Abstract
Background
Sublobar resection of lung cancer may benefit patients with lung cancer presenting as ground-glass opacity (GGO) nodules. The purpose of this study was to evaluate the effect of margin width on recurrence after sublobar resection in patients with clinical N0 non-small cell lung cancer presenting as GGO-predominant nodule.
Methods
We conducted a retrospective chart review of 91 patients treated for clinical N0 non-small cell lung cancer ≤3 cm by sublobar resection with clear resection margins. We assigned them to two groups: GGO-predominant tumor and solid-predominant tumor. Each group was subdivided into two groups according to the margin width: resection margin ≤5 mm and resection margin >5 mm. We analyzed the clinicopathological findings and survival among these four groups.
Results
There was no recurrence in GGO-predominant tumors after sublobar resection. Margin width did not influence the recurrence in GGO-predominant tumors. In the cases of solid-predominant tumor, 5-year recurrence-free survival after sublobar resection according to margin width ≤5 and >5 mm was 24.2 and 79.6 %, respectively (p < 0.001). Therefore, narrow margin width (resection margin ≤5 mm) was a significant risk factor for recurrence of solid-predominant tumors (hazard ratio 3.868, 95 % confidence interval 1.177–12.714, p = 0.026).
Conclusions
The width between the tumor and resection margin does not affect the recurrence after R0 sublobar resection in patients with clinical N0 GGO-predominant lung cancer ≤3 cm. By contrast, margin width is a significant risk factor for recurrence after sublobar resection in patients with clinical N0 solid-predominant lung cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer is the leading cause of cancer death in the world [1]. In many cases, early stage adenocarcinoma has been detected as ground-glass opacity (GGO) nodules. The persistent presence of GGO nodules on chest CT usually suggests the presence of lung adenocarcinoma or precancerous lesion [2]. Sublobar resection is generally preferred in lung cancer presenting as GGO nodules on chest CT, because it is considered as a non-invasive or less invasive lepidic adenocarcinoma. Many studies reported good prognosis after sublobar resection in GGO nodules [3–5]. Randomized trials to validate these conclusion are currently ongoing (JCOG 0802, JCOG 0804) [5, 6].
According to the National Comprehensive Cancer Network (NCCN) guideline for non-small cell lung cancer (NSCLC) (Version 1.2016), segmentectomy and wedge resection should achieve parenchymal resection margin ≥2 cm or greater or equal to the nodule size. Sufficient margin width is required because of the possible existence of remnant tumor cells between the tumor and the resection margin [7]. However, the effect of margin width for recurrence could be variable according to the histological type because non-small cell lung cancer includes several histological types with diverse characteristics. GGO nodules have low malignancy potential, and the possibility of cancer cells between the tumor and the resection margin could be lower than that for other types of lung cancer. This suggests that the importance of margin width may be lower for GGO nodules than for other types of lung cancer. However, there are no studies investigating the relationship between recurrence and margin width after sublobar resection in GGO lung cancer.
The use of video-assisted thoracoscopic surgery for tumor resection is increasing. Although this minimally invasive procedure has obvious advantages, sometimes narrow margin width is detected after resection because of inherent technical constraints. In the case of GGO lesions, it is difficult to detect the exact tumor boundary because the lesion is not robustly manually palpable, and this becomes more problematic in the case of deep GGO lesions. Narrow margin width sometimes is detected after sublobar resection of GGO lesions. It is questionable whether additional margin resection is necessary in those cases, especially when no cancer cells are identified in the cut margins of intraoperative frozen sections.
The purpose of this study was to evaluate whether narrow margin width is related to recurrence after sublobar resection of non-small cell lung cancer presenting as GGO-predominant nodules ≤3 cm, and to compare the effects of margin width on recurrence in GGO-predominant and solid-predominant tumors.
Materials and methods
Patients
From January 2004 to December 2013, 958 consecutive patients at Seoul St. Mary’s Hospital in Korea were diagnosed with NSCLC and underwent surgical resection. Of this population, 484 patients had tumors ≤3 cm that were staged as clinical N0, and 104 patients underwent sublobar resection. Patients who underwent incomplete resection were excluded. No patients included in the study received preoperative chemotherapy or radiotherapy. Complete resection was defined as an absence of both macroscopic and microscopic residual cancer, especially in the resection margin. The study retrospectively enrolled 91 patients and assigned them to two groups according to the radiological features: GGO-predominant tumor and solid-predominant tumor. Each group was further subdivided into two groups according to the resection margin width: resection margin ≤5 mm and resection margin >5 mm. Clinicopathological features and survival were compared among these four groups: Group A, GGO-predominant tumor and resection margin ≤5 mm; Group B, GGO-predominant tumor and resection margin >5 mm; Group C, solid-predominant tumor and resection margin ≤5 mm; Group D, solid-predominant tumor and resection margin >5 mm. The elective surgical procedure for GGO-predominant tumor was sublobar resection because of the strong probability for good postoperative prognosis. Sublobar resection of solid-predominant tumor was only performed for high-risk patients (e.g., old age or cardiopulmonary disease). None of the GGO tumors were pathologically confirmed preoperatively. Preoperative biopsy was performed only for solid-predominant tumor. This study was approved by the Institutional Review Board of Seoul St. Mary’s Hospital at the Catholic University of Korea.
Radiological evaluation and preoperative staging
Clinical staging was determined by contrast-enhanced chest CT and F-18-fluorodeoxyglucose (FDG)-positron emission tomography (PET)/CT scanning within 1 month before surgery. Primary lesions were evaluated using thin-section CT images. CT scans were obtained at full inspiration. GGO is defined on a CT scan by increased hazy opacities in lung parenchyma with preservation of bronchial structures and vascular margins [8]. The tumor diameter was defined as the largest axial diameter of the lesion on the lung window setting. The consolidation was defined as an area of increased opacification, which completely obscured underlying bronchial structures and vascular markings, and the diameter of consolidation area on the axial image of the lung window setting also was measured. Tumors that had a value of <0.5 for the ratio of the consolidation diameter to the tumor diameter were defined as GGO-predominant tumor, whereas tumors with a ratio ≥0.5 were defined as solid-predominant tumor. Each lung nodule on preoperative CT scans was reviewed blindly by two thoracic surgeons.
Histological evaluation
All clinical specimens were examined by pathology specialists whose observations were recorded. The free resection margin width was defined as the nearest length between the tumor and the resection line. The gross cut-surface margin distance was measured [9]. These data were recorded on final histological examination reports. In the cases of adenocarcinoma, histomorphological patterns (lepidic, acinar, papillary, micropapillary, and solid) were described according to the 2015 World Health Organization (WHO) classification of lung tumors [10]. Adenocarcinoma in situ (AIS) and minimally invasive adenocarcinoma (MIA) were defined as small (≤3 cm) and solitary adenocarcinomas that exhibited lepidic growth pattern without invasion (AIS) or with ≤5 mm invasion (MIA).
Statistical analysis
Clinicopathological factors of each of the four groups were compared. Student’s t test or the Wilcoxon rank-sum test was used for two groups of continuous variables, and the χ 2 test or Fisher’s exact test was applied for categorical variables. Follow-up data for the interval between surgical resection and last follow-up visit were analyzed, and confirmed recurrence/death was used to calculate recurrence-free survival (RFS) using the Kaplan–Meier method. Survival of each group was compared using the log-rank test, and the Cox proportional hazards model of multivariate analysis was used to determine risk of recurrence. A value of p < 0.05 was considered statistically significant.
Results
A total of 91 patients were retrospectively enrolled in this study; of these, 52 patients had GGO-predominant tumor and 39 patients had solid-predominant tumor. Clinical characteristics of GGO-predominant tumors were compared in Group A (n = 14) and Group B (n = 38), and clinical characteristics of solid-predominant tumors were compared in Group C (n = 11) and Group D (n = 28) (Table 1). All tumors were located peripherally. There were no differences between Groups A and B with respect to age, gender, smoking status, involved lobes, serum carcinoembryonic antigen (CEA) level, maximum standardized uptake value (SUVmax) of FDG on PET/CT scanning, and clinical TNM stage. Although the incidence of wedge resection tended to be higher in Group A, this was not statistically significant (p = 0.061). The incidence of postoperative complication was not statistically significant between Groups A and B (0 vs. 7.9 %, p = 0.279). There was no postoperative mortality in Groups A and B.
The comparison between Groups C and D showed that there were no significant differences in any of the clinical factors except for the incidence of VATS, which was 36.4 % in Group C and 85.7 % in Group D (p = 0.002). The incidence of postoperative complication in Groups C and D were 18.2 and 10.7 %, respectively (p = 0.530). There was no postoperative mortality in Groups C and D. Postoperative complication occurred in 8 of the 91 total patients (8.8 %); 6 patients had prolonged air leak (>7 days), 1 patient had paroxysmal atrial flutter, and 1 patient had pulmonary edema. All patients with postoperative complication recovered without any problems after transfer to conservative care. We also compared clinical characteristics between GGO-predominant tumor (Groups A and B) and solid-predominant tumor (Groups C and D). Solid-predominant tumor was associated with older age, male gender, higher serum CEA level, higher SUVmax, and more advanced TNM clinical stage than that of GGO-predominant tumor.
Pathological characteristics were compared among the four groups (Table 2). For Groups A and Group B, tumor size was not significantly different. The mean margin widths in Groups A and B were 3.7 and 21.3 mm, respectively. All tumors of Groups A and B were adenocarcinomas. The degree of tumor differentiation was similar in Groups A and B. The incidence of AIS or MIA was higher in Group B (27 patients, 71.1 %) than in Group A (6 patients, 42.9 %), but this difference was not statistically significant (p = 0.061). In Group A, eight patients displayed invasive adenocarcinoma; four patients had lepidic adenocarcinoma, three patients had acinar adenocarcinoma, and one patient had papillary adenocarcinoma. In Group B, 11 patients displayed invasive adenocarcinoma; 4 patients had acinar adenocarcinoma, 4 patients had papillary adenocarcinoma, and 3 patients had lepidic adenocarcinoma. There were no statistically significant differences between Groups A and B with respect to the distribution of pathological stage and the incidence of visceral pleural invasion, lymphatic invasion, and vascular invasion. Comparisons of Groups C and D for tumor size, histology distribution, tumor differentiation, pathological stage, and the incidence of pleural invasion, lymphatic invasion, and vascular invasion did not identify any statistically significant differences. Groups C and D included adenocarcinoma, squamous cell carcinoma, and other types of non-small cell lung cancer (two patients had adenosquamous cell carcinoma, and 1 patient had large cell neuroendocrine carcinoma).
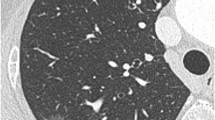
Median follow-up time for all patients was 974 days (range 98–2485 days), and recurrence was recorded in 13 patients. The 5-year RFS rate in Groups A and B was 100 %. However, the 5-year RFS rate in Group C was significantly lower than that in Group D, 24.2 versus 79.6 %, respectively (p < 0.001) (Fig. 1). Recurrence only occurred in patients with solid-predominant tumor. The recurrence patterns of Groups C and D were analyzed. For Group C recurrence, 7 cases were locoregional recurrence, and only 1 case was locoregional recurrence combined with distant recurrence; of these cases, resection site recurrence occurred in 4 cases (50 %). For Group D, 5 patients had recurrence; (locoregional recurrences were 4 cases, locoregional and distant recurrence was 1 case). And, resection site recurrences were 2 cases (40 %) in Group D.
Sublobar resection of GGO-predominant tumor did not lead to any cases of recurrence regardless of the margin width. We performed univariate and multivariate analysis using the Cox proportional hazards model to determine factors associated with recurrence of solid-predominant tumor (Table 3). In multivariate analysis, only margin width ≤5 mm was a significant risk factor for recurrence of solid-predominant tumor (hazard ratio 3.868, 95 % confidence interval 1.177–12.714, p = 0.026).
Discussion
NCCN guidelines for non-small cell lung cancers recommend sufficient margin width when sublobar resection (wedge resection and segmentectomy) is necessary. However, the necessary margin width for sublobar resection of GGO-predominant tumor has not been conclusively established because GGO-predominant tumor has lower malignancy than other non-small cell lung cancers. The effect of margin width on recurrence may be lower for GGO tumor than solid tumor because GGO tumor has lower malignancy potential. In the JCOG 0804/WJOG4507L protocol, which evaluates the effect of sublobar resection in early lung cancer (GGO tumor), the minimum required margin distance was 5 mm. Therefore, we choose a 5-mm margin to establish an additional subgroup. In this study, 5-year RFS after sublobar resection of GGO-predominant tumors was 100 % regardless of margin width ≤5 or >5 mm. Furthermore, there was no recurrence within 1550 days of a GGO-predominant tumor after wedge resection even though the margin width was only 1 mm.
All GGO-predominant tumors have the similar radiological features and patterns, which are detected as a consolidation area wrapped by a GGO area. Microscopic examinations also reveal that the invasive component was wrapped by a lepidic growth pattern. These results can explain why the margin width was not a critical factor for recurrence in GGO-predominant tumor, because the non-invasive component (lepidic growth pattern) wrapped the invasive component and thereby reduced the invasion of adjacent tissue. Accordingly, the probability of cancer cells in the margins around the tumor is very low. These factors may enable the success of complete resection for GGO-predominant tumor regardless of resection margin width.
Some studies reported that resection of contained tumors with micropapillary and solid growth patterns led to recurrence of mixed GGO tumor [11–14]. In the current study, most GGO-predominant tumors were classified as AIS, MIA, or lepidic adenocarcinoma, and micropapillary and solid growth patterns were not observed in GGO-predominant tumor. And, acinar adenocarcinoma or papillary adenocarcinoma presented as GGO-predominant tumors in 12 cases. Some studies reported that acinar and papillary growth patterns could present as GGO on radiological images [15–19]. Acinar and papillary patterns suggest lower potential for malignancy than those of micropapillary and solid patterns [5, 20]. Several studies reported that adenocarcinoma presenting as GGO had good prognosis regardless of histomorphological features [3, 15, 17, 21]. These combined results suggest that there was no recurrence of GGO-predominant tumor, even though all GGO-predominant tumors were not AIS or MIA.
A comparison of clinicopathological characteristics between Groups C and D showed that there were no statistically significant differences except for the incidence of open thoracotomy. The incidence of open thoracotomy was higher in Group C than in Group D. Essentially all lesions in Group C were located deeper than those in Group D. The incidence of pleural adhesion in Group C also was higher than in Group D. For these reasons, open thoracotomy was performed more frequently than VATS for patients in Group C, and the margin width would be narrower due to technical difficulties. However, differences in the surgical procedures used (VATS versus open thoracotomy) might not affect prognosis because the clinicopathological and tumor characteristics were not significantly different between Groups C and D. The results in this study indicate that margin width was an important factor for recurrence in solid-predominant tumor after sublobar resection because the 5-year RFS differed between Groups C and D, and margin distance was a significant risk factor for recurrence in multivariate analysis. Local recurrence was detected in 8 of 11 patients (72.7 %) who had margin widths of ≤5 mm. Although all specimens had microscopically clear resection margins, local recurrence occurred in solid-predominant tumors with narrow margin widths. This local recurrence may be caused by undetected cancer cells remaining from the resected tumor mass. Therefore, it is critical that sufficient margin width is resected according to the NCCN guideline for solid-predominant tumor. If it is possible, lobectomy is recommended rather than sublobar resection for solid-predominant tumor.
The surgical indications of GGO-predominant and solid-predominant nodules were different. For GGO-predominant tumors, most patients underwent elective sublobar resection because of the strong probability of good postoperative prognosis. When considering sublobar resection, we choose wedge resection or segmentectomy according to the nodule depth from the lung surface. In other words, the choice of sublobar resection depended on the feasibility of obtaining adequate resection margin. Sublobar resection also was performed for high-risk patients (e.g., old age or cardiopulmonary disease) with solid-predominant tumors. Therefore, a comparison of prognosis after sublobar resection of GGO-predominant and solid-predominant tumors was meaningless. However, a comparison of the relationship between margin width and disease recurrence between GGO-predominant and solid-predominant tumors was meaningful, and this also was compared with RFS because overall survival did not reflect prognosis due to comorbidities of solid-predominant tumor. Disease-specific prognosis reflects cancer-related RFS better than overall survival. Overall survival also is a poor gauge of prognosis for comparisons of stage I disease because deaths are less likely to be a direct result of cancer [5]. For this study, a comparison of cancer-specific prognosis with respect to resection margin width was our aim, by examining overall RFS and RFS at clinical stage I.
A number of study limitations are acknowledged. First, this was a retrospective review conducted at a single center. Second, we obtained the data from a single institution, and the number of cases was relatively small. Furthermore, we did not compare the effects of margin in wedge resection and segmentectomy due to the small number of cases. However, resection margin width is equally important in both segmentectomy and wedge resection according to the NCCN guideline, and the segmental plane is not anatomically different from the lobectomy plane (fissure). Therefore, we considered that the margin effect would not significantly differ for wedge resection and segmentectomy. Future multicenter studies with larger patient cohorts may remedy this problem. Third, the surgical indications of sublobar resection were not the same for GGO-predominant and solid-predominant tumors. However, the comparison of the relationship between recurrence and margin width was meaningful regardless of surgical indication, because the analysis was performed in each group. More accurate results could be achieved from homogenous samples. Fourth, the accuracy of cN0 staging determinations may have benefited from invasive diagnostics in addition to imaging studies. However, invasive LN staging very rarely yields positive results in instances of cN0 tumors found on chest CT and PET/CT scans, and given the high cost and related risks, it is generally performed only if nodal metastasis is suspected [22]. Therefore, at our institution, surgical treatment was performed initially for patients diagnosed with cN0 tumors by chest CT and PET/CT scanning.
In conclusion, the distance between the tumor boundary and the resection margin does not have a significant effect on disease recurrence after sublobar resection when R0 resection is achieved in patients with clinical N0 GGO-predominant lung cancer of ≤3 cm. By contrast, margin width is a significant risk factor for disease recurrence after sublobar resection in patients with clinical N0 solid-predominant lung cancer. Further studies that include data from larger homogenous cohorts may validate these conclusions and provide more refined results.
References
Torre LA, Siegel RL, Jemal A (2016) Lung cancer statistics. Adv Exp Med Biol 893:1–19
Kim HY, Shim YM, Lee KS et al (2007) Persistent pulmonary nodular ground-glass opacity at thin-section CT: histopathologic comparisons. Radiology 245:267–275
Yoshida J, Nagai K, Yokose T et al (2005) Limited resection trial for pulmonary ground-glass opacity nodules: fifty-case experience. J Thorac Cardiovasc Surg 129:991–996
Cho JH, Choi YS, Kim J et al (2015) Long-term outcomes of wedge resection for pulmonary ground-glass opacity nodules. Ann Thorac Surg 99:218–222
Eguchi T, Kadota K, Park BJ et al (2014) The new IASLC–ATS–ERS lung adenocarcinoma classification: what the Surgeon Should Know. Semin Thorac Cardiovasc Surg 26:210–222
Nakamura K, Saji H, Nakajima R et al (2010) A phase III randomized trial of lobectomy versus limited resection for small-sized peripheral non-small cell lung cancer (JCOG0802/WJOG4607L). Jpn J Clin Oncol 40:271–274
Sawabata N, Ohta M, Matsumura A et al (2004) Optimal distance of malignant negative margin in excision of nonsmall cell lung cancer: a multicenter prospective study. Ann Thorac Surg 77:415–420
Hansell DM, Bankier AA, MacMahon H et al (2008) Fleischner Society: glossary of terms for thoracic imaging. Radiology 246:697–722
Goldstein NS, Ferkowicz M, Kestin L et al (2003) Wedge resection margin distances and residual adenocarcinoma in lobectomy specimens. Am J Clin Pathol 120:720–724
Travis WD, Brambilla E, Nicholson AG et al (2015) The 2015 world health organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol 10:1243–1260
Nitadori J, Bograd AJ, Kadota K et al (2013) Impact of micropapillary histologic subtype in selecting limited resection vs lobectomy for lung adenocarcinoma of 2 cm or smaller. J Natl Cancer Inst 105:1212–1220
Zhang Y, Wang R, Cai D et al (2014) A comprehensive investigation of molecular features and prognosis of lung adenocarcinoma with micropapillary component. J Thorac Oncol 9:1772–1778
Yanagawa N, Shiono S, Abiko M et al (2014) The correlation of the International Association for the Study of Lung Cancer (IASLC)/American Thoracic Society (ATS)/European Respiratory Society (ERS) classification with prognosis and EGFR mutation in lung adenocarcinoma. Ann Thorac Surg 98:453–458
Zhang J, Liang Z, Gao J et al (2011) Pulmonary adenocarcinoma with a micropapillary pattern: a clinicopathological, immunophenotypic and molecular analysis. Histopathology 59:1204–1214
Wilshire CL, Louie BE, Manning KA et al (2015) Radiologic evaluation of small lepidic adenocarcinomas to guide decision making in surgical resection. Ann Thorac Surg 100:979–988
Cho H, Lee HY, Kim J et al (2015) Pure ground glass nodular adenocarcinomas: are preoperative positron emission tomography/computed tomography and brain magnetic resonance imaging useful or necessary? J Thorac Cardiovasc Surg 150:514–520
Duann CW, Hung JJ, Hsu PK et al (2013) Surgical outcomes in lung cancer presenting as ground-glass opacities of 3 cm or less: a review of 5 years’ experience. J Chin Med Assoc 76:693–697
Sim HJ, Choi SH, Chae EJ et al (2014) Surgical management of pulmonary adenocarcinoma presenting as a pure ground-glass nodule. Eur J Cardiothorac Surg 46:632–636 (discussion 636)
Lim HJ, Ahn S, Lee KS et al (2013) Persistent pure ground-glass opacity lung nodules ≥10 mm in diameter at CT scan: histopathologic comparisons and prognostic implications. Chest 144:1291–1299
Sasada S, Nakayama H, Miyata Y et al (2015) Comparison of malignant grade between pure and partially invasive types of early lung adenocarcinoma. Ann Thorac Surg 99:956–960
Suzuki K, Kusumoto M, Watanabe S et al (2006) Radiologic classification of small adenocarcinoma of the lung: radiologic–pathologic correlation and its prognostic impact. Ann Thorac Surg 81:413–419
Kirmani BH, Rintoul RC, Win T et al (2013) Stage migration: results of lymph node dissection in the era of modern imaging and invasive staging for lung cancer. Eur J Cardiothorac Surg 43:104–109 (discussion 109–110)
Acknowledgments
This research was not supported by outside funds.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Moon, Y., Lee, K.Y., Moon, S.W. et al. Sublobar Resection Margin Width Does Not Affect Recurrence of Clinical N0 Non-small Cell Lung Cancer Presenting as GGO-Predominant Nodule of 3 cm or Less. World J Surg 41, 472–479 (2017). https://doi.org/10.1007/s00268-016-3743-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3743-3