Abstract
Objective
The aim of this study was to evaluate the outcomes of video-assisted thoracic surgery (VATS) for mediastinal bronchogenic cyst (MBC) excision and investigate the surgical indication for MBC.
Methods
We retrospectively reviewed all consecutive MBC patients who underwent surgical excision between April 2001 and June 2016. One hundred and nineteen patients were enrolled with a median age of 45.4 years and divided into two groups: anterior mediastinum group (n = 48), and middle and posterior mediastinum group (n = 71). VATS technique was initially performed for each patient. The cyst should be resected completely as far as possible. Follow-up was completed by telephone or outpatient clinic every year. The deadline of follow-up was June 2017.
Results
One hundred and eighteen patients underwent VATS, and only one patient converted to open thoracotomy. The average operative time was 103.8 ± 41.6 min (40–360 min). The average intraoperative blood loss was 56.6 ± 86.6 ml (5–600 ml). The intraoperative complication rate was 3.4%, and the incomplete excision rate was 5.9%. The multivariate logistic analysis showed that maximal diameter >5 cm was significantly associated with risk of operation time extension (OR = 3.968; 95% CI 1.179–13.355, p = 0.026) and bleeding loss increasing (OR = 12.242; 95% CI 2.420–61.933, p = 0.002). No serious postoperative complications were observed. Follow-up was performed in 102 patients, and the mean follow-up time was 45 months (12–194 months). There was no local recurrence.
Conclusions
The maximal diameter >5 cm increased risk of operation time extension and bleeding loss increasing. Early surgical excision of MBC by VATS is recommended to establish histopathological diagnosis, relieve symptoms, and prevent surgery-related complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Mediastinal bronchogenic cyst (MBC) is a rare benign congenital malformation which originates from abnormal budding of the ventral foregut between the 26th and 40th days of gestation. They mostly occurred near the tracheobronchial tree in mediastinum and represent 5–10% of all mediastinal masses [1, 2]. The incidence of MBC has increased because of more advanced diagnostic methods, and regular medical examinations were performed in recent years. The MBCs are mainly revealed by radiological examination for most patients are asymptomatic. The most important treatment method for MBC is surgical excision. However, there is still controversy as to surgical indication for asymptomatic MBC patients. Although the MBCs show as benign course, early surgical excision of MBC is recommended by some surgeons because the surgery could establish histopathological diagnosis, relieve clinical symptoms, and prevent complications [3]. Video-assisted thoracic surgery (VATS) is now widely accepted as the primary therapeutic option in the management of MBC for its safety and mini-invasive. In this study, we performed a retrospective analysis over 15 years in our institution to evaluate the outcomes of VATS excision for MBC and to investigate the surgical indication and treatment strategy of MBC. To our knowledge, this is one of the largest case series of MBC treated via VATS.
Materials and methods
We retrospectively reviewed 119 consecutive patients who were diagnosed as MBCs by pathological examination following surgical excision at Peking University People’s Hospital between April 2001 and July 2016. All patients received chest X-ray and chest computerized tomography (CT) scan for preoperative diagnosis. Magnetic resonance imaging (MRI) or PET-CT could be performed when additional radiological information was needed. VATS excision was initially performed for each patient. Medical records were reviewed in detail regarding age, sex, symptom at presentation, concomitant malignancy, preoperative radiological examination report, surgical approach, extent of surgery, operation time, intraoperative bleeding, postoperative hospital stay, postoperative complication, mortality, and recurrence. Follow-up was completed by telephone or outpatient clinic annually, and the deadline of follow-up was July 2017.
Surgical techniques
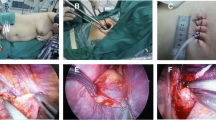
Under general anesthesia with one-lung ventilation by double lumen endotracheal incubation, VATS technique was initially performed for each MBC patient. The surgical procedures were conducted in the 30°–45° lateral recumbent position for anterior mediastinum cysts and lateral for recumbent position for middle and posterior mediastinum cysts with three- or two-port technique. The camera port was usually placed in the mid-axillary line of the 5th–7th intercostal space. Under the direct thoracoscopic vision, the operator port and assisted-operator port were selected according to the site of the cysts. The assisted-operator port might be omitted for simple cases (Fig. 1).
Our surgical principle included: (1) The cyst should be resected completely as far as possible, and the leakage of the cyst fluid should be avoided. (2) When complete excision could not be performed for serve adhesions, the residual part of the cyst should be destroyed by chemical agents or physical damage. (3) When thymoma or other malignant tumors of the thymus could not be excluded according to preoperative examination or intraoperative exploration, thymectomy should be performed for the anterior mediastinum cysts. At the end of surgery, one drainage tube was inserted in the thoracic cavity. Histologic examinations confirmed the diagnosis of MBC based on the existence of ciliated columnar epithelial lining.
Statistics analysis
Statistical Product and Service Solutions (SPSS) software version 20.0 (2011; IBM, Armonk, NY, USA) was used for statistical analysis. Differences were compared using a t test for continuous variables and Chi-square test for categorical variables. Multivariate logistic regression was used to select independent predict factors for operation time prolonged (>120 min) and blood loss increased (>100 ml). p value <0.05 was considered statistically significant.
Results
There were 56 male and 63 female patients. The median age was 45.4 years (range 4–75 years). 32 (26.9%) patients were symptomatic, 11 (9.2%) of them were asymptomatic at the first time of diagnosis by radiological examinations, but they had eventually developed symptoms during clinical observation with a median follow-up of 2 years (ranged 1–8 years). The chief complaints were cough (9.2%) and chest pain (9.2%), and other symptoms included dyspnea (5.0%), dysphagia (2.5%), fever (0.8%). Two patients had concomitant myasthenia gravis. The average size of the MBC was 3.53 ± 2.28 cm in greatest diameter (range 0.5–22.0 cm). The average CT value was 35.6 ± 14.8 Hu (range 0–67 Hu) on unenhanced CT (N = 119), and 40.4 ± 16.7 Hu (range 0–70 Hu) on contrast-enhanced CT (N = 61), respectively. 47.1% patients were diagnosed as mediastinal cyst by CT, and only 23.5% were correctly diagnosed as MBC. The patients were divided into two groups: anterior mediastinum group (N = 48), and middle and posterior mediastinum group (N = 71). The demographic characteristics of two groups are shown in Table 1. The patients in Group II were younger and had more clinical symptom, had a larger cyst and more easily diagnose as MBC, and symptom developed during observation mostly occurred in Group II. The location of MBC by Maier’s classification is shown in Table 2.
The cysts were removed by completely VATS in 118 patients, and conversion to thoracotomy was in one patient for severe adhesions to the thoracic aorta. The average operation time was 103.8 ± 41.6 min (range 40–360 min), and the average blood loss was 56.6 ± 86.6 ml (range 5–600 ml). The surgery-related complications included one patient with tracheal injury and three patients with esophageal injury, and they were repaired by the using of simple interrupted suturing with 3-0 absorbable suture material. The median chest tube indwelling time was 2.6 days (range 1–14 days), and the patients were discharged after a median of 4.5 days (range 2–21 days) postoperatively. The postoperative complications included one patient with arrhythmia, one patient with prolonged air leakage (≥7 days), two patients with pneumonia, and two patients with chylothorax. There was no significant difference of postoperative complications between the two groups (Table 3). The incomplete excision of the cyst mainly happened in Group II, and this situation was seen in seven patients because of severe adhesion to mediastinal structure, including five cases to the membranous wall of the trachea, one case to pulmonary artery and thoracic aorta, and one case to the recurrent laryngeal nerve.
Results of univariate analysis showed that the maximal diameter >5 cm and adhesion between the cyst and mediastinal structure prolonged the operation time and increased the blood loss (Table 4). All variables were analyzed by multivariate logistic analysis, and the result showed that the maximal diameter >5 cm was significantly associated with the risk of operation time extension (OR = 3.968; 95% CI 1.179–13.355, p = 0.026) and bleeding loss increasing (OR = 12.242; 95% CI 2.420–61.933, p = 0.002). Adhesions between the cyst and mediastinum could increase the risk of operation time extension (OR = 3.656; 95% CI 1.338–9.988, p = 0.011) (Table 5).
The postoperative follow-up was succeeded in 102 (85.7%) patients, and the long-term follow-up ranged from 12 to 194 months with a median follow-up of 45 months. The symptoms were all relieved among the succeeded follow-up patients (N = 28), and there were no late complications or recurrences in the 102 patients.
Discussion
MBCs are rare congenital bronchopulmonary malformation, which is thought to originate from the primitive ventral foregut in early stages [1, 2]. MBCs comprise 40–50% of all mediastinal cysts, and the incidence of MBCs has increased in recent years because more patients were detected by advanced radiographic equipment during routine medical examination [3, 4]. About 50–79% of MBC patients are symptomatic, the most common symptoms are mainly caused by the compression or stimulation of the cyst to mediastinal structure which included chest pain, cough, dysphagia, dyspnea [4,5,6], and the cyst could get an enlargement which could press the mediastinal structure severely (Fig. 2) or suffer a risk of rupture of the cyst. In addition, some studies indicated that there was a part of asymptomatic patients with MBC could ultimately become symptomatic [7].
Chest CT is the most commonly used preoperative diagnosis technique which could reveal the size and shape of the cyst, as well as the relationships between MBCs and surrounding mediastinal vital structures. The typical CT performance for MBCs included: (1) located in middle or posterior mediastinum near the tracheobronchial tree, (2) shown as cystic appearing on CT, (3) mostly manifest as round or oval, well-circumscribed, homogeneous attenuation, with thin or imperceptible walls, and (4) low-grade or no enhancement on contrast-enhanced CT scan (Fig. 3) [7, 8]. However, typical imaging performance was only seen in 10–40% patients. About 40–53% of patients were shown as soft-tissue attenuation on chest CT, and it is difficult to differentiated MBC from solid neoplasm for the cyst with high attenuation which might be caused by protein-rich cyst fluid [4, 8]. When the cyst is located in atypical position, it would be difficult to get an accurate diagnosis, such as anterior mediastinal or paraesophageal cyst which would be misdiagnosed as thymic cyst or esophageal cyst. In McAdams’ study [8], 20 patients underwent both CT and MRI, nine cysts were presented as water-like on MRI, while they were all seen as soft-tissue-like on CT, which demonstrated that MRI could provide more diagnostic information. When it is difficult to differentiated MBC from solid neoplasm, contrast-enhanced CT scan or MRI can be useful for differentiating problematic soft-tissue attenuation cysts from mediastinal neoplasia [7, 8].
Chest CT and resected specimen performance of mediastinal bronchogenic cyst. a, b Chest CT showed a cystic density mass (CT value 18 Hu) with a thin wall in carina, and the resected specimen reveals a MBC containing serous fluid. c, d Chest CT showed a solid density mass (CT value 60 Hu) in the posterior mediastinum, and the resected specimen reveals a MBC with sticky fluid
Most surgeons generally accept that the symptomatic MBC patients or those with progressive growth should receive surgical excision. However, there is still controversy in management of asymptomatic patients [9, 10]. The MBCs are benign mediastinal disease, and most of them are slow-growing. Kirmani and Sogliani [9] reviewed 23 papers which included 683 MBC patients, 74 asymptomatic patients were treated conservatively, and the longest period of observation could be 22 years; malignant transformation within the cyst could be founded in 0.7% patients. Moreover, there was no malignant transformation in our series which indicate that this situation was a fairly rare occurrence. Therefore, we think that conservative treatment could be performed for asymptomatic patients with a typical imaging performance of mediastinal cyst that could be easily differentiated from solid or malignant tumors. However, the regular follow-up by radiological examinations should not be ignored for these patients.
Kirmani and Sogliani [9] reported that about 45% of asymptomatic MBC patients could eventually develop symptoms during the observation period. In our study, 11 patients developed symptoms after detected by radiological examination with a median 2-year observation time. Some complications could develop occasionally such as infection, pneumothorax, superior vena cava obstruction, pleural effusion due to rupture of the cyst or arrhythmia caused by cardiac compression [9,10,11]. Furthermore, in Maurin’s study [12], they found that the growth of MBCs was continued even in absence of symptoms or complications. The enlargement of the cyst may lead to serve adhesion to adjacent mediastinal structures or get a secondary infection, which increases the difficulty of surgery and the risk of complications. Therefore, the surgical excision might be eventually required to relieve clinical symptoms, prevent development of symptoms or complications, confirm the histologic diagnosis, and avoid the probability of malignant transformation.
Fievet et al. [10] reported a series of 36 patients with MBCs, their finding showed that the early excision could reduce the incidence of inflammatory lesions and the rate of conversion to thoracotomy or surgical complications, and the best time to remove the cyst was between the 6th and 12th month of life. The enlargement of the cyst could become adherent to vital mediastinal structures severely which made it difficult to remove the cyst wall, especially when the cyst was adjacent to pulmonary artery/vein or membranous wall of the trachea which might lead to an incomplete excision. In our study, the multivariate logistic regression analysis showed that cysts with a maximal diameter >5 cm increase the risk of operation time extension by 3.968 times and bleeding loss increasing by 12.242 times. Therefore, we think that the surgical treatment should be performed in following situations: (1) The patients have symptom caused by MBC; (2) solid or malignant tumor cannot be excluded according to preoperative radiological examinations; (3) maximal diameter of the cyst is greater than 5 cm; (4) the cyst is located in middle or posterior mediastinum and is adjacent to the mediastinal vital structure (i.e., aorta, pulmonary artery/vein or membranous wall of the trachea).
Lewis et al. [13] performed the first VATS excision for a MBC patient in 1992. Since then, VATS has been gradually applied for the treatment of MBCs. Tölg et al. [14] compared the outcomes of MBC patients who underwent traditional thoracotomy versus VATS firstly, and indicated that VATS could decrease the chest tube duration and length of hospital stay for the strictly selected patients. Subsequently, In Jung’s study [15], VATS technique could be initially performed in 76.4% patients with MBCs. Guo’s study showed that VATS procedure decreased the operative time and intraoperative blood loss, and did not increase the risk of incomplete excision, surgery-related and postoperative complications. In the early stage, the conversion rate from VATS to open thoracotomy could be 8–35% [6, 16]. Recently, the conversion rate has declined to 1.5–3.5% with the accumulation of surgical experiences and evolvement of the thoracoscopic instruments [4, 9]. The main reason for conversion was severe adhesions and vascular injuries [5, 16]. In our series, VATS excision was initially performed for each patient without purposely selection, and adhesions around the cyst could be found in 37.8% patients. However, only one patient was converted to thoracotomy due to severe adhesions to the thoracic aorta. VATS is a safe and feasible mini-invasive therapy for MBCs, and our data also confirmed the advantages of VATS. Therefore, we think that the VATS could be the first choice of management for MBCs.
MBC is a congenital benign disorder; however, late recurrence due to incomplete excision has been reported even 25 years after surgery [17]. Thus, complete excision of the cyst wall should be performed as far as possible. Complete excision of the MBCs may be difficult due to severe adhesions to the mediastinal structure or seriously fusion between cyst and membranous wall of the trachea. In our study, 7 (5.9%) cysts were removed incompletely for the concern of vascular or tracheal injury, which was similar to that reported in the literature [4, 6]. Treatment with physical damage (i.e., electrocautery) or chemical agents (i.e., alcohol or iodine tincture) should be performed to destroy the epithelial layer of the residual cyst wall. For large MBC, the needle suction of the fluid could be performed to reduce the interfacial tension of the cyst and make the dissection easy. When the cyst was located in anterior mediastinum, thymectomy should be performed on the patients whose diagnosis of thymoma could not be ruled out by radiological examinations and intraoperative exploration.
This study has important limitations for its single-institution, retrospective analysis, small sample size, and relatively short follow-up time. Large prospective and long-term follow-up studies are suggested to confirm the conclusion.
Conclusion
VATS excision of the MBC was safe and reliable and should be considered as the primary therapeutic option for the management of MBCs. The maximal diameter of MBC >5 cm was significantly associated with risk of operation time extension and bleeding loss increasing. Early surgical excision of MBC is recommended to establish histopathological diagnosis, relieve clinical symptoms, and prevent surgery-related complications.
References
Maier HC (1948) Bronchogenic cysts of the mediastinum. Ann Surg 127:476–502
St-Georges R, Deslauriers J, Duranceau A et al (1991) Clinical spectrum of bronchogenic cysts of the mediastinum and lung in the adult. Ann Thorac Surg 52:6–13
Ribet ME, Copin MC, Gosselin B et al (1995) Bronchogenic cysts of the mediastinum. J Thorac Cardiovasc Surg 109:1003–1010
Guo C, Mei J, Liu C et al (2016) Video-assisted thoracic surgery compared with posterolateral thoracotomy for mediastinal bronchogenic cysts in adult patients. J Thorac Dis 8:2504–2511
De Giacomo T, Diso D, Anile M et al (2009) Thoracoscopic resection of mediastinal bronchogenic cysts in adults. Eur J Cardiothorac Surg 36:357–359
Weber T, Roth TC, Beshay M et al (2004) Video-assisted thoracoscopic surgery of mediastinal bronchogenic cysts in adults: a single-center experience. Ann Thorac Surg 78:987–991
Limaiem F, Ayadi-Kaddour AH, Kilani T et al (2008) Pulmonary and mediastinal bronchogenic cysts: a clinicopathologic study of 33 cases. Lung 186:55–61
Mcadams HP, Kirejczyk WM, Rosado-De-Christenson ML et al (2000) Bronchogenic cyst: imaging features with clinical and histopathologic correlation. Radiology 217:441–446
Kirmani B, Sogliani F (2010) Should asymptomatic bronchogenic cysts in adults be treated conservatively or with surgery? Interact CardioVasc Thorac Surg 11:649–659
Fievet L, D’Journo XB, Guys JM et al (2012) Bronchogenic cyst: best time for surgery. Ann Thorac Surg 94:1695–1699
Patel SR, Meeker DP, Biscotti CV et al (1994) Presentation and management of bronchogenic cyst in the adult. Chest 106:79–85
Maurin S, Hery G, Bourliere B et al (2013) Bronchogenic cyst: clinical course from antenatal diagnosis to postnatal thoracoscopic resection. J Minim Access Surg 9:25–28
Lewis RJ, Caccavale RJ, Sisler GE et al (1992) Imaged thoracoscopic surgery: a new thoracic technique for resection of mediastinal cysts. Ann Thorac Surg 53:318–320
Tölg C, Abelin K, Laudenbach V et al (2005) Open versus thoracoscopic surgical management of bronchogenic cysts. Surg Endosc 19:77–80
Jung HS, Dong KK, Lee GD et al (2014) Video-assisted thoracic surgery for bronchogenic cysts: is this the surgical approach of choice? Interact CardioVasc Thorac Surg 19:824–829
Martinod E, Pons F, Azorin J et al (2000) Thoracoscopic excision of mediastinal bronchogenic cysts: results in 20 cases. Ann Thorac Surg 69:1525–1528
Read CA, Moront M, Carangelo R et al (1991) Recurrent bronchogenic cyst: an argument for complete surgical excision. Arch Surg 126:1306–1308
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Wang, X., Chen, K., Li, Y. et al. The Video-Assisted Thoracic Surgery for Mediastinal Bronchogenic Cysts: A Single-Center Experience. World J Surg 42, 3638–3645 (2018). https://doi.org/10.1007/s00268-018-4660-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4660-4