Abstract
Background
Indeterminate fine-needle aspiration cytology (FNAC) imposes challenges in the management of thyroid nodules. This study aimed to examine whether preoperative anti-thyroid antibodies (Abs) and TSH are indicators of thyroid malignancy and aggressive behavior in patients with indeterminate FNAC.
Methods
This was a retrospective study of thyroidectomy patients from 2008 to 2016. We analyzed Abs and TSH levels, FNAC, and histopathology. Serum antibody levels were categorized as ‘Undetectable’, ‘In-range’ if detectable but within normal range, and ‘Elevated’ if above upper limit of normal. ‘Detectable’ levels referred to ‘In-range’ and ‘Elevated’ combined.
Results
There were 531 patients included. Of 402 patients with preoperative FNAC, 104 (25.9%) had indeterminate cytology (Bethesda III–V). Of these, 39 (37.5%) were malignant and 65 (62.5%) benign on histopathology. In the setting of indeterminate FNAC, an increased risk of malignancy was associated with ‘Elevated’ thyroglobulin antibodies (TgAb) (OR 7.25, 95% CI 1.13–77.15, P = 0.01) and ‘Elevated’ thyroid peroxidase antibodies (TPOAb) (OR 6.79, 95% CI 1.23–45.88, P = 0.008). Similarly, while still ‘In-range’, TSH ≥ 1 mIU/L was associated with an increased risk of malignancy (OR 3.23, 95% CI 1.14–9.33, P = 0.01). In all patients with malignancy, the mean tumor size was 8 mm larger in those with TSH ≥ 1 mIU/L (P = 0.03); furthermore, in PTC patients, ‘Detectable’ TgAb conferred a 4 × risk of lymph node metastasis (95% CI 1.03–13.77, P = 0.02).
Conclusion
In this cohort, in indeterminate FNAC patients, Abs and TSH were associated with an increased risk of malignancy. Additionally, TgAb and TSH were potential markers of aggressive biology. As such, they may be diagnostic and prognostic adjuncts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid nodules are common with a prevalence of up to 70% in the general population [1]. Approximately 15–30% of biopsied nodules are characterized as indeterminate, namely Bethesda III–V, with an estimated risk of malignancy of 5–75% [2,3,4]. Patients with indeterminate nodules may need to undergo diagnostic hemithyroidectomy, repeat FNAC or molecular testing depending on other clinical and imaging considerations, but none of these options is ideal. A diagnostic hemithyroidectomy can be a procedure of compromise because it is either unnecessary in the absence of other indications if the nodule is proven to be benign, or inadequate and requiring completion thyroidectomy if the nodule is shown to be malignant [5]. Schneider et al. [6] have reported that nearly 30% of patients with indeterminate nodules received inappropriate extent of initial thyroidectomy (under- or over-treatment). Similarly, the efficacy of repeat FNAC is unclear with reportedly no change of Bethesda category in 76% of patients with indeterminate nodules following a repeat FNAC [5]. Although molecular and gene testing can play a crucial role in malignancy risk stratification, these tests are very costly and may not be accessible in resource-constrained clinical settings. In addition, patients who have papillary thyroid cancer (PTC) might also miss out on a central lymph node dissection if the malignancy is not diagnosed preoperatively.
As the management of thyroid patients continues to be refined to achieve personalized treatment plans, we conducted this present study to explore the use of routine biochemical tests such as TSH and anti-thyroid antibody measurements in augmenting the preoperative assessment.
The literature shows an association between thyroiditis and thyroid carcinoma [7, 8], and chronic inflammation is a recognized risk factor for cancer development [9]. Moreover, TSH is a widely known thyroid growth factor, and several studies have suggested that higher TSH is associated with thyroid cancer development [10,11,12].
The cancer risk stratification and surgical treatment of thyroid nodules with indeterminate cytology remain a challenge for clinicians. Hence, this study aimed to examine whether preoperative anti-thyroid antibodies and TSH are potential markers of (1) thyroid carcinoma in patients with indeterminate cytology and (2) more aggressive behavior in patients with malignancy.
Methods
This was a retrospective study of patients undergoing thyroidectomy in the Monash University Endocrine Surgery Unit (MUESU) from 2008 to 2016. All information was retrieved from the MUESU surgical database and electronic medical records, including demographic data, preoperative anti-thyroid antibody and TSH levels, FNAC results and final histopathology which comprised of cancer type, largest malignant tumor size, and lymph node metastasis. Data collection and subsequent analysis were approved by the Alfred Health Human Research Ethics Committee (Project No: 185/19).
All patients with thyroid nodules were initially assessed clinically and by ultrasonography. Subsequently, FNAC was performed on those who had nodules with suspicious features based on the American Thyroid Association (ATA) guidelines [2], and where clinically indicated. FNAC was performed under ultrasound guidance, and cytology was reported by an endocrine cytopathologist. Indeterminate FNAC was defined as per Bethesda criteria, including Bethesda III (atypia of undetermined significance or follicular lesion of unknown significance), Bethesda IV (follicular neoplasm or suspicious for follicular neoplasm), and Bethesda V (suspicious for malignancy) [4].
Serum marker levels were categorized into three—‘Undetectable’ if below the lower limit of detection, ‘In-range’ if detectable and within the assay’s reference range, and ‘Elevated’ if above the upper limit of the reference range. In addition, in this study, the term ‘Detectable’ refers to ‘In-range’ and ‘Elevated’ combined. TSH levels were considered to be ‘In-range’ if they were within the specific laboratory normal range.
The presence of elevated anti-thyroid antibodies was correlated with the presence of thyroiditis on histopathology of the resected specimen, regardless of whether a malignancy was present.
Focusing on the patients with indeterminate cytology, we then correlated the presence of elevated anti-thyroid antibodies and TSH level to the risk of malignancy. The rates of malignancy in patients with and without either elevated TPOAb or TgAb were compared. Patients were then grouped into four groups according to TSH level (0–0.49, 0.5–0.99, 1.0–1.49, 1.5, and above) and the risk of malignancy calculated.
In this study, the features that defined aggressive behavior were tumor size and presence of lymph node metastasis. The mean cancer sizes were compared in patients with TSH below or above 1 mIU/L. The rates of lymph node metastasis were compared between patients with and without detectable TPOAb and TgAb.
Binary variables were analyzed using Pearson’s Chi-square test, and continuous variables were analyzed using Student’s t test. A P value less than 0.05 was considered statistically significant. Statistical analysis was performed using Stata software version 15.1 (StataCorp, Texas, USA).
Results
Clinical characteristics
During the 9-year study period from 2008 to 2016, 2045 patients had thyroid surgery and were eligible for the study. Of these, 531 patients were included for analysis, after excluding 1514 that did not have preoperative measurements of serum anti-thyroid antibodies or TSH, cytology, or histopathology reports. The mean age was 52 ± 17 (SD) years (range 15–89). There was a female preponderance—416 females (78.3%) and 115 males (21.7%) with a female-to-male ratio of approximately 4:1 (Table 1).
Of the 402 patients with preoperative cytology, 104 (25.9%) had indeterminate cytology (91, 87.5% Bethesda III or IV, and 13, 12.5% Bethesda V). The four most common primary indications for surgery for all patients in the study cohort were risk of malignancy (29.4%), pressure symptoms (26.2%), thyrotoxicosis (22.0%), and preoperative diagnosis of malignancy (15.1%) (Table 2). A high proportion of patients in the study cohort (319, 60%) had a total thyroidectomy, while 179 (33.7%) patients had hemithyroidectomy, and 33 (6.2%) patients had other types of thyroidectomy (e.g., isthmus resection, re-operative surgery). In contrast, the majority of patients with indeterminate cytology (63, 60.6%) had hemithyroidectomy.
Of the 151 patients with histopathologically confirmed thyroid cancer, the majority had PTC. This was followed by minimally invasive follicular thyroid cancer, follicular thyroid cancer, medullary thyroid cancer, and poorly differentiated thyroid cancer, in descending order (Table 3).
Anti-thyroid antibodies and thyroiditis on histopathology
The prevalence of elevated TPOAb and TgAb were 31.2% and 17.1% respectively. There were 114 (21.9%) patients with thyroiditis on final histopathology. There was a strong association between elevated anti-thyroid antibodies (TgAb and/or TPOAb) and thyroiditis on histology (OR 17.44, 95% CI 7.86–41.21, P < 0.0001). However, thyroiditis was sometimes seen on histopathology in the absence of elevated antibodies, and vice versa.
Anti-thyroid antibodies and risk of malignancy in the context of indeterminate cytology
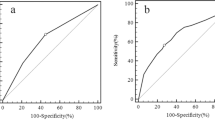
Of 104 patients with indeterminate cytology, 10 (18.9%) had elevated TPOAb and 9 (17.3%) had elevated TgAb. Among these patients with indeterminate cytology, 39 (37.5%) had a thyroid carcinoma, and 65 (62.5%) had a benign thyroid nodule on the final histopathologic examination. In this group, elevated TgAb (OR 7.25, 95% CI 1.13–77.15, P = 0.01) and elevated TPOAb (OR 6.79, 95% CI 1.23–45.88, P = 0.008) were found to be significantly associated with an increased risk of thyroid malignancy (Fig. 1).
TSH and risk of malignancy in the context of indeterminate cytology
When patients with indeterminate cytology were subdivided into four groups according to TSH levels, a correlation between TSH level and risk of malignancy with a substantial increase at the TSH value of 1 mIU/L emerged (Fig. 2). As TSH increased, the prevalence of malignancy on final histopathology also increased. Further, 49% of the patients with TSH ≥ 1 mIU/L were diagnosed with malignancy, which was over twice more frequently than those with TSH < 1 mIU/L, who had a frequency of 23% (OR 3.23, 95% CI 1.14–9.33, P = 0.01). Notably, in this cohort of patients with indeterminate cytology, three patients were on thyroxine to achieve a TSH in the normal range; however, all of them were excluded to avoid any confounding effect.
Synergistic association among markers
In patients with indeterminate cytology, the presence of either an elevated anti-thyroid antibody or TSH ≥ 1 mIU/L was associated with significant increased risk of thyroid cancer (OR 3.40, 95% CI 1.21–9.91, P = 0.009), and the presence of both an elevated anti-thyroid antibody and TSH ≥ 1 mIU/L was associated with an even greater risk of thyroid carcinoma, compared to patients with neither of the markers (OR 10.67, 95% CI 1.48–118.11, P = 0.003) (Fig. 3). Therefore, the risk of malignancy increased as the number of markers increased with the highest risk of malignancy being associated with having two markers. It should be recognized that the number of patients with both markers was small (N = 8), despite a significant P value.
TSH/TgAb and aggressive behavior
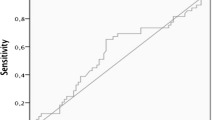
TSH and TgAb were found to be associated with more aggressive tumor biology as defined by primary tumor size and presence of lymph node metastasis respectively. Among 151 patients with histologically confirmed malignancy, the mean tumor size was 26 ± 20 (SD) mm in those with TSH ≥ 1 mIU/L, and 18 ± 17 (SD) mm in those with TSH < 1 mIU/L (P = 0.03) (Fig. 4a). Of the 119 patients with PTC, 32 (26.9%) had lymph node metastasis confirmed on histopathology. In patients with detectable TgAb, 50% had lymph node metastasis, whereas in patients with undetectable TgAb, 21% had lymph node metastasis (OR 3.78, 95% CI 1.03–13.77, P = 0.02) (Fig. 4b). In spite of a significant P value, it is worth noting that only three patients had both detectable TgAb and lymph node metastasis. No significant association between TPOAb and lymph node metastasis was seen. Likewise, no association was seen between the serum markers and subtype of malignancy.
Discussion
This study demonstrated that elevated anti-thyroid antibodies and TSH ≥ 1 mIU/L were independently and synergistically associated with an increased risk of thyroid carcinoma in patients with indeterminate cytology. Additionally, TSH ≥ 1 mIU/L was associated with larger primary tumor size, and detectable TgAb was associated with presence of lymph node metastasis, both suggestive of more aggressive tumor biology.
The association between anti-thyroid antibodies and thyroid cancer is controversial. In line with several previous studies, our data have demonstrated that autoimmune thyroiditis is associated with an increased risk of thyroid carcinoma [8, 13,14,15,16,17,18], while others have proposed that the coexistence of thyroiditis in patients with thyroid nodules confers no additional risk of malignancy [19,20,21,22]. Cytological series tend to find no significant association between autoimmune thyroiditis and thyroid carcinoma arguing that the association proposed by histology-based surgical series is a result of a selection bias reportedly due to the fact that patients undergoing thyroidectomy are more likely to have suspicious nodules; however, these studies are limited by a lack of definitive histopathological diagnosis.
The literature suggests that inflammation is essential for the development of most, if not all, tumors because it plays an important role in both cancer initiation and progression [23]. Chronic inflammation can promote a tumorigenic microenvironment by inhibiting apoptosis and stimulating increased cell proliferation, angiogenesis, and release of various mutagenic cytokines and free radicals [24,25,26]. Even though the exact mechanism remains unclear, a potential molecular mechanism for thyroid carcinogenesis involves PI3K/Akt pathway and RAS/RET/ERK pathway which are triggered in both thyroid carcinoma and Hashimoto's thyroiditis [27, 28]. Similarly, immunohistological markers of PTC, such as p63 [29] and cytokeratin 19 [30], can also be found in tissues with autoimmune thyroiditis.
Lymph node metastasis is a marker of tumor aggressiveness. We found that detectable TgAb was associated with approximately fourfold increased risk of lymph node metastasis in patients with PTC which was consistent with the study by Vasileiadis et al. who proposed a similar correlation between TgAb positivity and lymph node metastasis in PTC patients [31]. A potential confounder is that patients with thyroiditis would be more likely to have incidental lymph nodes resected at surgery, hence increasing the chance of detection of incidental microscopic metastasis in patients with positive antibodies. Conversely, while acknowledging the tumorigenic action of thyroiditis, a number of other studies have suggested that thyroiditis may have a protective effect in the long term with respect to recurrence and overall prognosis [32, 33]. Molecular rationales proposed for this phenomenon include anti-tumorigenic activity of IL-1 [34] and enhanced destruction of cancer cells expressing thyroid-specific antigens as a result of previous autoimmune reaction to thyroid-specific antigens [35, 36]. Notably however, Singh et al. have argued that patients with Hashimoto’s thyroiditis are more likely to have other protective factors such as younger age, so controversies exist [37].
Even within normal range, TSH is associated with an increased risk of thyroid carcinoma and advanced TNM stage [10,11,12, 16, 38,39,40,41]. Interestingly, in these studies, TSH of 1 mIU/L seems to have emerged as the threshold above which the risk of malignancy increases. Furthermore, pathological thyroid growth can be seen in Graves’ disease (through thyroid stimulatory antibodies) and TSH-secreting pituitary adenomas where chronic stimulation of TSH receptor leads to persistent hyperplasia [42, 43]. In our study, the mean malignant tumor size was found to be approximately 8 mm larger in those with TSH ≥ 1 mIU/L. The fact that the expression and responsiveness of TSH receptors remain moderately unaffected in differentiated thyroid cancer [38, 44,45,46] is also why levothyroxine-induced suppression of TSH is effective in tumor growth inhibition as an adjuvant therapy [47].
A key strength of this study was that we specifically focused on the utility of anti-thyroid antibodies and TSH in patients with indeterminate FNAC, as most published studies have reported the role of these markers in all patients with thyroid nodules. Additionally, of patients with indeterminate cytology, the majority (87.5%) had nodules with Bethesda III or IV classification with a small proportion (12.5%) who had nodules with Bethesda V classification. This reduces the risk of the findings being due to selection bias from a high proportion of Bethesda V cases with a high rate of malignancy. Moreover, to the best of our knowledge, this is the first study to explore the synergistic effect of TSH and anti-thyroid antibodies in increasing the risk of malignancy in patients with indeterminate cytology.
The limitations of this study included its retrospective design, and that we only had a static measure of anti-thyroid antibodies and TSH. Serial measurement of these markers to assess the period of elevated antibodies and TSH might have shed further insight. Despite a study period of 9 years, our study had a relatively small sample size by virtue of focusing on the patients with indeterminate cytology. This limited the statistical power of subgroup analysis. Longitudinal multicenter, prospective studies with larger number of patients with indeterminate cytology may be able to validate the potential role of these markers in determining the risk of malignancy, by allowing more standardized testing of serum markers.
In conclusion, in this cohort of patients, anti-thyroid antibodies and TSH were markers of thyroid carcinoma and aggressive behavior in the setting of indeterminate cytology. As such, in the absence of molecular testing which is not widely accessible outside of the USA, preoperative anti-thyroid antibodies and TSH may be additional diagnostic and prognostic adjuncts in the workup of patients with indeterminate nodules, aiding decision-making for the extent of surgery, and helping to achieve the practice of personalized medicine, and to avoid over- and under-treatment.
References
Parsa AA, Gharib H (2018) Chapter 1, Epidemiology of thyroid nodules. In: Gharib H (ed) Thyroid nodules - diagnosis and management. Humana Press, Cham, p 7
Haugen BR, Alexander EK, Bible KC et al (2016) 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26(1):1–133
Keutgen XM, Filicori F, Fahey TJ (2013) Molecular diagnosis for indeterminate thyroid nodules on fine needle aspiration: advances and limitations. Expert Rev Mol Diagn 13(6):613–623
Cibas ES, Ali SZ (2009) The Bethesda system for reporting thyroid cytopathology. Am J Clin Pathol 132(5):658–665
Jooya A, Saliba J, Blackburn A et al (2016) The role of repeat fine needle aspiration in the management of indeterminate thyroid nodules. J Otolaryngol Head Neck Surg 45(1):51
Schneider DF, Cherney Stafford LM, Brys N et al (2017) Gauging the extent of thyroidectomy for indeterminate thyroid nodules: an oncologic perspective. Endocr Pract 23(4):442–450
Uhliarova B, Hajtman A (2018) Hashimoto's thyroiditis: an independent risk factor for papillary carcinoma. Braz J Otorhinolaryngol 84(6):729–735
Seifman MA, Grodski SF, Bailey M et al (2011) Surgery in the setting of Hashimoto's thyroiditis. ANZ J Surg 81(7–8):519–523
Korniluk A, Koper O, Kemona H et al (2017) From inflammation to cancer. Ir J Med Sci 186(1):57–62
Besler E, Citgez B, Aygun N et al (2019) The relationship of clinicopathological factors of the tumor with preoperative TSH level in papillary thyroid cancers. Eurasian J Med 51(1):8–11
Hu N, Li ZM, Liu JF et al (2016) An overall and dose-response meta-analysis for thyrotropin and thyroid cancer risk by histological type. Oncotarget 7(30):47750–47759
Haymart MR, Repplinger DJ, Leverson GE et al (2008) Higher serum thyroid stimulating hormone level in thyroid nodule patients is associated with greater risks of differentiated thyroid cancer and advanced tumor stage. J Clin Endocrinol Metab 93(3):809–814
Kim KW, Park YJ, Kim EH et al (2011) Elevated risk of papillary thyroid cancer in Korean patients with Hashimoto's thyroiditis. Head Neck 33(5):691–695
Muzza M, Degl'Innocenti D, Colombo C et al (2010) The tight relationship between papillary thyroid cancer, autoimmunity and inflammation: clinical and molecular studies. Clin Endocrinol (Oxf) 72(5):702–708
Hosseini S, Payne RJ, Zawawi F et al (2016) Can preoperative thyroglobulin antibody levels be used as a marker for well differentiated thyroid cancer? J Otolaryngol Head Neck Surg 45(1):31
Azizi G, Keller JM, Lewis M et al (2014) Association of Hashimoto's thyroiditis with thyroid cancer. Endocr Relat Cancer 21(6):845–852
Repplinger D, Bargren A, Zhang YW et al (2008) Is Hashimoto's thyroiditis a risk factor for papillary thyroid cancer? J Surg Res 150(1):49–52
Zhang Y, Dai J, Wu T et al (2014) The study of the coexistence of Hashimoto's thyroiditis with papillary thyroid carcinoma. J Cancer Res Clin Oncol 140(6):1021–1026
Anil C, Goksel S, Gursoy A (2010) Hashimoto's thyroiditis is not associated with increased risk of thyroid cancer in patients with thyroid nodules: a single-center prospective study. Thyroid 20(6):601–606
Matesa-Anic D, Matesa N, Dabelic N et al (2009) Coexistence of papillary carcinoma and Hashimoto's thyroiditis. Acta Clin Croat 48(1):9–12
Castagna MG, Belardini V, Memmo S et al (2014) Nodules in autoimmune thyroiditis are associated with increased risk of thyroid cancer in surgical series but not in cytological series: evidence for selection bias. J Clin Endocrinol Metab 99(9):3193–3198
Selek A, Cetinarslan B, Tarkun I et al (2017) Thyroid autoimmunity: is really associated with papillary thyroid carcinoma? Eur Arch Otorhinolaryngol 274(3):1677–1681
Mantovani A, Allavena P, Sica A et al (2008) Cancer-related inflammation. Nature 454(7203):436–444
Allavena P, Garlanda C, Borrello MG et al (2008) Pathways connecting inflammation and cancer. Curr Opin Genet Dev 18(1):3–10
Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420(6917):860–867
Guarino V, Castellone MD, Avilla E et al (2010) Thyroid cancer and inflammation. Mol Cell Endocrinol 321(1):94–102
Larson SD, Jackson LN, Riall TS et al (2007) Increased incidence of well-differentiated thyroid cancer associated with Hashimoto thyroiditis and the role of the PI3k/Akt pathway. J Am Coll Surg 204(5):764–773 (discussion 73–5)
Kang DY, Kim KH, Kim JM et al (2007) High prevalence of RET, RAS, and ERK expression in Hashimoto's thyroiditis and in papillary thyroid carcinoma in the Korean population. Thyroid 17(11):1031–1038
Unger P, Ewart M, Wang BY et al (2003) Expression of p63 in papillary thyroid carcinoma and in Hashimoto's thyroiditis: a pathobiologic link? Hum Pathol 34(8):764–769
Arif S, Blanes A, Diaz-Cano SJ (2002) Hashimoto's thyroiditis shares features with early papillary thyroid carcinoma. Histopathology 41(4):357–362
Vasileiadis I, Boutzios G, Charitoudis G et al (2014) Thyroglobulin antibodies could be a potential predictive marker for papillary thyroid carcinoma. Ann Surg Oncol 21(8):2725–2732
Ahn D, Heo SJ, Park JH et al (2011) Clinical relationship between Hashimoto's thyroiditis and papillary thyroid cancer. Acta Oncol 50(8):1228–1234
Song E, Oh HS, Jeon MJ et al (2019) The value of preoperative antithyroidperoxidase antibody as a novel predictor of recurrence in papillary thyroid carcinoma. Int J Cancer 144(6):1414–1420
Kimura H, Yamashita S, Namba H et al (1992) Interleukin-1 inhibits human thyroid carcinoma cell growth. J Clin Endocrinol Metab 75(2):596–602
Cunha LL, Morari EC, Guihen AC et al (2012) Infiltration of a mixture of immune cells may be related to good prognosis in patients with differentiated thyroid carcinoma. Clin Endocrinol (Oxf) 77(6):918–925
Lucas SD, Karlsson-Parra A, Nilsson B et al (1996) Tumor-specific deposition of immunoglobulin G and complement in papillary thyroid carcinoma. Hum Pathol 27(12):1329–1335
Singh B, Shaha AR, Trivedi H et al (1999) Coexistent Hashimoto's thyroiditis with papillary thyroid carcinoma: impact on presentation, management, and outcome. Surgery 126(6):1070–1077
Rowe CW, Paul JW, Gedye C et al (2017) Targeting the TSH receptor in thyroid cancer. Endocr Relat Cancer 24(6):R191–R202
Boelaert K, Horacek J, Holder RL et al (2006) Serum thyrotropin concentration as a novel predictor of malignancy in thyroid nodules investigated by fine-needle aspiration. J Clin Endocrinol Metab 91(11):4295–4301
Golbert L, de Cristo AP, Faccin CS et al (2017) Serum TSH levels as a predictor of malignancy in thyroid nodules: a prospective study. PLoS ONE 12(11):e0188123
Boi F, Minerba L, Lai ML et al (2013) Both thyroid autoimmunity and increased serum TSH are independent risk factors for malignancy in patients with thyroid nodules. J Endocrinol Invest 36(5):313–320
Hegedus L, Hansen JM, Karstrup S (1983) High-incidence of normal thyroid-gland volume in patients with Graves-disease. Clin Endocrinol (Oxf) 19(5):603–607
Beck-Peccoz P, Persani L, Mannavola D et al (2009) Pituitary tumours: TSH-secreting adenomas. Best Pract Res Clin Endocrinol Metab 23(5):597–606
Kim D, Park JW (2013) Clinical implications of preoperative thyrotropin serum concentrations in patients who underwent thyroidectomy for nonfunctioning nodule(s). J Korean Surg Soc 85(1):15–19
Carayon P, Thomas-Morvan C, Castanas E et al (1980) Human thyroid cancer: membrane thyrotropin binding and adenylate cyclase activity. J Clin Endocrinol Metab 51(4):915–920
Abe Y, Ichikawa Y, Muraki T et al (1981) Thyrotropin (TSH) receptor and adenylate cyclase activity in human thyroid tumors: absence of high affinity receptor and loss of TSH responsiveness in undifferentiated thyroid carcinoma. J Clin Endocrinol Metab 52(1):23–28
McGriff NJ, Csako G, Gourgiotis L et al (2002) Effects of thyroid hormone suppression therapy on aciverse clinical outcomes in thyroia cancer. Ann Med 34(7–8):554–564
Acknowledgements
We would like to acknowledge all the surgeons who have contributed cases to the Monash University Endocrine Surgery Unit (MUESU) database.
Funding
No grants or funding received for this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Study approved by Alfred Health Human Research Ethics Committee (Project No: 185/19).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Adhami, M., Michail, P., Rao, A. et al. Anti-Thyroid Antibodies and TSH as Potential Markers of Thyroid Carcinoma and Aggressive Behavior in Patients with Indeterminate Fine-Needle Aspiration Cytology. World J Surg 44, 363–370 (2020). https://doi.org/10.1007/s00268-019-05153-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05153-1