Abstract
Background
Chest X-ray (CXR) prior to thyroid surgery continues to be routinely obtained at some institutions despite the lack of evidence for its utility. This study aimed to determine the utility of preoperative CXR in patients undergoing thyroidectomy at a single institution.
Methods
In total, 594 thyroidectomy patients were included in the study. Demographics, CXR findings, anesthesia records and pathologic data were assessed. We investigated whether difficult intubation or cancer stage correlated with the presence of CXR abnormalities.
Results
Of the total cohort, 83% had a preoperative CXR and 67% had cancer on surgical pathology. In total, 56% had at least one CXR abnormality, the most frequent being skeletal abnormalities (25%), followed by tracheal deviation (16%). Of 78 patients (15.8%) with tracheal deviation on CXR, only 5% had a difficult intubation. Tracheal deviation was more commonly seen in non-cancer cases compared to cancer cases (27 vs. 12%, p < 0.001). CXR impacted management in 4%. Among patients with cancer, a higher T-stage (>2) was associated with higher rate of tracheal deviation compared to T1 (17 vs. 8%, p < 0.001). While patients with non-metastatic cancer (n = 277) compared to metastatic cancer patients had a higher proportion of any abnormality on CXR (57 vs. 44%, p = 0.045), there was no significant difference for tracheal deviation, skeletal abnormalities or lung nodules. Of patients with nodules on CXR (n = 29), only 14% were found to have metastatic disease.
Conclusion
The utility of preoperative CXR in patients undergoing thyroidectomy is very limited. In the climate of value-based care, routine use of this modality may be redundant and should only be ordered if clinically indicated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chest X-ray (CXR) prior to thyroid surgery continues to be routinely obtained despite the lack of evidence to establish its utility [1]. The practice first emerged in the 1940s when CXRs were ordered to identify asymptomatic tuberculosis carriers, and evolved thereafter to routine preoperative testing to identify underlying disease and help in postoperative care [2]. The routine practice of ordering preoperative chest X-rays was questioned in the 1970s [3]. The first major systematic review of the preoperative chest radiograph in elective non-cardiopulmonary surgery was published in 1979 in Lancet by the Royal College of Radiologists [4]. Studies have been conducted since in an attempt to establish appropriate criteria for testing [3]. Unnecessary testing would be adding medical, financial and personal expenses without benefit. This study aimed to determine the utility of preoperative CXR in patients undergoing thyroidectomy.
Materials and methods
A retrospective chart review was performed involving patients who underwent thyroid surgery at the Cleveland Clinic Main Campus from January 2004 to December 2009 after approval by the Cleveland Clinic Institutional Review Board (IRB). Cases were identified using search terms thyroid lobectomy, total thyroidectomy and chest X-ray. We utilized the electronic medical record (EMR) which captures basic demographic information and other clinically relevant clinicopathologic information. A file database was created for data collection that was accessible only by authorized study personnel. Each patient was assigned a consecutive study number which was used to identify all study-related data. Data were collected and managed using research electronic data capture (REDCap) which included patient identification, medical record number, age, gender and ethnicity. The REDCap database contained data on 668 patients. Seventy patients were listed as ineligible in field comments, and four additional patients had no information on X-rays leaving 594 total patients for analysis.
Five hundred and ninety-four consecutive patients who underwent thyroidectomy at the Cleveland Clinic were included in the study. Patients without preoperative CXR were excluded from the study. Retrospective chart review using the EMR was performed to collect data which included demographics, CXR findings, anesthesia records, pathologic data including cancer stage and the presence of metastases. For the purpose of this study, difficult intubation was defined as any patient who had intraoperative difficult mask ventilation, difficult laryngeal mask airway (LMA) ventilation, difficult intubation or difficult tracheotomy. For patients with cancer, the pathologic stage variable was coded as three separate variables for T, N and M. If multiple stages were recorded for a patient, the higher stage was used. If patients were noted to have nodules on the CXR, in addition to looking at each type of nodule individually, subcentimetric nodules and nodules that were ≥1 cm were combined together to create an “any nodule” category.
One new variable was created for the metastatic versus non-metastatic using the aggressiveness variable. Patients with findings on CXR were compared to those without, to see whether there was any correlation with difficult intubation or stage of cancer. For the statistical analysis, categorical variables were described using frequencies and percentages. Pearson’s Chi-square and Fisher’s exact tests were used to compare groups on the presence of abnormalities. Analyses used SAS software (version 9.3; Cary, NC).
Results and discussion
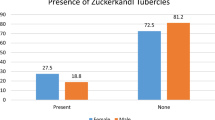
Of the 594 patients evaluated, 494 patients (83%) had a preoperative CXR. Of these, 362 cases (73.3%) were found to have cancer on surgical pathology. Of the patients with thyroid malignancy, 81 patients (16%) were found to have metastatic disease (Fig. 1). Four patients with malignancy did not have data on metastatic status.
There were 275 cases (55.7%) of all chest X-rays that had at least one abnormality. The most common abnormality was rib or skeletal abnormality that occurred in 125 (25.3%) of all chest X-rays (Table 1). This was followed by tracheal deviation (16%), cardiomegaly (12%), lung nodules (6%, of which 3% were subcentimetric and 0.5% showing diffuse nodularity), emphysema (2%) and pleural effusion (1%). Of 78 patients (15.8%) with tracheal deviation on CXR, only 5% had a difficult intubation during surgery. CXR was shown to impact management in 4%.
Non-cancer cases were more likely to have tracheal deviations when compared to cases with cancer on surgical pathology (27 vs. 12%, p < 0.001) (Fig. 2). Among patients with cancer, non-metastatic cancers were more likely than metastatic cancers to have any CXR abnormality (57 vs. 44%, p = 0.045). However, there was no significant difference for tracheal deviation or lung nodules on CXR (Fig. 3).
Patients with a higher T-stage were more likely to have tracheal deviation compared to those with lower T-stages (17 vs. 8%, p = 0.012) (Fig. 4). Of patients with nodules on CXR (n = 29), only 14% were shown to have metastatic disease. Of the 29 patients with any nodules, only 21 reported information on metastasis. Table 2 summarizes metastasis location for those with nodules. Of these 21, four (19.0%) showed distant metastasis. If one assumed that the eight patients without aggressiveness information were non-metastatic, these four distant metastasis cases would represent 13.7% of the 29 cases with nodules (Table 2).
Given the above results, it was noted that the most commonly detected abnormalities on CXR, such as skeletal abnormalities, were benign incidental findings that did not impact perioperative clinical management. Although the presence of tracheal deviation was the second most common abnormality, encompassing about 16% of CXR abnormalities, it was found that only 5% of these 78 patients with tracheal deviation had a difficult intubation at the time of surgery. This translates into an impact on management in 4% of the cases, i.e., 100 preoperative CXRs would need to be performed in order to alter the course of management in only four cases.
Notably, patients without a cancer diagnosis on surgical pathology were more likely to have tracheal deviation than patients with cancer. However, among patients with cancer, the incidence of tracheal deviation was higher in those with a higher T-stage. In other words, the larger the tumor, the more likely the tracheal deviation was.
One could argue that a preoperative CXR could assist in evaluating for metastases; however, it was observed that non-metastatic cancers were more likely to have CXR abnormalities than metastatic cancers. Furthermore, while evaluating the two major CXR abnormalities that would be clinically relevant in patients with malignancy, i.e., the presence of lung nodules and tracheal deviation, there was no significant difference, which makes obtaining a CXR medically futile since no added diagnostic benefit was obtained, and the practice did not change the sequence of events pertaining to the perioperative management.
In order to evaluate the utility of the variable CXR findings in predicting thyroid cancer and/or the presence of metastases, the sensitivities (Sn), specificities (Sp), positive predictive values (PPV) and negative predictive values (NPV) were calculated and are delineated in Table 3. In patients found to have tracheal deviation, the PPV for detecting thyroid cancer and metastases were 53.8 and 14.3%, respectively. The PPV for the presence of lung nodules in detecting thyroid cancer were 72.4%. Given the low sensitivity of the CXR as a tool for the detection of thyroid cancer and/or metastases, its use as a screening tool is therefore limited.
One limitation of this study is that it was performed at a single institution. As such, common practices vary among different institutions. Many large academic centers do not routinely perform preoperative CXRs on patients undergoing thyroidectomies. In fact, since we presented these data at our institution, the practice of obtaining a preoperative CXR before thyroidectomy has changed. Our aim is to provide scientific evidence to help providers who routinely care for these patients to assess whether or not obtaining a chest radiograph is necessary.
Another possible limitation of our study is the difficulty in defining difficult intubation. As per the updated report of the American Society of Anesthesiology Practice Guidelines for the management of a difficult airway, there are no set criteria that define a difficult airway. For the purpose of their guidelines, a difficult airway was defined as a clinical situation in which an anesthesiologist experiences difficulty with facemask ventilation of the upper airway or difficulty with tracheal intubation, or both [5]. This was the definition used in our study. Evaluating cases at a single medical center eliminates the possible variability in technique (related to anesthesiologists’ experience, preparation, equipment availability, positioning, etc.) all of which could affect the percentage of patients that had a difficult intubation (or lack thereof) in our study.
When deciding to order or perform any medical procedure, one must weigh the risks versus the benefits to justify the necessity of the procedure. Although obtaining a CXR is a relatively harmless procedure, it does expose the patient to a minimal amount of radiation and imposes added cost without an apparent added benefit.
Based on the data presented, the preoperative CXR is not predictive of perioperative complications. The presence of CXR abnormalities did not correlate with an increased likelihood of having thyroid cancer. The presence of tracheal deviation impacted management in 4% of cases and was associated with an increased T-stage. No unusual or unsuspected CXR findings were incidentally noted during our review, and as such, there was no apparent added therapeutic impact in obtaining a preoperative CXR.
One may therefore conclude that the utility of preoperative CXR in patients undergoing thyroidectomy including for thyroid cancer is very limited. In the climate of value-based care, routine use of this modality may be considered redundant and should be ordered only if otherwise clinically indicated.
References
Hong BW, Mazeh H, Chen H et al (2012) Routine chest X-ray prior to thyroid surgery: is it always necessary? World J Surg 36:2584. https://doi.org/10.1007/s00268-012-1720-z
Kerr IH (1974) The preoperative chest X-ray. Br J Anaesth 46(8):558–563. https://doi.org/10.1093/bja/46.8.558
Mccomb BL, Chung JH, Crabtree TD, Heitkamp DE, Iannettoni MD, Jokerst C, Saleh AG, Shah RD, Steiner RM, Mohammed TL, Ravenel JG (2016) ACR appropriateness criteria® routine chest radiography. J Thorac Imaging. https://doi.org/10.1097/rti.0000000000000200
(1979) Preoperative chest radiology. National study by the Royal College of Radiologists. Lancet 314(8133):83–86. https://doi.org/10.1016/s0140-6736(79)90131-4
Apfelbaum JL (2013) Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on management of the difficult airway. Anesthesiology 118(2):251–270. https://doi.org/10.1097/ALN.0b013e31827773b2
Acknowledgements
We thank Dr. Ahmet Bahadir Ergin for the research design.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Mikhael, A., Patell, R., Tabet, M. et al. Chest X-ray Prior to Thyroidectomy: Is It Really Needed?. World J Surg 42, 1403–1407 (2018). https://doi.org/10.1007/s00268-017-4357-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4357-0