Abstract
Background
Total thyroidectomy can be performed for Graves’ disease after a euthyroid state is achieved using inhibitors of thyroid hormone synthesis (thioamides). However, hypervascularization of the thyroid gland is associated with increased hemorrhage risk, in addition to complicating identification of the recurrent laryngeal nerve and parathyroid gland. Saturated iodine solution (Lugol’s solution) has been recommended to reduce thyroid gland hypervascularization and intraoperative blood loss, although this approach is not used at our center based on our experience that it induces thyroid firmness and potentially hypoparathyroidism.
Methods
This retrospective single-center study evaluated patients who underwent total thyroidectomy for Graves’ disease between November 2010 and November 2015. The rates of various complications at our center were compared to those from the literature (e.g., cervical hematoma, hypocalcemia, and recurrent laryngeal nerve palsy).
Results
Three hundred and eighty consecutive patients underwent total thyroidectomy without preoperative Lugol’s solution (311 women [81.84%] and 69 men [18.16%], mean age 43.41 years). No postoperative deaths were reported, although 30 patients (7.89%) experienced recurrent laryngeal nerve palsy and 9 patients experienced permanent injuries (2.37%). Hypoparathyroidism was experienced by 87 patients (25.53%) and 14 patients experienced permanent hypoparathyroidism (3.68%). Four patients required reoperation for cervical hematoma (1.05%; 2 deep and 2 superficial hematomas).
Conclusion
Despite the recommendation of iodine pretreatment, few of our non-pretreated patients experienced permanent nerve injury (2.37%) or permanent hypoparathyroidism (3.68%). These results are comparable to the outcomes from the literature. Randomized controlled trials are needed to determine whether iodine pretreatment is necessary before surgery for Graves’ disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total thyroidectomy is a definitive treatment for Graves’ disease (also known as Basedow disease) that is frequently used in cases with recurrence, failed or intolerable medical treatment, a goiter, suspected malignancy, or pregnancy [1]. Surgery for Graves’ disease is planned after a euthyroid state has been achieved using inhibitors of thyroid hormone synthesis (thioamides) [2,3,4]. However, these patients can have hypervascularization of the thyroid gland, which is associated with increased hemorrhage risk, in addition to complicating identification of the recurrent laryngeal nerve and parathyroid gland. Therefore, it is recommended that a saturated iodine solution (e.g., Lugol’s solution) be used as a pretreatment to reduce thyroid gland hypervascularization and intraoperative blood loss [2]. In this context, Lugol’s solution rapidly and effectively decreases the synthesis and circulatory release of thyroid hormones [5]. Furthermore, it decreases thyroid gland vascularization, thyroid artery blood flow, and intraoperative blood loss [6].
In our experience, iodine pretreatment induce a reaction in the thyroid gland increasing firmness of the gland. This can make it extremely difficult to selectively remove the thyroid gland without harming the parathyroid gland. Thus, based on the possible postoperative hypoparathyroidism, our center has not used iodine pretreatment for several years. This retrospective study aimed to evaluate the outcomes of thyroid surgery without iodine pretreatment for Graves’ disease at our center and to compare those outcomes to the outcomes from the literature.
Methods
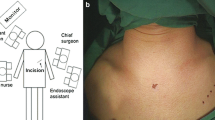
This retrospective study evaluated consecutive patients who underwent total thyroidectomy for Graves’ disease between November 2010 and November 2015. Most identified patients were included in the present study, with the exception of 3 patients who preoperatively received Lugol’s solution from their endocrinologist. The patients were treated by three endocrine surgeons from the same department and were followed-up for at least 6 months, with the exception of 1 patient who was lost to follow-up.
All interventions were performed using intraoperative monitoring of the recurrent laryngeal nerve (NIM 2.0; Medtronic, Jacksonville, FL, USA). At the start of the intervention, systematic bilateral vagal stimulation was performed, and flexible laryngoscopy was performed to identify vocal cord immobilization or recurrent laryngeal nerve palsy in cases with significant modification or loss of the vagal signal. In addition, flexible laryngoscopy was performed on the first postoperative day if the patient’s voice appeared to be modified, even if the recurrent laryngeal nerve signal was preserved at the end of the surgery. Vocal cord immobilization (or recurrent laryngeal nerve palsy) was considered present when the flexible laryngoscopy provided visual confirmation that the vocal cords did not vibrate during attempts to speak, and the palsy was considered permanent when the immobilization persisted for >6 months.
All patients underwent serum calcium testing on the first postoperative day, and on all other hospitalization days if their stay was >24 h. Hypoparathyroidism was defined as a postoperative serum calcium level of <2 mmol/L (<8 mg/dL) in the absence of calcium supplementation. Patients with hypoparathyroidism were treated using alfacalcidol (1–2 µg twice per day) and calcium carbonate (500 mg three times per day), and the hypoparathyroidism was considered permanent if the alfacalcidol treatment was still required at >6 months after the surgery.
Results
During the study period, 380 patients were considered eligible because they had undergone total thyroidectomy without preoperative Lugol’s solution for Graves’ disease. The patients included 311 women (81.8%) and 69 men (18.2%) and had an average age of 43.4 years (range 5–89 years). No postoperative deaths were reported.
Thirty patients (7.9%) experienced recurrent laryngeal nerve palsy, with 11 cases involving the right nerve, 18 cases involving the left nerve, and 1 case involving bilateral palsy. One patient had immediate recurrent laryngeal nerve palsy without voice change, which was confirmed using flexible laryngoscopy. Nine patients experienced permanent vocal cord palsy (30% of affected cases and 2.37% of all cases), 18 patients experienced transient vocal cord palsy, and 3 patients did not attend their 6-month follow-up (2 patients refused because of scheduling issues and 1 patient was lost to follow-up). If the lost patients were considered to have permanent nerve damage, the overall rate of permanent palsy increased to 3.16%.
Ninety-seven patients (25.5%) experienced postoperative hypoparathyroidism, with 87 patients experiencing transient hypoparathyroidism and 14 patients experiencing permanent hypoparathyroidism (14.4% of affected cases and 3.7% of all cases). One patient was lost to follow-up, and if that patient was considered to have permanent hypoparathyroidism, the overall rate of permanent hypoparathyroidism increased to 3.9%.
Four patients underwent reoperation. A 27-year-old man underwent two reoperations for deep compressing cervical hematomas at 16 and 24 h after the original surgery. Active bleeding from a branch of the superior thyroidal artery was identified, controlled, and then drained. A 47-year-old woman underwent reoperation at 5 h after the original surgery for a deep compressing cervical hematoma. No active bleeding was detected during the surgical exploration, and a drain was left in situ after removing a blood clot. A 48-year-old woman underwent reoperation on the same day as the original surgery because of a superficial cervical hematoma, which likely formed because she required anticoagulation therapy for a mechanical cardiac valve. A 48-year-old man underwent reoperation for a superficial cervical hematoma on the same day as the original surgery.
One case of bilateral vocal cord immobilization without traumatic nerve damage was detected. The patient was reintubated because of respiratory distress in the post-anesthesia recovery unit and was successfully extubated after 2 days of corticotherapy without tracheotomy. Both vocal cords were mobile at the 1-month postoperative visit.
Discussion
The present study examined our surgical team’s experience performing total thyroidectomy for Graves’ disease. Despite the apparent consensus regarding the usefulness of a supersaturated iodine solution for patients with Graves’ disease, there remains debate among surgeons regarding this treatment’s benefits and consequences. Although there are numerous data regarding complications after total thyroidectomy, there is limited information in the context of Graves’ disease (vs. other pathologies), which makes comparisons difficult. The main finding of the present study is that even if surgery without Lugol’s solution for Graves’ disease may be considered more difficult and more hemorrhagic, our complication rates were similar to the rates from previous studies.
When all pathologies are considered, total thyroidectomy is associated with transient damage (0.2–9.8%) and permanent damage (0.7–5.65%) to the recurrent laryngeal nerve [7]. In the present study, the rates were 7.9% for transient injury and 2.4% for permanent vocal cord palsy, which agree with the previously reported results. Hypoparathyroidism is the other main complication of total thyroidectomy (transient 0.2–50.2%, permanent 0.5–4.4%) [7], and the present study revealed similar rates, which were 25.5% for transient hypoparathyroidism and 3.7% for permanent hypoparathyroidism. Moreover, a recent French prospective multicenter trial revealed that laryngoscopy-confirmed recurrent laryngeal nerve palsy was detected in 7.5% of 2369 total thyroidectomies that were performed for all diseases [7]. Among the cases with vocal cord palsy, 27.5% of the cases involved permanent palsy, which corresponded to an overall rate of 2.1% among all patients. Furthermore, the same study revealed rates of 25.1% for transient parathyroid malfunction and 2.7% for permanent dysfunction. In the French study, up to 11% of the patients had Graves’ disease [7]. The only significant risk factor for recurrent laryngeal nerve palsy was the inability to view the nerve, while female sex and central lymph node dissection were risk factors for permanent hypoparathyroidism [7]. However, Graves’ disease was not associated with increased risks of recurrent laryngeal nerve injury or hypoparathyroidism among the patients who underwent total thyroidectomy. When patient with Graves’ disease was specifically analyzed, the recurrent laryngeal nerve palsy rates were 6.6% for transient palsy and 3.5% for permanent palsy, while the hypoparathyroidism rates were 30.7% for temporary malfunction and 3.4% for permanent dysfunction [7]. Those results are similar to the findings of the present study. As the thyroidectomies were performed by experienced surgeons, the complications in this study cannot be the result of a learning curve effect [8] An older study of 714 patients who underwent thyroid surgery for Graves’ disease (156 total thyroidectomies and 558 near-total thyroidectomies with <2 g of remaining thyroid parenchyma on one side) revealed recurrent laryngeal nerve palsy rates of 2.2% for transient palsy and 0.4% for permanent palsy, and rates of 10.2% for transient hypoparathyroidism and 1.5% for permanent hypoparathyroidism [9]. However, that report did not describe the preoperative use of a saturated iodine solution. Another retrospective study examined 1432 patients who received Lugol’s solution pretreatment before surgery for Graves’ disease (971 total thyroidectomies) and revealed rates of 0.9% for permanent recurrent laryngeal palsy and 3.2% for permanent hypoparathyroidism [10]. Several others series have reported similar outcomes [11,12,13].
Lugol’s solution pretreatment is recommended before total thyroidectomy for Graves’ disease [2], with a standard dosage of 7 drops daily for 10 days before surgery. This treatment is intended to decrease thyroid gland vascularization by modifying arterial blood flow and increasing arterial resistance index [5, 6, 14, 15]. One report has indicated that this treatment reduces the intraoperative blood loss (Lugol’s pretreatment 54 mL, no pretreatment 109 mL) [6]. In theory, the reduced bleeding in the operative field enhances recognition of the structures of interest (recurrent laryngeal nerve and parathyroid glands). However, our experience is that Lugol’s solution modifies the thyroid gland’s texture through an apparently fibrotic reaction with adhesion to the surrounding tissue. This increases the difficulty of locating and dissecting the parathyroid gland, which increases the risk of parathyroid devascularization. Moreover, we have observed that the hypervascularization that is associated with Graves’ disease persists, even if it is reduced. Thus, vascular control using ligation as the first step remains critical, although it can be time consuming and require careful attention. Finally, Lugol’s solution is associated with various benign side effects, such as diarrhea, vomiting, gastric pain, skin eruption, or neck discomfort [16].
The recommendations of preoperative saturated iodine solution appear to be supported by low-quality evidence, based on the statement from the America Thyroid Association [2]. For example, Shinall et al.’s [17] retrospective study at a high-volume center for thyroid surgery revealed no significant differences in complications or blood loss between patients who did and did not receive iodine pretreatment, similar to patients with a multinodular goiter. To the best of our knowledge, no study has revealed an absolute decrease in postoperative complications among cases that received iodine pretreatment. In another European center, Robert et al. [18] reported rates of 34.0% for transient hypoparathyroidism and 8.5% for permanent hypoparathyroidism, which are higher than the rates at our center.
The present study has several limitations. First, the retrospective single-center design is associated with known risks of bias. Second, the serum calcium results were analyzed by our surgical team, which might have led to bias and underreporting of transient hypoparathyroidism. This is because transient hypoparathyroidism has a less objective definition that is based on laboratory results (vs. permanent hypoparathyroidism). In addition, there are data challenging the validity of using this complication as a measure of thyroid surgery quality [19]. In contrast, vocal assessments were performed by unrelated physicians when the surgeons reported intraoperative nerve signal loss or postoperative voice modification. The decision to only use flexible laryngoscopy for these patients was based on the results of a randomized controlled trial, which revealed few missed nerve injuries when both signals were intact after nerve dissection (negative predictive value 98.9%) [20]. Therefore, we believe that the systematic use of laryngoscopy prevented underreporting of recurrent laryngeal nerve palsy. However, the low threshold for vocal cord control could have resulted in an artificially high rate of vocal cord immobilization.
Conclusion
The present study revealed that total thyroidectomy without iodine pretreatment for Graves’ disease was associated with similar surgical morbidity rates, compared to the reported rates. Furthermore, there was no apparent relationship with transient or permanent recurrent laryngeal nerve injury and hypoparathyroidism. Although a randomized controlled trial is needed to evaluate this issue, our team avoids iodine pretreatment in these cases based on our experience that it complicates the surgery because of the resulting fibrotic reaction.
Change history
08 February 2018
In the original article, Mathieu Bonal’s last name was spelled incorrectly. It is correct as reflected here. The original article has also been updated.
References
De Leo S, Lee SY, Braverman LE (2016) Hyperthyroidism. Lancet 388:906–918
Ross D, Burch HB, Cooper DS et al (2016) 2016 American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid 26:1343–1421
Orgiazzi J (2011) The treatment of Graves’ disease: current views and controversies. Presse Med 40:1155–1162 (in French)
Pearce EN (2006) Diagnosis and management of thyrotoxicosis. BMJ 332:1369–1373
Huang SM, Liao WT, Lin CF et al (2015) Effectiveness and mechanism of preoperative lugol solution for reducing thyroid blood flow in patients with euthyroid Graves’ disease. World J Surg 40:505–509. https://doi.org/10.1007/s00268-015-3298-8
Erbil Y, Ozluk Y, Giris M et al (2007) Effect of lugol solution on thyroid gland blood flow and microvessel density in the patients with Graves’ disease. J Clin Endocrinol Metab 92:2182–2189
Daher R, Lifante JC, Voirin N et al (2015) Is it possible to limit the risks of thyroid surgery? Ann Endocrinol (Paris) 76(Suppl 1):S16–S26
Duclos A, Carty MJ, Peix JL et al (2012) Development of a charting method to monitor the individual performance of surgeons at the beginning of their career. PLoS ONE 7:e41944
Gaujoux S, Leenhardt L, Trésallet C et al (2006) Extensive thyroidectomy in Graves’ disease. J Am Coll Surg 202:868–873
Bojic T, Paunovic I, Diklic A et al (2015) Total thyroidectomy as a method of choice in the treatment of Graves’ disease-analysis of 1432 patients. BMC Surg 15:39–44
Stalberg P, Svensson A, Hessman AO et al (2008) Surgical treatment of Graves’ disease: evidence-based approach. World J Surg 32:1269–1277. https://doi.org/10.1007/s00268-008-9497-9
Liu ZW, Masterson L, Fish B et al (2015) Thyroid surgery for Graves’ disease and Graves’ ophthalmopathy. Cochrane Database Syst Rev 25:CD010576
Welch KC, McHenry CR (2011) Total thyroidectomy: Is morbidity higher for Graves’ disease than nontoxic goiter? J Surg Res 170:96–99
Chang DC, Wheeler MH, Woodcock JP et al (1987) The effect of preoperative Lugol’s iodine on thyroid blood flow in patients with Graves’ hyperthyroidism. Surgery 102:1055–1061
Ansaldo GL, Pretolesi F, Varaldo E et al (2000) Doppler evaluation of intrathyroid arterial resistances during preoperative treatment with Lugol’s iodide solution in patients with diffuse toxic goiter. J Am Coll Surg 191:607–612
Burch HB, Cooper DS (2015) Management of Graves’ disease: a review. JAMA 314:2544–2554
Shinall MC Jr., Broome JT, Baker A et al (2013) Is potassium iodide solution necessary before total thyroidectomy for Graves disease? Ann Surg Oncol 20:2964–2967
Robert J, Mariéthoz S, Pache JC et al (2001) Short- and long-term results of total vs subtotal thyroidectomies in the surgical treatment of Graves’ disease. Swiss Surg 7:20–24
Lifante JC, Payet C, Menegaux F et al (2017) Can we consider immediate complications after thyroidectomy as a quality metric of operation? Surgery 161:156–165
Barczynski M, Konturek A, Cichon S (2009) Randomized clinical trial of visualization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br J Surg 96:240–246
Acknowledgements
We thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report that they have no conflict of interest that is relevant to this report.
Additional information
The original version of this article was revised: Mathieu Bonal's last name was spelled incorrectly.
Rights and permissions
About this article
Cite this article
Mercier, F., Bonal, M., Fanget, F. et al. Does Surgery Without Lugol’s Solution Pretreatment for Graves’ Disease Increase Surgical Morbidity?. World J Surg 42, 2123–2126 (2018). https://doi.org/10.1007/s00268-017-4443-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4443-3