Abstract
Background
Invasion of the upper aerodigestive tract by papillary thyroid carcinoma (PTC) affects both prognosis and quality of life. We assessed the efficacy of window resection for patients with intraluminal cricotracheal invasion.
Methods
Clinical data were retrospectively reviewed for all patients with PTC undergoing surgery at our institution during 1981–2009. Seventy-six patients with intraluminal cricotracheal invasion were enrolled, including 34 relapsing patients.
Results
The 10-year disease-specific survival rate of 42 patients with intraluminal invasion who underwent initial surgery was 60.8%. The lesion was located on the laryngo-trachea in 3 (4%) of 12 patients with locoregional recurrence. No major surgical complications were associated with cricotracheal resection. Stomal closure was achieved in 30 of 76 patients (39%). Twelve patients (16%) had a permanent stoma that was directly related to cricotracheal invasion. Their stomas had been caused by large cricotracheal defects with greater than or equal to 50% circumferential resection of the trachea. Sixty-seven patients (88%) had PTC invasion into other aerodigestive structures, including the recurrent laryngeal nerve (n = 54), esophagus (n = 38), and thyroid cartilage or intraluminal invasion of the larynx (laryngeal invasion n = 23). Multivariate analysis showed that cricotracheal invasion accompanied by recurrent laryngeal nerve invasion was predictive of permanent stoma (odds ratio 0.32; 95% CI 0.107–0.945; p = 0.039).
Conclusions
Window resection appears to be an effective treatment option for patients with intraluminal cricotracheal invasion. However, this surgical technique may be inappropriate for the treatment of large cricotracheal defects without a supportive hard structure.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Papillary thyroid carcinoma (PTC) is generally associated with an excellent prognosis. However, the rare cases in which PTC invades the upper aerodigestive tract are known to have a relatively poor prognosis and quality of life. Approximately 6% (range 3.6–22.9%) of PTC patients exhibit cricoid and/or tracheal invasion [1, 2]. Moreover, intraluminal extension occurs in 0.5–1.5% of patients with PTC [3].
Regarding the surgical management of aerodigestive invasion, the 2015 American Thyroid Association management guidelines state that surgical decision-making can be complex and should balance oncologic surgical completeness with preservation of the upper aerodigestive tract, as well as head and neck function [4]. A gross intraluminal tumor should be resected completely because incomplete resection results in a poor prognosis [5,6,7,8,9]; however, no consensus has been reached regarding the ideal type of surgical management for superficial invasion that does not involve the intraluminal surfaces of the aerodigestive tract [1, 10,11,12,13]. Thus, it is unclear whether shave excision or radical tumor resection should be adopted in such cases. Furthermore, the comparative effectiveness of window resection and circumferential resection as surgical treatments remains unknown for patients with intraluminal invasion of the cricoid-trachea [3, 14,15,16]. Thus, the surgical management of airway invasion is controversial.
At our institute, we have performed window resection and reconstructive surgery of cricotracheal defects for PTC patients with intraluminal cricotracheal invasion. Here, we aimed to assess the efficacy of this surgical method.
Materials and methods
Patients
We retrospectively reviewed the medical records of patients with PTC who were surgically treated at Kyoto Medical Center and Kusatsu General Hospital during 1981–2009. Based on our review of these records, we selected the patients who had intraluminal invasion of the cricoid-trachea with or without laryngeal invasion.
The surgical treatment for cricotracheal invasion consisted of shave excision for cases with superficial invasion and window resection for cases with intraluminal invasion (Table 1). We examined associations between window resection, prognosis, recurrence, and postoperative status in patients with intraluminal cricotracheal invasion. Prognosis and recurrence rate were compared between patients who received window resection and those who had superficial invasion of the cricoid-trachea. We also investigated postoperative airway outcomes in patients undergoing window resection.
The relevant institutional review board approved this study. The patients’ privacy was strictly maintained.
Surgical methods
Window resection was defined as resection of the cartilage, including the penetrated area of the cricotracheal lumen. Circumferential sleeve resection was defined as resection of the entire circumference of the cricoid-trachea and was adapted for massive cricotracheal infiltration.
Patients with intraluminal invasion of the cricoid-trachea underwent resection with a small surgical margin of approximately 1–2 mm. Consequently, a cricotracheal defect or tracheocutaneous fistula was formed and was not closed immediately. During surgery, multiple margin samples were examined via frozen section analysis to pathologically confirm the presence of negative margins.
The closure or reconstruction of the tracheocutaneous fistula was performed in stages. A small cricotracheal stoma was closed using a local cutaneous flap. The original deltopectoral (D-P) flap or pectoralis major musculocutaneous (PMMC) flap was used for repair in cases with large cricotracheal defects that could not be closed with a local flap, but where the remaining structure could still provide internal support. Patients who had large cricotracheal defects without sufficient internal support underwent closure using the D-P flap combined with nasal septal cartilage for hard structure reconstruction.
Some patients had large cricotracheal defects that could not be closed because of the presence of a massive cricotracheal defect, subglottic stenosis, bilateral recurrent laryngeal nerve (RLN) palsy, or continuous aspiration. In these patients, plastic surgery for cricoid-trachea defects were performed using the D-P flap alone or the D-P flap combined with nasal septal cartilage to improve phonetic function. The D-P flap is a skin flap of the deltoid and pectoral regions, based on the internal mammary vessels. The PMMC flap is a myocutaneous flap of the pectoral regions, based on the thoracoacromial vessels. These flaps are flexible and easy to make.
There are 4 parameters related to resection of the cricoid-trachea: the longitudinal resection area of the trachea, the circumferential resection region of the trachea, invasion into the membranous portion of the trachea, and cricoid cartilage invasion. The longitudinal resection area of the trachea was measured based on the number of resected tracheal rings.
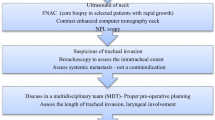
Preoperative diagnosis and postoperative follow-up
Invasion of the aerodigestive tract, including the cricoid-trachea, was evaluated via preoperative diagnostic imaging and intraoperative clinical or pathological examinations. Cervical ultrasonographic examination was routinely performed for all patients with thyroid carcinoma. Moreover, for patients with suspected cricotracheal invasion, enhanced computed tomography or magnetic resonance imaging and endoscopic examination were performed preoperatively. Intraluminal invasion of the cricoid-trachea was evaluated via endoscopic examination. Postoperative assessments were conducted at 6-month intervals to check for locoregional or distant recurrence.
Statistical analysis
Groups were compared using the Mann–Whitney U test or Chi-square test, as appropriate. A multivariate, binary logistic regression analysis was performed to examine associations between variables and the need for a permanent stoma. The logistic regression used the forward stepwise method and included the factors that showed significant associations in univariate analyses. Ten-year disease-specific survival rates were estimated using the Kaplan–Meier method and compared using the log-rank test. Commercially available software (Ekuseru-Toukei 2015; SSRI Co., Ltd., Tokyo, Japan) was used for all statistical analyses. Significance was defined as a p value <0.05.
Results
During the study period, 140 of 803 PTC patients exhibited cricotracheal invasion. In total, 64 patients (including 9 relapsing patients) had superficial invasion and 76 patients had intraluminal invasion. Of the 76 patients with intraluminal invasion, 42 were found to have cricotracheal invasion by PTC at the time of the initial diagnosis, whereas 34 were diagnosed with cricotracheal invasion by PTC during cancer relapse (Fig. 1). Sixty-one of the 76 patients (80%) were referred from other institutions for the surgical treatment of cricotracheal invasion by PTC. Among the patients with intraluminal cricotracheal invasion, the mean age at the time of surgery was 67 years (range 32–92 years). The duration of follow-up after surgery was 7.4 years (SD 6.3 years) for patients surviving the procedure (Table 2).
Of the 34 patients who had been referred to our institution because of cancer relapse in the cricoid-trachea, 6 (18%) and 5 (15%) underwent radioactive iodine treatment (RAI) and external-beam radiation therapy (EBRT) after the initial surgery, respectively. Post-surgical EBRT or chemotherapy was not indicated for the patients with cricoid-tracheal invasion. Only 1 patient received EBRT for sternal bone metastasis. Six patients (8%) underwent RAI after cricotracheal tumor resection. Only 1 patient had radioactive iodine uptake in the lung metastases; the other patients had no radioactive iodine uptake.
Ninety-seven patients received initial surgery, of whom 55 had superficial invasion and 42 had intraluminal invasion. The patients who underwent surgery for intraluminal invasion of the cricoid-trachea had a significantly lower 10-year disease-specific survival rate than did those who underwent surgery for superficial invasion of the cricoid-trachea (60.8 vs. 91.2%, p < 0.001, log-rank test, Fig. 2).
Comparison of DSS rates for patients who received initial surgery and who had superficial or intraluminal invasion of the cricoid-trachea. The solid line represents patients with superficial invasion of the cricoid-trachea (n = 55), while the dotted line represents patients with intraluminal invasion of the cricoid-trachea (n = 42). Ten-year DSS rates were estimated using the Kaplan–Meier method and compared using the log-rank test. The 10-year DSS rate was significantly in the superficial invasion group than in the intraluminal invasion group (91.2 vs. 60.8%; p < 0.001). DSS disease-specific survival
Of the 76 patients who received window resection, 12 (16%) and 19 (25%) had locoregional and distant recurrence, respectively. Of the 64 patients who received shave excision, 8 (13%) and 7 (11%) had locoregional and distant recurrence, respectively (Table 3).
Seventeen patients died of distant metastasis (n = 16) or locoregional disease (n = 1). Early postoperative death unrelated to the cricoid-tracheal resection, was noted in 4 patients (acute respiratory distress syndrome caused by respiratory insufficiency due to bilateral phrenic nerve invasion, n = 1; intestinal bleeding, n = 1; heart failure, n = 1; injury to the innominate artery following clavicular resection and mediastinal dissection, n = 1). There were no major surgical complications associated with cricotracheal resection.
Ten (13%, including 6 relapsing patients) of 76 patients with intraluminal cricotracheal invasion were diagnosed with poorly differentiated carcinoma. Of the patients with poorly differentiated carcinoma, 7 died because of distant metastasis (lung metastasis, n = 4; brain metastasis, n = 2) or early postoperative death (heart failure, n = 1). Only 2 patients had a locoregional recurrence unrelated to the cricotracheal resection area (cervical or mediastinal lymph node recurrence).
Stomal closure was achieved in 30 of 76 patients (39%), whereas permanent stoma was required in 46 patients (61%, Table 4). The need for a permanent stoma was related to bilateral RLN invasion in 13 patients, continuous aspiration associated with tumor excision without pulmonary complications in 8 patients (window resection and esophageal reconstruction for trachea-esophageal invasion, n = 5; vertical hemilaryngectomy for laryngo-tracheal invasion, n = 3), total or subtotal laryngectomy for laryngo-tracheal invasion in 5 patients, and other factors in 8 patients (early postoperative death, n = 4; age-associated decrease in swallowing function, n = 3; decrease in swallowing function due to brain metastasis, n = 1). Permanent stoma directly related to cricotracheal invasion was noted in 12 patients (16%), of whom 10 had a large cricotracheal defect with ≥50% circumferential resection of the trachea. The remaining 2 patients developed tracheal stenosis after reconstruction of the cricotracheal defect, as caused by large cricoid cartilage resection or tracheal deformity (Fig. 3).
Intraluminal cricotracheal invasion from PTC. Greater than 50% circumferential cricotracheal resection and resection of the membranous portion of the trachea were performed for intraluminal invasion of the cricoid-trachea (a, b: *). The longitudinal resection was from the cricoid cartilage to the fourth ring of the trachea. The cricotracheal defect was reconstructed using the D-P flap combined with nasal septal cartilage (c, d: **). The cricotracheal stoma was closed after the staged reconstructive surgery. The reconstructed range of the cricotracheal stoma was from the trachea cartilage beyond the midline to the membranous portion in computed tomography imaging (d: **). C Cricoid cartilage, T trachea, D-P flap deltopectoral flap
Forty-four patients (58%) required ≥50% circumferential resection of the trachea. The remaining 32 patients (42%) required <50% circumferential resection of the trachea. Circumferential sleeve resection was required in 3 (4%) of the 44 patients with ≥50% circumferential resection of the trachea. The mean longitudinal resection area of the trachea involved 6.0 and 4.3 rings in patients with ≥50% and <50% circumferential resection of the trachea, respectively; the difference was statistically significant (p = 0.001, Mann–Whitney U test). Invasion into the membranous portion of the trachea was detected in 40 patients (53%) and was significantly more common in patients with ≥50% circumferential resection of the trachea than in those with <50% circumferential resection of the trachea (31 of 44 patients vs. 9 of 32 patients, p < 0.001, Chi-square test, Table 5).
Among the 76 patients with intraluminal cricotracheal invasion, 67 (88%) had PTC invasion into other aerodigestive structures, including the RLN (n = 54), esophagus (n = 38), and thyroid cartilage or intraluminal invasion of the larynx (laryngeal invasion, n = 23) (Table 6). The mean number of invaded aerodigestive structures was 2.5 (Fig. 4).
Aerodigestive tract and cervical skin invasion from PTC (laryngo-tracheo-esophageal invasion). Laryngo-tracheal and esophageal invasion by the left thyroid carcinoma were noticed. The primary tumor had also invaded the left recurrent laryngeal nerve, vagal nerve, and cervical skin. We performed laryngeal framework resection for superficial laryngeal invasion (a, b: *), window resection from the cricoid cartilage to the sixth ring of the trachea for intraluminal invasion (a, b: **), and muscle layer resection of the esophagus for superficial invasion. The cervical skin (including surrounding muscles) was resected with the tumor, and the defect area was reconstructed by bilateral D-P flaps. A cricotracheal stoma was formed using bilateral D-P flaps (c). D-P flap deltopectoral flap
Various clinical variables were analyzed to determine their associations with permanent stoma. Univariate analyses showed significant associations between permanent stoma and longitudinal resection area of the trachea, ≥50% circumferential resection of the trachea, and cricotracheal invasion accompanied by RLN invasion (Table 7). Multivariate analysis showed that cricotracheal invasion accompanied by RLN invasion was significantly predictive of permanent stoma (odds ratio, 0.32; 95% confidence interval, 0.107–0.945; p = 0.039, Table 8).
Discussion
In the present study, we examined window resection, which achieved negative margins as confirmed via intraoperative pathological examination, and the subsequent staged reconstructive procedure for the cricotracheal defect.
The surgical method appeared to be an effective treatment option for the following reasons: First, the incidences of locoregional recurrence in the laryngo-trachea and total laryngectomy were low in patients who had cricotracheal invasion accompanied by laryngeal invasion. Second, no major surgical complications were associated with cricotracheal resection. However, this technique involved multiple surgical procedures and was difficult to perform in cases that had floppy or flat cricotracheal defects without any supportive hard structure.
There are 2 types of surgical management for intraluminal cricotracheal invasion by PTC: circumferential resection and window resection. Many reports have recommended circumferential resection for cricotracheal invasion by PTC because it allows precise determination of invasion depth and margin status, simple reconstruction of the cricotracheal defect, good functional preservation, and few surgical complications associated with full-thickness resection of the cricoid-trachea [3, 14, 15]. In articles advocating circumferential resection, window resection has been described as having no clinical role because of limitations to the extent of resection (in terms of length and circumference) and certain reconstruction problems [3]. Moreover, window resection was reported to lead to a high frequency of positive margins, as histologic examination of the circumferential spread showed that invasion on the mucosal side exceeded invasion on the adventitial side [17]. In contrast, the life-threatening operative complications associated with circumferential resection include insufficiency of the anastomosis and bleeding from large vessels [18].
A few reports have suggested window resection for cricotracheal invasion by PTC [16, 19]. Although window resection is associated with greater risks of positive margins, it reportedly yields good outcomes and a low rate of local recurrence, with survival ratios similar to those for other surgical treatments.
Our institution is a secondary referral center for the difficult problem of endoluminal invasion by PTC. Consequently, 80% of the patients in the present study were referred, and the rate of intraluminal invasion is therefore high. However, death was caused by distant metastasis in most cases, and the rate of locoregional recurrence at the laryngo-trachea was low (4%). These results were equal to or better than the results reported in several previous studies [2, 10, 12]. The rate of total laryngectomy for laryngo-tracheal invasion was lower in this study than in previous reports [14, 18].
Permanent stoma directly related to cricotracheal invasion was noted in 12 patients (16%). A large cricotracheal defect with ≥50% circumferential resection of the trachea was a major cause of permanent stoma. Accordingly, it is possible that window resection was not suitable for such large defects without a supportive hard structure. In patients with massive cricotracheal invasion, circumferential resection and end-to-end anastomosis of the trachea may be more effective for stomal closure, as compared with window resection and staged reconstruction of the tracheal stoma. Nevertheless, there are certain limits to the extent of longitudinal excision for end-to-end anastomosis of the trachea. Moreover, the probability of surgical complications increases in cases with large tracheal defects. Another major cause of permanent stoma was invasion of the surrounding organs complicating cricotracheal invasion. In particular, cricotracheal invasion accompanied by RLN invasion was frequently observed in cases with permanent stoma. Thus, to improve postoperative functional outcome, we need to develop a treatment plan that is tailored to the invasion of multiple organs, including the cricoid-trachea. In the recent guidelines, surgery for aerodigestive invasive diseases is recommended in combination with RAI and/or EBRT. However, EBRT showed limited effectiveness for gross residual disease, and RAI showed limited concentrations for extrathyroidal or extranodal extension [20, 21]. In our study, RAI or EBRT was performed as postoperative adjuvant therapy for select patients who received cricotracheal resection in recent years. RAI is not common in Japan because of limited facilities for RAI and because many Japanese persons consume large amounts of iodine. In our study, many patients did not receive RAI or EBRT because they had pathologically confirmed negative margins.
In our study, window resection achieved negative margins as confirmed via intraoperative pathological examination. Our results suggest that window resection decreases the incidence of locoregional recurrence in the aerodigestive structures and is an effective surgical method for cricotracheal invasion that is accompanied by laryngeal invasion. Hence, we believe that window resection is an effective surgical method for cricotracheal invasion.
References
Park CS, Suh KW, Min JS (1993) Cartilage-shaving procedure for the control of tracheal cartilage invasion by thyroid carcinoma. Head Neck 15:289–291
Nishida T, Nakao K, Hamaji M (1997) Differentiated thyroid carcinoma with airway invasion: indication for tracheal resection based on the extent of cancer invasion. J Thorac Cardiovasc Surg 114:84–92
Honings J, Stephen AE, Marres HA et al (2010) The management of thyroid carcinoma invading the larynx or trachea. Laryngoscope 120:682–689
Haugen BR, Alexander EK, Bible KC et al (2016) 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26:1–133
Shindo ML, Caruana SM, Kandil E et al (2014) Management of invasive well-differentiated thyroid cancer: an American Head and Neck Society consensus statement. AHNS consensus statement. Head Neck 36:1379–1390
Czaja JM, McCaffrey TV (1997) The surgical management of laryngotracheal invasion by well-differentiated papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg 123:484–490
Ishihara T, Kobayashi K, Kikuchi K (1991) Surgical treatment of advanced thyroid carcinoma invading the trachea. J Thorac Cardiovasc Surg 102:717–720
Shadmehr MB, Farzanegan R, Zangi M et al (2012) Thyroid cancers with laryngotracheal invasion. Eur J Cardiothorac Surg 41:635–640
Wada N, Nakayama H, Masudo Y et al (2006) Clinical outcome of different modes of resection in papillary thyroid carcinomas with laryngotracheal invasion. Langenbecks Arch Surg 391:545–549
Ito Y, Fukushima M, Yabuta T et al (2009) Local prognosis of patients with papillary thyroid carcinoma who were intra-operatively diagnosed as having minimal invasion of the trachea: a 17-year experience in a single institute. Asian J Surg 32:102–108
Tsukahara K, Sugitani I, Kawabata K (2009) Surgical management of tracheal shaving for papillary thyroid carcinoma with tracheal invasion. Acta Otolaryngol 129:1498–1502
McCarty TM, Kuhn JA, Williams WL Jr et al (1997) Surgical management of thyroid cancer invading the airway. Ann Surg Oncol 4:403–408
Tsai YF, Tseng YL, Wu MH et al (2005) Aggressive resection of the airway invaded by thyroid carcinoma. Br J Surg 92:1382–1387
Gaissert HA, Honings J, Grillo HC et al (2007) Segmental laryngotracheal and tracheal resection for invasive thyroid carcinoma. Ann Thorac Surg 83:1952–1959
Musholt TJ, Musholt PB, Behrend M et al (1999) Invasive differentiated thyroid carcinoma: tracheal resection and reconstruction procedures in the hands of the endocrine surgeon. Surgery 126:1078–1088
Ebihara M, Kishimoto S, Hayashi R et al (2011) Window resection of the trachea and secondary reconstruction for invasion by differentiated thyroid carcinoma. Auris Nasus Larynx 38:271–275
Ozaki O, Sugino K, Mimura T et al (1995) Surgery for patients with thyroid carcinoma invading the trachea: circumferential sleeve resection followed by end-to-end anastomosis. Surgery 117:268–271
Nakao K, Kurozumi K, Nakamura M et al (2004) Resection and reconstruction of the airway in patients with advanced thyroid cancer. World J Surg 28:1204–1206. doi:10.1007/s00268-004-7606-y
Moritani S (2015) Surgical management of cricotracheal invasion by papillary thyroid carcinoma. Ann Surg Oncol 22:4002–4007
Schwartz DL, Lobo MJ, Ang KK et al (2009) Postoperative external beam radiotherapy for differentiated thyroid cancer: outcomes and morbidity with conformal treatment. Int J Radiat Biol Phys 74(4):1083–1091
Vassilopoulou-Sellin R, Schultz PN, Haynie TP (1996) Clinical outcome of patients with papillary thyroid carcinoma who have recurrence after initial radioactive iodine therapy. Cancer 78:493–501
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Moritani, S. Window Resection for Intraluminal Cricotracheal Invasion by Papillary Thyroid Carcinoma. World J Surg 41, 1812–1819 (2017). https://doi.org/10.1007/s00268-017-3927-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-3927-5