blood flow and hypercoagulable states. All three mechanisms of acute thrombus formation may apply to indwelling intravenous catheters [14].
The outcome of acute thrombus will determine the lasting effects these catheters have on the venous system. Complete resolution of thrombus may leave the vein wall intact without intimal injury. Partial lysis and recanalization of thrombus may result in a thickened vein wall and venous stenosis [14]. Organization of thrombus may cause stenosis or chronic venous occlusion. In the present study, we found a 7% incidence of new central vein stenosis or occlusion in patients with prior indwelling peripheral VADs. In our study, 2 patients with renal disease developed central vein stenosis or occlusion due to VAD placement, precluding use of that upper extremity for future dialysis access. This emphasizes the importance of avoiding use of upper extremity veins in patients with end-stage renal disease (ESRD) or chronic renal insufficiency (CRI) for VAD placement who may be dependent on long-term venous access for hemodialysis.
The National Kidney Foundation-Dialysis Outcome Quality Initiative (NKF-DOQI) guidelines state that “hemodialysis access failure is a major cause of morbidity” for patients requiring hemodialysis [15]. With native fistulae offering 4–5 year patency rates and synthetic grafts offering at best 3–5 year patency rates [15], dialysis patients require multiple venous accesses over the course of a lifetime. NKF-DOQI venous access guideline #7 states that all “arm veins suitable for placement of vascular access should be preserved” and “should not be used for venipuncture or intravenous catheters” [15]. This guideline should be followed for all “patients with progressive kidney disease (creatinine >3 mg/dL), and all patients with conditions likely leading to ESRD” [15]. Failure to adhere to these guidelines may preclude the placement of dialysis catheters, grafts and native fistulae in current and future dialysis patients [16 17 18].
Ideally, central venous catheters should be avoided in patients with ESRD and CRI, however impractical. These patients commonly have multiple co-morbid conditions that require frequent hospital admissions and reliable intravenous access for various medications, along with catheter placements for hemodialysis. An acceptable form of venous access for this patient population is the insertion of tunneled internal or external jugular catheters. Sasadeusz et al. [19] recently reported placement of 43 tunneled PICCs in 34 patients with no reported symptoms of venous thrombosis [19].
Although we found no relationship between catheter size and venous abnormalities in the current study, which may be due to the small number of patients who developed central vein abnormalities, a report by Grove and Pevec [10] showed a significant, linear relationship between catheter size and venous thrombosis rates. The authors reported a 1%, 6.6% and 9.8% venous thrombosis rate for 4-F, 5F and 6-F catheters placed in upper arm veins, respectively. They also demonstrated that small-bore catheters are less likely to cause intravascular thrombosis than larger catheters. In addition, studies have shown an increased thrombosis risk with catheter tips located within the peripheral two-thirds of the SVC [12 20]. Therefore, catheter tips should be placed in the central SVC or at the cavoatrial junction where blood flow and vein diameter are the greatest [12 20].
Catheter dwell times were significantly longer in patients who developed new or worsened central vein abnormalities, suggesting a positive correlation between dwell time and subsequent development of central vein stenosis or occlusion. However, due to the small sample size of patients who developed central vein stenosis or occlusion, this finding should be confirmed in larger prospective studies.
In summary, we found that patients with a normal central venogram who undergo placement of a PICC or venous infusion port in the upper arm have a 7% risk of developing central vein stenosis or occlusion. Those who developed central vein abnormalities were asymptomatic. When possible, peripheral VADs should be avoided in ESRD and CRI patients in order to preserve arm veins for construction of native fistulae or graft placement as hemodialysis access.
References
JF Cardella PS Fox JB Lawler (1993) ArticleTitleInterventional radiologic placement of peripherally inserted catheters. JVIR 4 653–660 Occurrence Handle8219560
MJ Foley (1995) ArticleTitleRadiologic placement of long-term central venous peripheral access system ports (PAS Port): Results in 150 patients. JVIR 6 255–262 Occurrence Handle7787360
DM Hovsepian J Bonn DJ Eschelman (1993) ArticleTitleTechniques for peripherally inserted central venous catheters. JVIR 4 795–803 Occurrence Handle8281003
KL Sullivan J Bonn MJ Shapiro GA Gardiner (1995) ArticleTitleVenography with carbon dioxide as a contrast agent. CVIR 18 141–145
J Bonn DJ Eschelman KL Sullivan GA Jr. Gardiner (1994) ArticleTitlePeripheral insertion of central venous catheters guided by means of carbon dioxide contrast agents. JVIR 5 32
ST Hahn T Pfammatter KJ Cho (1995) ArticleTitleCarbon dioxide gas as a venous contrast agent to guide upper-arm insertion of central venous catheters. CVIR 18 146–149
PC Shetty MK Mody DJ Kastan RP Sharma MW Burke C Venugopal TH Burke (1997) ArticleTitleOutcome of 350 implanted chest ports placed by interventional radiologists. JVIR 8 IssueID6 991–995
KR Simpson DM Hovsepian D Picus (1997) ArticleTitleInterventional radiologic placement of chest wall ports: Results and complications in 161 consecutive placements. JVIR 8 189–195 Occurrence Handle9083981
JF Cardella K Cardella N Bacci PS Fox JH Post (1996) ArticleTitleCumulative experience with 1,273 peripherally inserted central catheters at a single institution. JVIR 7 5–13 Occurrence Handle8773968
JR Grove WC Pevec (2000) ArticleTitleVenous thrombosis related to peripherally inserted central catheters. JVIR 11 IssueID7 837–840 Occurrence Handle10928518
AW Allen JL Megargell DB Brown FC Lynch H Singh Y Singh PN Waybill (2000) ArticleTitleVenous thrombosis associated with the placement of peripherally inserted central catheters. JVIR 11 IssueID10 1309–1314 Occurrence Handle11099241
MA Ryder (1993) ArticleTitlePeripherally inserted central venous catheters. Nurs Clin North Am 28 IssueID4 937–971
L Balestreri M DeCicco M Matovic F Coran S Morassut (1995) ArticleTitleCentral venous catheter-related thrombosis in clinically significant symptomatic oncologic patients. Eur J Radiol 20 108–111 Occurrence Handle10.1016/0720-048X(95)00633-2 Occurrence Handle7588863
MD Karim Valji (1999) Vascular and Interventional Radiology WB Saunders Philadelphia 320
Dialysis Outcome Quality Initiative Guidelines for Vascular Access (2001) American Journal of Kidney Disease, Vol. 37, No. 1 (Suppl 1) S141–S149
LU Mailloux B Napolitano AG Bellucci M Vernace BM Wilkes RT Mossey (1994) ArticleTitleRenal vascular disease causing end-stage renal disease, incidence, clinical correlates, and outcomes: A 20-year clinical experience. Am J Kidney Dis 24 IssueID4 622–629 Occurrence Handle7942820
AH Mokdad ES Ford BA Bowman DE Nelson MM Engelgau JS. Vinic Marks (2001) ArticleTitleThe continuing increase of diabetes in the US. Diabetes Care 24 IssueID2 412
InstitutionalAuthorNameHealth Care Food Nutr Focus (2001) ArticleTitleDiabetes in the United States. It is still on the rise, according to the CDC’s latest report . 17 3–4
KM Sasadeusz SO Trerotola H Shah J Namyslowski MS Johnson KP Moresco NH Patel (1999) ArticleTitleTunneled jugular small-bore central catheters as an alternative to peripherally inserted central catheters for intermediate-term venous access in patients with hemodialysis and chronic renal insufficiency. Radiology 213 303–306 Occurrence Handle10540677
JK Brown-Smith MH Stoner (1990) ArticleTitleTunnelled catheter thrombosis: Factors related to incidence. Oncol Nurs Forum 17 543 Occurrence Handle2399167
ML Goodwin I Carlson (1993) ArticleTitleThe peripherally inserted central catheter. J Int Nurs 16 IssueID2 92–99
JJ Crowley JK Pereira LH Harris CJ Becker (1997) ArticleTitlePeripherally inserted central catheters: Experience in 523 children. Radiology 204 617–621 Occurrence Handle1:STN:280:ByiH38vjtFY%3D Occurrence Handle9280234
EH Kincaid PW Davis MC Chang JM Fenstermaker TC Pennell (1999) ArticleTitle“Blind” placement of long-term central venous access devices: Evaluation of 589 consecutive procedures. Am Surg 65 IssueID6 520–523 Occurrence Handle1:STN:280:DyaK1M3pt1ehtQ%3D%3D
MC Horattas J Trupiano S Hopkins D Pasini C Martino A Murty (2001) ArticleTitleChanging concepts in long-term central venous access: Catheter selection and cost savings. Am J Inf Contr 29 32–40 Occurrence Handle10.1067/mic.2001.111536
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gonsalves, C., Eschelman, D., Sullivan, K. et al. Incidence of Central Vein Stenosis and Occlusion Following Upper Extremity PICC and Port Placement . CVIR 26, 123–127 (2003). https://doi.org/10.1007/s00270-002-2628-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-002-2628-z