Abstract
Introduction
Colorectal cancer (CRC) is the second leading cause of cancer mortality in the USA. We aimed to determine racial and socioeconomic disparities in the surgical management and outcomes of patients with CRC in a contemporary, national cohort.
Methods
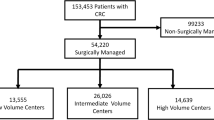
We performed a retrospective analysis of the National Inpatient Sample for the period 2009–2015. Adult patients diagnosed with CRC and who underwent colorectal resection were included. Multivariable linear and logistic regressions were used to assess the effect of race, insurance type, and household income on patient outcomes.
Results
A total of 100,515 patients were included: 72,552 (72%) had elective admissions and 27,963 (28%) underwent laparoscopic surgery. Patients with private insurance and higher household income were consistently more likely to have laparoscopic procedures, compared to other insurance types and income levels, p < 0.0001. Black patients, compared to white patients, were more likely to have postoperative complications (OR 1.23, 95% CI, 1.17, 1.29). Patients with Medicare and Medicaid, compared to private insurance, were also more likely to have postoperative complications (OR 1.30, 95% CI, 1.24, 1.37 and OR 1.40, 95% CI, 1.31, 1.50). Patients in low-household-income areas had higher rates of any complication (OR 1.11, 95% CI 1.06, 1.16).
Conclusions
The use of laparoscopic surgery in patients with CRC is strongly influenced by insurance type and household income, with Medicare, Medicaid and low-income patients being less likely to undergo laparoscopic surgery. In addition, black patients, patients with public insurance, and patients with low household income have significant worse surgical outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the third most commonly diagnosed cancer in males and females and the second most common cause of cancer mortality in the USA [1]. Surgical resection is the mainstay treatment for CRC. Specifically, laparoscopic surgery has been shown to be a safe alternative to open surgery, offering faster recovery and comparable oncological outcomes in patients with colon cancer [2].
Previous studies have described variations in CRC incidence and mortality in patients with different race and socioeconomic status. For instance, black patients have shown to be diagnosed with CRC at younger ages and with more advanced diseases than white patients [3,4,5]. Low socioeconomic status (SES) groups also have a higher incidence of CRC and less favorable survival outcomes compared with high SES groups in the USA [6,7,8].
Differences in surgical management and postoperative outcomes in patients with CRC across race and SES status should also be explored to better define strategies to ameliorate inequalities. Therefore, we aimed to determine racial and socioeconomic disparities in the surgical management and outcomes of patients with CRC in a contemporary, national cohort.
Methods
We performed a retrospective analysis of the National Inpatient Sample (NIS) database to assess potential disparities in the surgical treatment of CRC. The NIS is an all-payer American health care database and represents around 20% of all hospital admissions in the USA. Patients are identified in the database using ICD-9-CM diagnostic and procedural codes.
Hospitalizations of adult patients (≥ 18 years old), diagnosed with CRC (ICD-9-CM 153–154.8), and who underwent either laparoscopic (17.3–17.39, 45.81, 48.42, and 48.51) or open (45.7–45.79, 45.82, 45.83, 48.40, 48.43, 48.49, 48.50, 48.52, 48.59, 48.64, and 48.69) colorectal resection while admitted between January 1, 2009, (the first year all laparoscopic codes were implemented by) and September 30, 2015, (before ICD-10 codes were implemented) were eligible for inclusion. Patients with non-Medicare, Medicaid, or private insurance (n = 5623), diagnosed with both colon and rectal cancer (n = 712), or who underwent surgery >5 days after admission or who were missing the date of surgery (n = 15,249) were excluded. Patients with procedure codes for both laparoscopic and open resections were classified as open.
Outcomes analyzed in the study included postoperative morbidity, inpatient mortality, length of stay (LOS) after surgery, and inflation-adjusted total charges. Due to concern for bias introduced in patients that received surgical intervention after an extensive hospitalization, analysis was restricted to patients who underwent surgery within 5 days. Comorbidities of interest and postoperative complications included in our study, along with their corresponding codes, were previously described [9, 10].
Statistical analyses
Patient demographics and hospital characteristics were compared across procedure and admission type using Chi-square and Student’s t tests. Quarterly trends of laparoscopic, versus open, colorectal resections, stratified by race/ethnicity, primary insurance type, and estimated median household income of the patient’s ZIP code, were estimated using Poisson regression.
Multivariable analyses on the potential association between race/ethnicity, primary insurance type, and estimated median household income of the patient’s ZIP code on patient outcomes were performed using linear and logistic regression, where appropriate. Models were adjusted for admission year, elective admission, laparoscopic procedure, age, sex, cancer diagnosis (colon vs. rectal cancer), comorbidities, hospital region, teaching status, and hospital size. Age was modeled as a restricted cubic spline. Interaction terms were used to assess whether the effect of race/ethnicity, primary insurance type, and estimated median household income in the patient’s ZIP code on the odds of complication was consistent across cancer diagnosis.
A p value <0.05 was considered significant for all the statistical methods.
Results
A total of 100,515 patients were included, and 72,552 (72%) had elective admissions and 27,963 (28%) underwent laparoscopic surgery. Laparoscopic procedures were significantly more frequent in elective (43%) than emergent (22%) admissions, p < 0.0001. 84,889 (84%) of patients were diagnosed with colon cancer and 15,626 (16%) were diagnosed with rectal cancer. Patient demographics, comorbidities, and hospital characteristics stratified by admission status and surgical approach are shown in Table 1. Racial differences in the prevalence of comorbidities were also assessed, as shown in Table 2.
From 2009 to 2015, there was almost a 50% increase in laparoscopic procedures in both elective and emergent admissions, p < 0.0001 and p < 0.0001 (Fig. 1). And while laparoscopic use was similar over time across races/ethnicity (Fig. 2a), patients with private insurance (Fig. 2b) and higher household incomes (Fig. 2c) were consistently more likely to have laparoscopic procedures, compared to other insurance types and income levels, p < 0.0001 and p < 0.0001.
Overall, 36% of patients (n = 35,787) had at least one inpatient complication. Specifically, 4% (n = 4134) of patients had a venous thromboembolism, 1% (n = 1282) had wound complications, 9% (n = 9204) developed an infection, 20% (n = 20,527) had a bleeding complication, <1% (n = 492) developed shock, 8% (n = 7611) had cardiac failure, 8% (n = 8206) had renal failure, and 5% (n = 4652) had respiratory failure. Mean LOS after surgery was 7.2 days (standard deviation 6.1 days).
Black patients, compared to white patients, were overall more likely to have postoperative complications (OR 1.23, 95% CI, 1.17, 1.29). Additionally, these patients were more likely to have postoperative bleeding (OR 1.32, 95% CI 1.26, 1.38), cardiac failure (OR 1.17, 95% CI 1.09, 1.26), renal failure (OR 1.40, 95% CI 1.32, 1.50), and respiratory failure (OR 1.13, 95% CI 1.04, 1.23) (Table 3). When stratified by cancer type, the increased odds of complications was more substantial in black patients, compared to white patients, among those with rectal cancer (OR 1.45, 95% CI 1.27, 1.65) than those with colon cancer (OR 1.19, 95% CI 1.13, 1.26), p = 0.008. The effect of Hispanic and other race was consistent across cancer diagnosis, p = 0.36 and p = 0.99, respectively. Moreover, the association between race and complications has remained consistent between 2009 and 2015, p = 0.50.
Patients with Medicare or Medicaid, respectively, compared to patients with private insurance, were overall more likely to have postoperative complications (OR 1.30, 95% CI, 1.24, 1.37), (OR 1.40, 95% CI, 1.31, 1.50) among Medicare and Medicaid patients, respectively. Additionally, these patients were more likely to have postoperative infection (OR 1.25 and 1.32, respectively), bleeding (OR 1.15 and 1.36, respectively), cardiac failure (OR 1.52 and 1.78, respectively), renal failure (OR 1.38 and 1.26, respectively), respiratory failure (OR 1.51 and 1.62, respectively), shock (OR 1.81 and 1.73, respectively), and inpatient mortality (OR 1.50 and 1.56, respectively), compared to patients with private insurance (Table 4). When stratified by cancer type, there were no meaningful differences in the impact of Medicare or Medicaid, compared to private insurance, on the odds of complications, p = 0.32 and p = 0.22. The effect of insurance type on complications has remained consistent over time, p = 0.23.
Patient living in areas with low median household incomes, compared to patients living in areas with the highest income quartile, were more likely to have postoperative cardiac failure (OR 1.16, 95% CI 1.09, 1.24), renal failure (OR 1.11, 95% CI 1.04, 1.18), respiratory failure (1.09, 95% CI 1.01, 1.18), and inpatient mortality (1.17, 95% CI 1.05, 1.83) (Table 5). When stratified by cancer diagnosis, no differences were seen in the impact of patients living in low, medium, or high median household income areas, compared to highest income, p = 0.74, p = 0.61, p = 0.93, respectively. The effect of median household income in the patient’s ZIP code on complications has remained consistent over time, p = 0.28.
Discussion
We aimed to determine current disparities in surgical outcomes of patients with CRC in the USA. We found that (a) the increase in laparoscopic surgery was particularly notable in patients with private insurance and high household income; (b) black patients were more likely to have worse postoperative outcomes; and (c) patients with Medicare and Medicaid, and patients with low household income had also worse postoperative outcomes.
Previous studies have identified benefits of laparoscopic surgery for CRC. Weeks et al. [11] conducted a multicenter randomized trial with 449 consecutive patients with resectable colon cancer, and found that patients undergoing laparoscopic colectomy, as compared to open colectomy, required fewer days of both parenteral and oral analgesics. Similarly, another randomized trial showed that laparoscopic colectomy was associated with shorter length of hospital stay, faster recovery of gastrointestinal motility, and less use of pain medication [12]. Milsom et al. [13] also found that laparoscopic colectomy offered a faster recovery of pulmonary and gastrointestinal function compared with conventional surgery, without any apparent short-term oncologic disadvantages. The long-term outcomes of the Australasian randomized clinical trial confirmed that the laparoscopic approach was not inferior to open colon resection in direct measures of survival and disease recurrence [14]. Unfortunately, disadvantaged patients are less likely to obtain the benefits of minimally invasive surgery in colon cancer. We have demonstrated that the use and embracement of laparoscopic colectomy was significantly higher in patients with private insurance and high household income.
Racial disparities in CRC are notorious. Since 1960, CRC mortality declined by around 40% among whites, but increased by around 30% among African–Americans [15]. In addition, both incidence and mortality are higher among black patients when compared with other race/ethnicities [16, 17]. The underlying factors contributing to racial disparities, including those impacting the higher mortality rates in black patients are likely multiple and complex. Most studies have focused on the prevalence of risk factors, the biology of particular tumor types, reduced access and use of CRC screening, mistrust in the healthcare system, and reduced use of the healthcare system seen in black patients [3,4,5, 18,19,20]. Our study suggests that worse postoperative outcomes, including life-threatening complications, in black patients, compared to white patients, may also play an important role. Our paper also looked at whether laparoscopic surgery was different across patient characteristics and found that race did not appear to play a role in surgery type (open vs. laparoscopic), correlating with previous studies with minimal difference in laparoscopic surgery use across race [21, 22]. However, despite this, we found that black patients were more likely to have complications after their surgery, even after adjusting for surgical approach. Furthermore, this trend of increased complications has not improved but rather stayed consistent over time, suggesting little benefit of current public health measures in addressing this disparity. A study by Mehtsun et al. [23] found mortality trends improving by 0.10 percent per year and 0.07 percent per year, for black and white patients, respectively. Interestingly, our study did not find any improvement between the disparities of black patients, as compared to white patients, over the time period.
Insurance and SES status should also be considered when analyzing disparities in CRC. A study using the Surveillance, Epidemiology and End Results (SEER) database showed that Medicaid patients and the lowest education level group patients with CRC had poorer prognosis [7]. Robbins et al. [24] used data from the National Cancer Data Base (NCDB) and examined insurance status and survival among 19,154 rectal cancer patients aged 18–64 years. The authors found that the hazard ratio for death at 5 years, considering privately insured patients as reference, was 2.05 (95% CI, 1.89–2.23) among Medicaid-insured patients, and 2.01 (95% CI, 1.84–2.19) among uninsured patients. Similarly, another study showed that the prevalence of comorbidities among adult colorectal cancer patients was lower in those with private insurance, and higher in those insured by public insurance or who were uninsured. Survival at 1 year was also poorer for patients without private health insurance [25]. In line with these findings, we also found that patients with Medicare, Medicaid, and patients with low household income had poorer prognosis. Specifically, these patients were more likely to have serious postoperative complications and inpatient mortality after colorectal resection for cancer. Furthermore, this increased likelihood of worsened complications and outcomes was not found to improve over the study period.
There are multiple limitations in this retrospective study. The NIS does not link hospital records, thereby all postoperative complications and mortality are limited to the initial admission, which underestimates the overall incidence. Similarly, we used administrative codes to identify comorbidities and complications, which means that missing codes would cause us to also underestimate the prevalence and incidence, respectively. However, many of the complications would be serious and have a significant impact on patient treatment and outcomes, which may make them less likely to be missed. There is also the potential for coding errors in large administrative databases. In addition, details about the complexity of the cases and stage of disease are not provided by NIS, and we were not able to adjust for it. These factors are likely to influence the severity at presentation and increase the probability of inpatient complications. Moreover, if differences in severity exist across race/ethnicity, primary insurance or estimated median household income for the patient’s ZIP code, these unmeasured differences could potentially bias our results. However, we attempted to minimize the impact of this by adjusting for cancer type. Finally, the income variable is not a patient-level measurement, but rather the median household income for patient’s ZIP code. Future research should assess the potential impact of SES on postoperative outcomes is needed.
Conclusions
The use of minimally invasive surgery in patients with CRC is strongly influenced by insurance type and household income, with patients with non-private insurance and low income having less laparoscopic surgery. In addition, black patients, patients with public insurance, and patients with low household income have significantly worse postoperative outcomes. This analysis highlights that disparities in surgical treatment, as well as postoperative morbidity and mortality, still persist. Greater public health programming and surgeon-specific treatment strategies to reduce these disparities and improve surgical outcomes in underserved patients with CRC are needed.
References
Siegel RL, Miller KD, Fedewa SA et al (2017) Colorectal cancer statistics, 2017. CA Cancer J Clin 67(3):177–193
Chen CF, Lin YC, Tsai HL, et al (2018) Short-and long-term outcomes of laparoscopic-assisted surgery, mini-laparotomy and conventional laparotomy in patients with Stage I–III colorectal cancer. J Minim Access Surg, epub ahead of print
Shavers VL (2007) Racial/ethnic variation in the anatomic subsite location of in situ and invasive cancers of the colon. J Natl Med Assoc 99:733–748
Dignam JJ, Colangelo L, Tian W et al (1999) Outcomes among African–Americans and Caucasians in colon cancer adjuvant therapy trials: findings from the National Surgical Adjuvant Breast and Bowel Project. J Natl Cancer Inst 91:1933–1940
Doubeni CA, Field TS, Buist DS et al (2007) Racial differences in tumor stage and survival for colorectal cancer in an insured population. Cancer 109:612–620
Aarts MJ, Lemmens VE, Louwman MW et al (2010) Socioeconomic status and changing inequalities in colorectal cancer? A review of the associations with risk, treatment and outcome. Eur J Cancer 46:2681–2695
Zhang Q, Wang Y, Hu H et al (2017) Impact of socioeconomic status on survival of colorectal cancer patients. Oncotarget 8:106121–106131
Jemal A, Siegel R, Ma J et al (2015) Inequalities in premature death from colorectal cancer by state. J Clin Oncol 33:829–835
Schlottmann F, Strassle PD, Charles AG et al (2018) Esophageal cancer surgery: spontaneous centralization in the US contributed to reduce mortality without causing health disparities. Ann Surg Oncol 25(6):1580–1587
Schlottmann F, Gaber C, Strassle PD, et al (2018) Cholecystectomy vs. cholecystostomy for the management of acute cholecystitis in elderly patients. J Gastrointest Surg, epub ahead of print
Weeks JC, Nelson H, Gelber S et al (2002) Short-term quality-of-life outcomes following laparoscopic-assisted colectomy vs open colectomy for colon cancer: a randomized trial. JAMA 287(3):321–328
Kaiser AM, Kang JC, Chan LS et al (2004) Laparoscopic-assisted vs. open colectomy for colon cancer: a prospective randomized trial. J Laparoendosc Adv Surg Tech 14(6):329–334
Milsom JW, Bohm B, Hammerhofer KA et al (1998) A prospective, randomized trial comparing laparoscopic versus conventional techniques in colorectal cancer surgery: a preliminary report. J Am Coll Surg 187(1):46–54
Bagshaw PF, Allardyce RA, Frampton CM et al (2012) Long-term outcomes of the Australasian randomized clinical trial comparing laparoscopic and conventional open surgical treatments for colon cancer: the Australasian Laparoscopic Colon Cancer Study trial. Ann Surg 256(6):915–919
Soneji S, Iyer SS, Armstrong K, Asch DA (2010) Racial disparities in stage-specific colorectal cancer mortality: 1960–2005. Am J Public Health 100:1912–1916
Siegel R, Naishadham D, Jemal A (2013) Cancer statistics, 2013. CA Cancer J Clin 63:11–30
Tammana VS, Laiyemo AO (2014) Colorectal cancer disparities: issues, controversies and solutions. World J Gastroenterol 20(4):869–876
Bolen JC, Rhodes L, Powell-Griner EE et al (2000) State-specific prevalence of selected health behaviors, by race and ethnicity—behavioral risk factor surveillance system, 1997. MMWR CDC Surveill Summ 49:1–60
Advani AS, Atkeson B, Brown CL et al (2003) Barriers to the participation of African–American patients with cancer in clinical trials: a pilot study. Cancer 97:1499–1506
Gregg J, Curry RH (1994) Explanatory models for cancer among African–American women at two Atlanta neighborhood health centers: the implications for a cancer screening program. Soc Sci Med 39:519–526
Ravi P, Sood A, Schmid M et al (2015) Racial/ethnic disparities in perioperative outcomes in major procedures: results from national surgical quality improvement program. Ann Surg 262(6):955–964
Alnasser M, Schneider EB, Gearhart SL et al (2014) National disparities in laparoscopic colorectal procedures for colon cancer. Surg Endosc 28(1):49–57
Mehtsun WT, Figueroa JF, Zhang J et al (2017) Racial disparities in surgical mortality: the gap appears to have narrowed. Health Affairs 36(6):64
Robbins AS, Chen AY, Stewart AK et al (2010) Insurance status and survival disparities among nonelderly rectal cancer patients in the national cancer data base. Cancer 116:4178–4186
Robbins AS, Pavluck AL, Fedewa SA et al (2009) Insurance status, comorbidity level, and survival among colorectal cancer patients age 18 to 64 years in the national cancer data base from 2003 to 2005. J Clin Oncol 27:3627–3633
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cairns, A.L., Schlottmann, F., Strassle, P.D. et al. Racial and Socioeconomic Disparities in the Surgical Management and Outcomes of Patients with Colorectal Carcinoma. World J Surg 43, 1342–1350 (2019). https://doi.org/10.1007/s00268-018-04898-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-04898-5