Abstract
Background
Our objective was to compare the surgical staff’s feelings of fatigue between laparoendoscopic single-site adrenalectomy (LESS-A) and conventional laparoscopic adrenalectomy (CLA) before and after surgery.
Method
Data were collected for surgical procedures performed between June 2011 and September 2017 (57 LESS-A and 37 CLA). Each procedure in both groups was performed by the same chief surgeon. The subjective fatigue feelings of the key members of the surgical team (chief surgeon, scopist, assistant surgeon) were assessed using the “Jikaku-sho shirabe” questionnaire, which contained questions about work-related feelings of fatigue. It consisted of 25 subjective items for 5 factors drawn from factor analysis (drowsiness, instability, uneasiness, local pain or dullness, and eyestrain). For each item, the participants were requested to estimate the intensity of their feelings using a five-point rating scale before and after surgery.
Results
There was no significant difference in operative time (p = 0.231) between the LESS-A and CLA procedure groups. For the chief surgeon, local pain or dullness (p = 0.603) and eyestrain (p = 0.086) were similar between the LESS-A and CLA procedures. The scopists and assistant surgeons in the LESS-A group did not suffer local pain or dullness (p = 0.793 and p = 0.240, respectively). They did, however, suffer more eyestrain than those in the CLA group (p = 0.001 and p = 0.001, respectively).
Conclusion
Although LESS-A is generally considered to be a technically difficult procedure, the results of this study demonstrate that the feelings of physical fatigue are roughly equivalent between LESS-A and CLA procedures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic surgery has become the standard for many surgical interventions as there is less postoperative pain, recovery is faster, the hospital stay is shorter, and cosmetic outcomes are improved compared with open surgery [1,2,3]. Surgical procedures involve a complex series of manual and psychological tasks that can require precise hand–eye coordination. They include lengthy and demanding cognitive tasks in which attention, memory, and response time play very important roles. Surgeons need to maintain concentration during surgery in order to avoid complications, but fatigue can make this difficult [4]. It has thus been suggested that surgeons may sometimes consider musculoskeletal problems they have experienced during surgery when selecting a surgical approach [5].
The field of minimally invasive surgery (MIS) is constantly evolving. Novel techniques, such as laparoendoscopic single-site (LESS) surgery, typically have greater benefits for the patient than the surgeon [6]. LESS urologic surgery minimizes postoperative wound pain and improves cosmetic outcomes [7]. It has been performed for various urological diseases, and studies have shown that, compared with conventional laparoscopic surgery, there is less pain, shorter hospital stays, and excellent cosmetic outcomes [8]. A previous study on the effect of the patient’s opinion on the approach selected for urologic MIS found that young women prefer MIS such as transumbilical LESS surgery [9]. However, LESS surgery is technically challenging, which limits its widespread application [10]. The surgeon faces many difficulties that are not present in conventional laparoscopic procedures, including the lack of instrument triangulation, collisions between instrument shafts, and the need for ambidexterity [11]. LESS surgery may thus impose a greater physical workload on surgeons than conventional laparoscopic surgery.
The objective of this study was to compare the feelings of fatigue between laparoendoscopic single-site adrenalectomy (LESS-A) and conventional laparoscopic adrenalectomy (CLA) for each of the key members of the surgical team (chief surgeon, scopist, assistant surgeon) before and after surgery.
Methods
Data collection
Data were prospectively collected for surgical procedures (57 LESS-A and 37 CLA) performed between June 2011 and September 2017 at Hiroshima University Hospital. Each procedure in both groups was performed by the same chief surgeon (S.I.) with the assistance of a scopist, an assistant surgeon, and other surgical staff. (S.I. had previously performed only three CLA procedures and ten LESS-A procedures.) The LESS-A procedures were performed between June 2011 and March 2016. To establish a control group, the same surgeon performed CLA procedures on 37 patients between November 2012 and September 2017. Thirty-three of the CLA procedures (89%) were performed after the period during which the LESS-A ones were performed; that is, the CLA procedures were performed mainly in the latter half of the data collection period. There were 3 scopists and 15 assistant surgeons in the LESS-A group and 10 scopists and 15 assistant surgeons in the CLA group. All participants consented to take part in this study. The team positioning during the LESS-A procedures is illustrated in Fig. 1. The scopist sat while everyone else stood. The team positioning during CLA procedures was similar to LESS-A procedure except that everyone including the scopist stood. Figure 2 shows the port placement in CLA procedure.
Protocol
The subjective feelings of fatigue of the key members of the surgical team were assessed before and after surgery by using the “Jikaku-sho shirabe” questionnaire (Table 1) [12] assembled by the Industrial Fatigue Research Committee of Japanese Occupational Health. It was designed to assess fatigue and has been widely used in Japan as a reliable tool to assess fatigue in workers [13, 14], including nurses and care workers [15, 16] and surgeons [17]. It consists of 25 subjective items for 5 factors (I: feeling of drowsiness; II: feeling of instability; III: feeling of uneasiness; IV: feeling of local pain or dullness; V: feeling of eyestrain). For each item, the participants were asked to estimate the intensity of their feeling using the following scale: “disagree completely”, “agree scarcely”, “agree slightly”, “agree considerably”, and “agree strongly”. These five intensities were assigned scores of 1–5 points, respectively (maximum: 125 points).
This research protocol was approved by the Institutional Review Board of Hiroshima University Hospital (IRB No. 449). Informed consent was confirmed by the IRB.
Statistical analysis
Only the data for complete responses both before and after each surgical procedure were analysed. The total number of points for all items was defined as the perceived level of fatigue. The higher the fatigue level (i.e. score), the higher the degree of fatigue due to surgery.
The data were analysed in accordance with each approach using the chi-squared test and the Mann–Whitney U test. For all tests, a p value of < 0.05 was considered statistically significant. All values are shown as means. The survey data were analysed using Wilcoxon’s signed rank sum test and the Mann–Whitney U test. They were also analysed using JMP 15 software (SAS Institute, Cary, NC, USA).
Results
Surgeon characteristics
As mentioned, all the procedures in both groups were performed by the same chief surgeon. The age of the chief surgeon and mean age of the assistant surgeons were significantly lower for the LESS-A group than for the CLA group (38.3 vs. 41.8 years, p = 0.001; 31.1 vs. 34.1 years, p = 0.011). In contrast, the mean age of the scopists was higher for the LESS-A group than for the CLA group (43.1 vs. 37.3 years, p = 0.001) (Table 2).
Demographic characteristics
There were no conversions to open surgery for any of the procedures. However, one LESS-A procedure was converted to a CLA procedure due to the need to place three additional trocars to repair an inferior vena cava injury. This case was excluded from the study. There were no significant between-group differences in patient characteristics. The operative time was 112.1 min for the LESS-A group and 104.0 min for the CLA group (p = 0.231). Estimated blood loss was higher for the CLA group than for the LESS-A group (80.3 ml vs. 28.4 ml; p = 0.064) (Table 3).
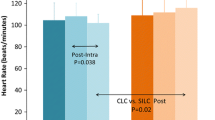
Between-group comparison of fatigue scores before and after surgery
We compared the overall fatigue scores between the LESS-A and CLA groups before and after surgery (Fig. 3) and found no significant differences in the overall scores for the chief surgeon (p = 0.115), scopists (p = 0.231), and assistant surgeons (p = 0.775). That is, the overall fatigue score was roughly equivalent between the LESS-A and CLA groups for each of the key members of the surgical team (chief surgeon, scopist, and assistant surgeon).
The fatigue scores before and after surgery by the five factors are shown in Fig. 4. There were no significant between-group differences in the scores for local pain or dullness before and after surgery for the chief surgeon. The score increased from 5.91 to 16.98 for the LESS-A group and from 5.13 to 16.73 for the CLA group (p = 0.603). There were also no significant between-group differences for the scopists (p = 0.793) and assistant surgeons (p = 0.240). Although the LESS-A procedure is considered to be technically difficult, these results indicate that local pain or dullness was roughly equivalent between the LESS-A and CLA procedures for all of the key members of the surgical team (chief surgeon, scopist, and assistant surgeon).
There were no significant between-group differences in the scores for eyestrain before and after surgery for the chief surgeon (p = 0.086); these scores increased significantly more for the LESS-A group for the scopists (p = 0.001) and assistant surgeons (p = 0.001). There was also no significant between-group difference in the scores for drowsiness before and after surgery for the chief surgeon (p = 0.787); these scores increased significantly more for the CLA group for the scopists (p = 0.001) and assistant surgeons (p = 0.013). These results indicate that a LESS-A procedure tends to create severe eyestrain for the scopist and assistant surgeon but not drowsiness.
There were no significant between-group differences in the scores for instability before and after surgery for the chief surgeon (p = 0.115) and scopists (p = 0.752); the scores were significantly higher for the CLA group for the assistant surgeons (p = 0.001). The scores for uneasiness were significantly higher before and after surgery for the CLA group for the chief surgeon (p = 0.001) and scopists (p = 0.001); there was no significant difference in these scores for the assistant surgeons (p = 0.637).
In addition, with the aim of investigating the effect of aging by the chief surgeon, we divided the data collection period into 2 equal sub-periods. We then compared the increases in the feelings of fatigue between sub-periods (data not shown). The increases in the score for local pain or dullness were significant for both sub-periods for the LESS-A group. It was greater for the second sub-period (from 6.00 to 18.62) than for the first (from 5.82 to 15.29) (p = 0.007). For the CLA group, there was no significant difference between sub-periods (p = 0.081).
We also compared the feeling of eyestrain between sub-periods. For the LESS-A group, the score increased significantly more for the second sub-period (from 5.34 to 11.21) than for the first sub-period (from 5.21 to 8.00) (p = 0.001). Again, for the CLA group, there was no significant difference between sub-periods (p = 0.368).
Consideration of factors that affected fatigue score
We divided the patients on the basis of whether their tumour was pheochromocytoma or non-pheochromocytoma for the purpose of investigating the effect of the patient’s condition on the feelings of fatigue. Tumour size was significantly larger in the patients with pheochromocytoma (39.7 vs. 21.1 mm; p = 0.001); however, there were no significant differences in the insufflation time (p = 0.558) and estimated blood loss (p = 0.218) between the two conditions. For the LESS-A group, there was no significant difference in the evaluation of the overall scores for feelings of fatigue between conditions for the chief surgeon (p = 0.054), scopists (p = 0.564), and assistant surgeons (p = 0.421). For the CLA group, there was no significant difference in the overall fatigue scores for the chief surgeon (p = 0.154) and scopists (p = 0.938), whereas these scores were significantly higher for the pheochromocytoma condition for the assistant surgeons (p = 0.040). For the patients with pheochromocytoma, the overall fatigue scores were significantly lower in the LESS group than the CLA group for the chief surgeon (p = 0.010), whereas there was no significant difference in the overall fatigue scores between both groups for the scopists (p = 0.303) and assistant surgeons (p = 0.068). For the patients with non-pheochromocytoma, there was no significant difference in the overall fatigue scores for the chief surgeon (p = 0.648) and assistant surgeons (p = 0.108), whereas the overall fatigue scores were significantly lower in the LESS group than the CLA group for the scopists (p = 0.034) (Fig. 5a).
Furthermore, we divided the patients on the basis of whether their tumour was large (> 5 cm) or small. For the LESS-A group, there was no significant difference in the overall fatigue scores for the chief surgeon (p = 0.860) and assistant surgeons (p = 0.593), whereas the scores were significantly higher for the large tumour condition for scopists (p = 0.028). For the CLA group, there was no significant difference in the overall fatigue scores for the chief surgeon (p = 0.163) and scopists (p = 0.890), whereas the scores were significantly higher for the large tumour condition for the assistant surgeons (p = 0.014). For the patients with the large tumour, there was no significant difference in the overall fatigue scores between the LESS-A and the CLA for the chief surgeon (p = 0.153), scopists (p = 0.487) and assistant surgeons (p = 0.109). For the patients with the small tumour, there was no significant difference in the overall fatigue scores between both groups for the chief surgeon (p = 0.234), whereas the overall fatigue scores were significantly lower in the LESS group than the CLA group for the scopists (p = 0.017) and assistant surgeons (p = 0.026) (Fig. 5b).
We also divided the patients on the basis of whether their bleeding was massive (> 200 mL) or not. For the LESS-A group, there were no cases in which the bleeding was massive. For the CLA group, there was no significant difference in the overall fatigue scores between massive and non-massive bleeding for the chief surgeon (p = 0.320), scopists (p = 0.754), and assistant surgeons (p = 0.573).
Comparison of scores between groups in terms of sense of accomplishment
The sense of accomplishment was assigned scores of 1–5 points by each of the key members of the surgical team only after surgery. We compared the scores between groups (Fig. 6) and found them to be significantly higher for the LESS-A group than the CLA group for the chief surgeon (4.11 vs. 3.10; p = 0.001) and scopists (3.70 vs. 3.06; p = 0.006). In contrast, for both groups, the assistant surgeons felt a lower sense of accomplishment (1.60 vs. 2.00; p = 0.098). These findings suggest that the work-related fatigue score associated with the difficulty of the LESS-A procedure may have been reduced by the feeling of accomplishment.
Discussion
Although laparoscopic surgery significantly improves patient comfort, the surgeon must operate in a completely different biomechanical environment, one that is much more demanding than the one for open surgery. Well-known difficulties include the limited freedom of movement and the lack of tactile feedback [18]. A surgeon performing a laparoscopic procedure usually stands and maintains a fixed head and neck position, which places more strain on the upper body muscles. Despite the growing use of laparoscopic surgery for a range of treatments, little has been done to improve the surgeon’s working environment and reduce the physical stresses and strains. Although ergonomics has been addressed for many occupations, priority has not been given to the changes needed to reduce the stress of the laparoscopic environment.
Many laparoscopic techniques have been developed to reduce the size and number of ports placed during minimally invasive operations in response to the demand for MIS. LESS surgery has been performed for various urological diseases, and studies have shown that there is less postoperative pain, recovery is faster, hospital stays are shorter, and cosmetic outcomes especially are better compared with conventional approaches [8]. Much effort has been made to further reduce the invasiveness of laparoscopic surgery, but an incision is ultimately needed to extract the specimen [19]. A common target in LESS surgery is the adrenal gland as it is relatively small, and laparoscopic adrenalectomy has become a common procedure. LESS surgery remains a difficult procedure, especially with the transumbilical approach, because incomplete triangulation and more complex movements of the articulating instruments limit effective dissection [20]. Therefore, the LESS procedure may impose a greater physical workload on the surgeon. To our knowledge, this is the first study to compare the feelings of fatigue between LESS-A and CLA procedures for each of the three main roles in laparoscopic surgery (chief surgeon, scopist, assistant surgeon).
Several ergonomic studies have revealed that surgeons face multiple restrictions during laparoscopic surgery that are directly related to risk factors for exacerbating musculoskeletal disorders (MSDs) [21]. Additional studies found that the percentage of MSD prevalence is as high as 87–88% among chief surgeons who perform MIS [22, 23]. These numbers are excessively high compared with those for the general population. Laparoscopic surgeons mainly complain of pain or dullness in their neck, back, shoulders, wrists, and thumbs. Symptoms associated with these disorders mainly include fatigue, pain, stiffness, and numbness. Such symptoms may affect surgical outcomes [24] and may indirectly affect patient safety, which is a major surgical priority.
Despite reports of the physical burden of laparoscopic surgery [25], there has been barely any reduction in the physical workload imposed on the surgeon. This may be because a laparoscopic approach is generally preferred by patients [26]. It is commonly believed that the physical workload is “part of the job” for surgeons and must be tolerated. Several studies have found that surgeons believe that the injury or pain they suffer may negatively affect surgical outcomes [27, 28] and that their physical complaints might affect their choice of surgical approach [5]. In fact, one report has shown that, although LESS surgery is often requested by patients, surgeons may not select this approach because of its technical difficulties [7, 9]. Therefore, the number of LESS procedures has not increased to meet demand.
Mental fatigue is a psychobiological condition caused by prolonged severe stress [29] and is ubiquitous in clinical practice. However, this condition is difficult to define, and there is no standardized way to assess mental fatigue in an objective manner. Cognitive function during extremely stressful work in life and death situations is particularly important and can be affected by mental fatigue. In this study, the feeling of instability was considered to reflect the feeling of mental fatigue, and the scores for the chief surgeon and scopists were equivalent between groups. The feeling of drowsiness and uneasiness was also considered to reflect the feeling of mental fatigue. The scores for drowsiness before and after surgery were significantly higher for the CLA group for the scopists, and the scores for uneasiness before and after surgery were significantly higher for the CLA group for the chief surgeon and scopists. In addition, the feelings of physical fatigue were almost the same between groups. The sense of accomplishment after surgery was significantly higher for the LESS-A group than for the CLA group. This suggests that the positive effect of a higher sense of accomplishment may have reduced the feelings of both mental and physical fatigue for the chief surgeon.
Ocular symptoms, such as eyestrain, accommodative difficulties, dry eye, and visual discomfort not only cause the surgeon to feel uncomfortable during laparoscopic surgery [30, 31] but also have subtle effects on the surgeon’s visual functions and thus require more attention. Decreased depth perception and spatial orientation due to the lack of natural binocular vision on a 2D display also cause emergent pain and muscular fatigue [32]. In this study, the degree of the feeling of eyestrain for the scopists was higher for the LESS-A group than for the CLA group. This is attributed to image blurring caused by using an articulating scope in the LESS-A procedures to avoid internal and external collisions (an articulating scope was used in the LESS-A procedures, and a rigid one was used in the CLA procedures).
Our study has six specific limitations. First, the sample size was very small. Second, evaluation was performed using only subjective measurement, not objective measurement. That is, we did not perform ergonomic measurements to assess the objective factors related to the feelings of fatigue. Ergonomic measurements would be helpful as they would provide data that could be correlated with the results. Third, the “Jikaku-sho shirabe” questionnaire used to collect the data is used only in Japan and has not been validated in other countries, cultures, and practice situations. Fourth, this study would benefit by having more data as the reporting instrument is based on subjective “feelings” of fatigue. There would be a benefit to collecting data on sleep hours, nutritional intake prior to surgery, and the time when surgery was performed. We did not collect data on these factors and did not consider the effect of these factors on the feelings of fatigue. Fifth, this study was performed over a long period (nearly 7 years). Our comparison of the feelings of fatigue between the two sub-periods for each procedure showed that, for the LESS-A group, the scores for the feeling of local pain or dullness were significantly higher for the second sub-period. This indicates that aging by the chief surgeon may have aggravated the score for the feeling of local pain or dullness. Sixth, randomized trials are needed to compare fatigue scores before and after surgery.
LESS-A is commonly thought to be a technically difficult procedure, and we had the same belief. However, our results revealed that for each of the three main roles in laparoscopic surgery, physical fatigue such as the feeling of local pain or dullness was roughly equal between the LESS-A and CLA groups. Although LESS-A has been reported to result in better cosmetic outcomes, the number of LESS-A procedures being performed is actually stagnant. Despite the technical difficulties of LESS-A, the actual feelings of fatigue were equivalent to those for CLA. Since LESS-A is generally preferred by patients, efforts should be made to educate surgeons about the actual physical effects of performing LESS-A so that patient demands can be met.
Conclusion
This study addressed the assumption that LESS-A is a technically difficult procedure by comparing the feelings of fatigue between LESS-A and CLA procedures for each of the key members of the surgical team before and after surgery. The results showed that physical fatigue such as local pain or dullness was basically the same for each member between the two procedures. This means that surgeons should not be constrained by concerns about feelings of fatigue and select LESS-A more often in consideration of patients’ demands.
References
Braga M, Vignali A, Gianotti L et al (2002) Laparoscopic versus open colorectal surgery: a randomized trial on short-term outcome. Ann Surg 236(6):759–767
Gervaz P, Inan I, Perneger T et al (2010) A prospective, randomized, single-blind comparison of laparoscopic versus open sigmoid colectomy for diverticulitis. Ann Surg 252(1):3–8
Veldkamp R, Kuhry E, Hop WC et al (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477–484
Lal SK, Craig A (2002) Driver fatigue: electroencephalography and psychological assessment. Psychophysiology 39(3):313–321
Bagrodia A, Raman JD (2009) Ergonomics considerations of radical prostatectomy: physician perspective of open, laparoscopic, and robot-assisted techniques. J Endourol 23(4):627–633
Sodergren MH, Aslanyan A, McGregor CG et al (2014) Pain, well-being, body image and cosmesis: a comparison of single-port and four-port laparoscopic cholecystectomy. Minim Invasive Ther Allied Technol 23(4):223–229
Inoue S, Hayashi T, Hieda K et al (2019) Longitudinal analysis of laparoendoscopic single-site adrenalectomy and conventional laparoscopic adrenalectomy regarding patient-reported satisfaction and cosmesis outcomes. Asian J Surg 42(3):514–519
Kaouk JH, Autorino R, Kim FJ et al (2011) Laparoendoscopic single-site surgery in urology: worldwide multi-institutional analysis of 1076 cases. Eur Urol 60(5):998–1005
Inoue S, Kajiwara M, Teishima J et al (2015) Population perception of surgical approach in minimally invasive surgery. Can Urol Assoc J 9(1–2):E1-4
Inoue S, Ikeda K, Kajiwara M et al (2014) Laparoendoscopic single-site adrenalectomy sans transumbilical approach: initial experience in Japan. Urol J 11(4):1772–1776
Inoue S, Kajiwara M, Teishima J et al (2016) Needlescopic-assisted laparoendoscopic single-site adrenalectomy. Asian J Surg 39(1):6–11
Sasaki T, Matsumoto S (2005) Actual conditions of work, fatigue and sleep in non-employed, home-based female information technology workers with preschool children. Ind Health 43(1):142–150
Sanchez JA, Ikaga T, Sanchez SV (2018) Quantitative improvement in workplace performance through biophilic design: A pilot experiment case study. Energy Build 177:316–328
Kubo T, Takahashi M, Sato T et al (2011) Weekend sleep intervention for workers with habitually short sleep periods. Scand J Work Environ Health 37(5):418–426
Kagamiyama H, Yana R (2018) Relationship between subjective fatigue, physical activity, and sleep indices in nurses working 16-hour night shifts in a rotating two-shift system. J Rural Med 13(1):26–32
Nagai M, Morikawa Y, Kitaoka K et al (2011) Effects of fatigue on immune function in nurses performing shift work. J Occup Health 53(5):312–319
Okamura C, Kojima T, Tokiwa S, et al. (2020) Microscopic ophthalmic surgery using freely movable arm support robot: basic experiment and clinical experience. Ophthalmic Res [Online ahead of print]
Vettoretto N, Foglia E, Ferrario L et al (2018) Why laparoscopists may opt for three-dimensional view: a summary of the full HTA report on 3D versus 2D laparoscopy by S.I.C.E. (Società Italiana di Chirurgia Endoscopica e Nuove Tecnologie). Surg Endosc 32(6):2986–2993
Cindolo L, Gidaro S, Neri F et al (2010) Assessing feasibility and safety of laparoendoscopic single-site surgery adrenalectomy: initial experience. J Endourol 24(6):977–980
Ju SH, Lee DG, Lee JH et al (2011) Laparoendoscopic single-site pyeloplasty using additional 2-mm instruments: a comparison with conventional laparoscopic pyeloplasty. Korean J Urol 52(9):616–621
Wauben LS, van Veelen MA, Gossot D et al (2006) Application of ergonomic guidelines during minimally invasive surgery: a questionnaire survey of 284 surgeons. Surg Endosc 20(8):1268–1274
Franasiak J, Ko EM, Kidd J et al (2012) Physical strain and urgent need for ergonomic training among gynecologic oncologists who perform minimally invasive surgery. Gynecol Oncol 126(3):437–442
Park A, Lee G, Seagull FJ et al (2010) Patients benefit while surgeons suffer: an impending epidemic. J Am Coll Surg 210(3):306–313
Huysmans MA, Hoozemans MJ, van der Beek AJ et al (2010) Position sense acuity of the upper extremity and tracking performance in subjects with non-specific neck and upper extremity pain and healthy controls. J Rehabilit Med 42(9):876–883
Hemal AK, Srinivas M, Charles AR (2001) Ergonomic problems associated with laparoscopy. J Endourol 15(5):499–503
Kolfschoten NE, van Leersum NJ, Gooiker GA et al (2013) Successful and safe introduction of laparoscopic colorectal cancer surgery in Dutch hospitals. Ann Surg 257(5):916–921
Ruitenburg MM, Frings-Dresen MH, Sluiter JK (2013) Physical job demands and related health complaints among surgeons. Int Arch Occup Environ Health 86(3):271–279
Esposito C, Najmaldin A, Schier F et al (2014) (2014) Work-related upper limb musculoskeletal disorders in pediatric minimally invasive surgery: a multicentric survey comparing laparoscopic and sils ergonomy. Pediatr Surg Int 30:395–399
Marcora SM, Staiano W (1985) Manning V (2009) Mental fatigue impairs physical performance in humans. J Appl Physiol 106(3):857–864
Hanna GB, Shimi SM, Cuschieri A (1998) Randomised study of influence of two-dimensional versus three-dimensional imaging on performance of laparoscopic cholecystectomy. Lancet 351(9098):248–251
Nam KW, Park J, Kim IY et al (2012) Application of stereo-imaging technology to medical field. Healthc Inform Res 18(3):158–163
Sinha RY, Raje SR, Rao GA (2017) Three-dimensional laparoscopy: Principles and practice. J Minim Access Surg 13(3):165–169
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Inoue, S., Ikeda, K., Goto, K. et al. Comparison of Chief Surgeons’ and Assistants’ Feelings of Fatigue Between Laparoendoscopic Single-site and Conventional Laparoscopic Adrenalectomy. World J Surg 45, 1466–1474 (2021). https://doi.org/10.1007/s00268-021-05962-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-05962-3