Abstract
Background
The main limiting factor for major liver resections is the volume and function of the future remnant liver (FLR). Portal vein embolization (PVE) is now standard in most centers for preoperative hypertrophy of FLR. However, it has a failure rate of about 20–30 %. In these cases, the “Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy” (ALPPS) may represent a suitable and possibly the only alternative.
Methods
We performed a retrospective analysis of nine patients who had ALPPS following an insufficient hypertrophy after PVE. Computed tomography volumetry were performed before and after PVE as well as the first step of ALPPS. Furthermore, complications, 30-day mortality and outcome were analyzed.
Results
The FLR volume rose significantly by 77.7 ± 40.7 % (FLR/TLV: 34.9 ± 9.7 %) as early as 9 days after the first stage despite insufficient hypertrophy after preoperative portal vein embolization. Major complications (Grade > IIIb) occurred in 33 % of the patients, and 30-day mortality was 11.1 %. The OS at 1 and 2 years was 78 and 44 %. Four patients are presently still alive at a median of 33.4 (range 15–48) months (survival rate 44.4 %).
Conclusion
The ALPPS procedure could be a suitable alternative for patients following insufficient PVE or indeed the last chance of a potentially curative treatment in this situation. Nevertheless, the high morbidity and mortality rates and the lack of data on the long-term oncological outcome must also be taken into account.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical resection is generally the only option for the curative treatment of primary and secondary hepatic malignancies [1]. However, its chance of success is limited by the anatomical location of space-occupying lesions, by the patient’s general condition and—particularly in case of major resections—by the size and function of the future liver remnant [2]. In order to increase the proportion of resectable patients, various strategies have been developed. On the one hand, neoadjuvant therapy concepts are able to reduce the size of the tumor (“downsizing”) [3], while preoperative portal vein embolization [4, 5], two-stage liver resections [6] or a combination of both [7] can increase the size of the postoperative future liver remnant (FLR).
Portal vein embolization (PVE), which is now a standard procedure in most centers, is successfully and effectively performed with low morbidity and mortality rates [8]. Despite good results, it has a failure rate of about 20–30 % due to technical failure, anatomical variations and insufficient hypertrophy [8, 9].
Whenever hypertrophy of the future remnant liver is insufficient after PVE, the “Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy” (ALPPS) may represent a suitable alternative [10, 11]. In order to evaluate this hypothesis, patients with an ALPPS procedure following an unsuccessful PVE were analyzed.
Patients and methods
Patients
All patients who underwent PVE prior to liver resection were identified retrospectively from a prospective institutional database. The decision to do an ALPPS procedure was made if preoperative computer tomography (CT) liver volumetry revealed an insufficient FLR volume after PVE (FLR/total liver volume (TLV) <25 % in patients with normal liver or <30 % with cholestasis or chemotherapy-associated hepatopathy) [12, 13]. Apart from that, in some cases the decision to perform an ALPPS procedure was made intraoperatively—even if the CT volumetry yielded a sufficient FLR volumetric. This decision was based on the surgeon’s subjective assessment and his experience with regard to the macroscopically identifiable remnant liver volume and the quality of the parenchyma as well as the corresponding laboratory values and the patient’s general condition. Extrahepatic metastases or a patient’s poor clinical status (ECOG ≥ 3) was considered contraindications for an ALPPS procedure.
Liver volumetry
A contrast-enhanced abdominal CT was performed in all patients prior to PVE, and before the first and second stage of the ALPPS procedure. Total liver volume (TLV) and future liver remnant (FLR) were calculated for each patient and stage of treatment using the program OsiriX, an advanced open-source picture archiving and communication system (PACS) and digital imaging and communications in medicine viewer (DICOM) viewer [14]. The percentage increase in FLR volume was calculated after each step in percent (%FLR) as follows: [(FLR post-intervention − FLR pre-intervention)/FLR pre-intervention] × 100. We also calculated the difference between the individual FLRs and the ratio between future liver remnant volume and total liver volume ratio (FLR/TLV), as well as the daily increase in volume (kinematic growth rate, KGR) as median increase in volume per day (ml per day and % per day). To standardize kinetic growth, a mean volume increase per day was calculated assuming a linear growth model.
Laboratory parameters
Blood samples were taken on POD 1 and 5 after step I and POD 1, 5 and 10 after step II of the ALPPS procedure. Samples were analyzed for bilirubin, creatinine, GOT, GPT, prothrombin time and albumin levels.
Portal vein embolization (PVE)
CT-guided access to the portal venous system was gained via an ipsilateral approach. After successfully puncturing a right portal vein branch, a guidewire was placed into the superior mesenteric vein. Embolization of the right portal vein branches (5–8) was performed with a mixture (1:2–1:3) of n-butyl-cyanoacrylate (Braun, Tuttlingen, Germany) and lipiodol (Guerbet, Roissy, France). Successful embolization was documented by repeated portography.
Surgical procedure
The technical aspects of ALPPS have been described in detail [10, 15]. In sum, the ALPPS procedure is a two-stage hepatectomy with an interval of 7–14 days between stages. In addition to a potential FLR cleanup, a complete parenchymal transection and right portal vein ligature of the liver lobe to be removed are performed during the first stage (ALPPS1). The bile duct, the right hepatic vein and the hepatic artery are left undisturbed. In the present study, in two patients with cholangiocarcinoma the bile duct bifurcation was resected and a biliodigestive anastomosis was performed in the first step.
Depending on the increase in FLR volume and the patient’s clinical condition, the bile duct, the right hepatic artery and the right hepatic vein were dissected during the second stage of the ALPPS procedure (ALPPS2).
Complications and outcome
Postoperative adverse events were evaluated according to the Dindo-Clavien [16] classification of surgical complications. Major complications were defined as Grade ≥ IIIa complications. Mortality was recorded when death occurred during hospital stay or during the 90-day follow-up period. The “50–50” criteria were used to define postoperative liver failure [17]. Each patient was followed up with routine laboratory tests, tumor markers and imaging evaluation (CT scan or MRI) for 1 month and every 3–6 months after surgery. Overall survival (OS) was defined from the date of the second stage (ALPPS2) until death. Disease-free-survival (DFS) was determined as the time from the second surgical procedure (ALPPS2) until the first recorded evidence of recurrence at any anatomical site. Postoperative deaths were excluded from OS and DFS analyses.
Statistics
The distribution of variables was analyzed using the Kolmogorov–Smirnov test. Continuous data are presented as mean and standard deviation (SD). In case of normal distribution, statistical differences between groups were determined by one-way ANOVA, followed by the paired Student’s t test to compare the FLR volume after PVE and ALPPS1. In case of non-normal data distribution, a Mann–Whitney U test was used to compare two groups. p < 0.05 was considered statistically significant. Statistical analysis and graphical representations including Kaplan–Maier survival were carried out using the Statistical Package for Social Sciences (SPSS®, version 27, Chicago, IL, USA) or GraphPad Prism® (version 5.0, La Jolla, CA, USA), respectively.
Results
Patient demographics
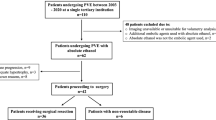
A total of 733 liver resections, of which 89 had portal vein embolization (PVE), were performed at our hospital between July 2011 and April 2015. During this period, 22 patients underwent the ALPPS procedure. Of those patients, a total of nine (5 males, 4 females) had insufficient volume growth of the FLR after preoperative PVE. Patients’ characteristics are provided in Table 1.
In all patients, tumors were localized to the right lobe and the central sector of the liver, with additional spreads in segments II and III in three patients. They were subjected to a laparoscopic resection (cleanup) as a first step. Five patients with CRM and one patient with hepatic metastases from hypopharynx cancer underwent preoperative chemotherapy. The timespan between the end of chemotherapy and surgery was at least 6 weeks in all patients. Postoperative histology revealed mild cirrhosis in two patients. All other patients had no liver pathology besides the carcinoma.
In all patients, both stages of the ALPPS procedure could be completed and an R0-resection was achieved. Time intervals between the procedures, incision-to-suture time and blood transfusions are provided in Table 2.
Volumetry
The FLR volume increased by 87 ± 56 ml following PVE corresponding to a percentage increase of 31 ± 20 % after a median of 27 days (Table 3; Figs. 1, 2). This was statistically significant when compared to the initial volume, although the FLR/TLV ratio was below the targeted value of 0.3 in seven of nine patients. In two patients, the ratio was slightly higher. However, after considering the laboratory findings and intraoperative assessment of liver parenchyma, an ALPPS procedure was performed.
Individual increase in future liver remnant (FLR) in nine patients after portal vein embolization (PVE) and before step 1 and 2 of the Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy (ALPPS1 and ALPPS2). Of note is the remarkable hypertrophy after the first step of the ALPPS following insufficient PVE
Representative CT scans (portal venous phase) at different time points (preoperative, after PVE and ALPPS, respectively) showing an ALPPS procedure in insufficient hypertrophy after portal vein embolization (PVE). Future liver remnant (FLR) is marked. PVE: portal vein; ALPPS1 and ALPPS2: step 1 and 2 of the Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy
After the first stage of the ALPPS procedure, the mean increase in volume (Δ-volume) was 239 ± 90 ml, corresponding to a percentage increase of 77.7 ± 40.7 % and a FLR/TLV ratio of 34.9 %. This increase in volume was already observed after a median of 9 days (range 6–14) and was significantly higher (p = 0.002) and more rapid (p = 0.039) than the increase after PVE.
Similar results were also observed when evaluating the growth rate per day (KGR). After the first stage, the increases in volume were significantly higher than the values following PVE (p = 0.004).
The volume growth in patients with PVE and a short interval of <22 days did not differ significantly from that in patients with a long interval (Δ-FLR/TLV: 52.79 ± 39.2 % vs. Δ-FLR/TLV: 41.28 ± 33.31 %; p = 0.26).
Laboratory parameters
No significant changes in any of the examined laboratory parameters were observed following PVE. The laboratory values (50–50 criteria) after ALPPS did not provide any evidence of severe postoperative liver function disorder. We merely observed a slight increase in bilirubin level and a drop of prothrombin time after the in situ split (ALPPS1), which was more pronounced after the second stage (ALPPS2), but stabilized again over time (values are shown in Table 4). The increase in alanine transaminase (ALT) and the drop in albumin were likewise more pronounced after the second stage than after ALPPS1, normalizing again in almost all patients after a period of 10 days. Creatinine values showed no abnormalities. Postoperative renal failure was not observed.
Chemotherapy
Six of nine patients (66.6 %) underwent neoadjuvant chemotherapy up to 6 weeks before the procedure (Table 1). Patients, who had been undergoing neoadjuvant chemotherapy, showed a liver volume growth (mean Δ-volume) of 109 ± 47.3 ml following PVE, with a volume growth of 247 ± 110 ml after the first ALPPS stage. The volume growth without chemotherapy after PVE was 121 ± 45.8 and 223 ± 111 ml after ALPPS1 (p = 0.11 and p = 0.66). Likewise, in comparison with the FLR/TLV ratio and the linear growth rate, there were no significantly lower values in the group with neoadjuvant chemotherapy.
Clinical outcomes and complications
The median follow-up period was 18.5 (range 1–48) months. Severe complications (>IIIa) occurred in five (56 %) of a total of nine patients. Three patients experienced a biliary leakage after the second procedure, which had to be treated by percutaneous transhepatic cholangiography and drainage. The drainages could be gradually removed under irrigation with saline solution after 4 weeks at the latest, and the patients discharged free of symptoms.
Perioperative mortality (in hospital) was 11.1 % (one of nine patients). This patient suffered from Bechterew disease and acquired a severe respiratory infection leading to uncontrollable septic complications and finally multiorgan failure and death 25 days after surgery.
Contrast-enhanced cross-sectional imaging revealed hepatic recurrences in 6/9 patients during follow-up. In three patients, tumor recurrence was treated by local liver resection. In two of these patients, additional extrahepatic metastases and hepatic re-recurrences were found. However, both are still alive following chemotherapy treatment and selective internal radiation therapy (SIRT). Overall, the OS at 1 and 2 years was 78 and 44 %, whereas the DFS rates were 50 and 13 %, respectively. Four patients are presently still alive at a median of 33.4 (range 15–47) months (survival rate 44.4 %).
Discussion
Our analysis of nine patients showed a high hypertrophy rate after ALPPS despite a previously insufficient hypertrophy after PVE. FLR volume rose significantly by 77.7 % as early as 9 days after the first stage of the ALPPS procedure, thus enabling the second stage of the procedure in all patients. Previous chemotherapy did not seem to have a negative impact on the hypertrophy rate. Major complications (Grade > IIIa) occurred in 56 % of the patients. One patient died postoperatively due to sepsis following a respiratory infection. Four patients are presently still alive at a median of 33.4 (range 15–47) months (survival rate 44.4 %).
Preoperative portal vein embolization (PVE) in humans was first described by Kinoshita et al. [18]. After that, numerous reports were able to confirm the efficient hypertrophy of the FLR after PVE with low morbidity and mortality rates [5, 19]. Hitherto untreatable patients could now undergo surgery—also in combination with two-stage hepatectomies [2, 20]. In a recently published review with 1791 patients [8], the increase in FLR volume following embolization was 37.9 %. According to our assessment, this figure is realistic, even though there is evidence that improved growth rates can be achieved following the additive embolization of segment IV or the hepatic artery [21, 22]. Nevertheless, in our opinion the PVE has three limitations. To start with, the procedure is sometimes not possible or too risky because of technical difficulties and/or anatomical variations or due to vascular infiltration of the tumor. Secondly, relevant tumor progression may occur during the waiting time for sufficient hypertrophy [8]. This could have the effect of rendering a curative resection impossible [15, 23]. However, some authors do not actually consider this a limitation, but rather perceive it as an oncological selection of suitable patients [24, 25]. Of note, there might be evidence of direct stimulation of tumor growth by PVE [26, 27].
The third and final limitation, as seen in our patients, is the fact that PVE may not stimulate FLR hypertrophy sufficiently for major liver resections [28, 29]. To this day, the causes have not yet been conclusively explained. The presence of collaterals of the portal vein between the liver lobes or a recanalization of the embolized portal vein has been suggested as causes. This could be an explanation for our findings that longer waiting periods seem ineffective. On the other hand, the stimulus for hypertrophy and the related volume growth might decrease after a few days. Altogether 20–40 % of patients are irresectable after PVE as a result of the three above-stated limitations [29, 30].
In many of these cases, the ALPPS procedure with its inherently high hypertrophy rates in a short time may represent a suitable, and possibly the only, alternative for the patients concerned. The procedure was first performed by Schlitt et al. 2007 [10]. The multicenter study reported a median volume increase of 74 % within 9 days in 25 patients. During the last 3 years, these values were either verified or surpassed in numerous publications [31–33].
Besides marked and fast hypertrophy of the FLR, the affected part of the liver left in situ, also described as “auxiliary liver,” is able to temporarily support the function of the smaller FLR, thus avoiding postoperative liver failure [31]. This is supported by the observation that liver failure only occured after the second stage (ALPPS2), i.e., following the final resection of the “auxiliary liver” [30]. Furthermore, the oncological outcome could also be improved by early initiation or shorter pauses of chemotherapy due to rapid hypertrophy in connection with the ALPPS procedure compared to two-stage hepatectomies [34].
The underlying mechanism of ALPPS responsible for inducing accelerated hypertrophy of the liver remnant still needs to be explored. Nevertheless, we and Truant et al. [35] found efficient volume growth even after failed PVE. In contrast to our study, the subgroup analysis of the multicenter study [35] does not provide any detailed information on the volume before and after embolization nor on the clinical course or on the short- and long-term outcome of these patients.
However, since both were able to observe high growth rates even after unsuccessful PVE, other elements besides redistribution of the portal vein blood flow and hepatotrophic factors to the FLR may be involved. Animal trials provided evidence that a systemic inflammatory-like reaction triggered by the parenchymal transection of the liver or even with simultaneously induced thermal damage of the spleen or lung can stimulate hypertrophy in the future liver remnant beyond a PVE [36].
After the initial enthuisiasm over the ALPPS procedure, particularly in the initial phase, there has recently been a growing body of critical opinion [24, 37, 38], focussing on the published high morbidity (50–90 %) and mortality (0–29 %) rates [10, 29, 33, 39]. These figures partly correspond to our own results. Our relatively high morbidity rate can be partially attributed to the inhomogeneous, older patient cohort. An analysis of the ALPPS Register by Schadde et al. [39] determined that an age of >60 years and non-CRM conditions were risk factors for severe complications. This could also be an explanation for the published, slightly lower morbidity (49–59 %) and mortality rates (6.4–19 %) in two-stage hepatectomies and major liver resection in a similar patient cohort [9, 40].
Moreover, the high rates may also reflect the influence of a learning curve [41]. This effect was also observed with the introduction of two-stage hepatectomy. The initially high mortality rate of 15 % in the inaugural series in 2000 [6] dropped to 7 % in 2008 [41]. Finally, technical modulations of ALPPS, such as partial ALPPS [42] or laparoscopic parenchymal dissection using radio frequency probe, could increase the safety of the procedure.
The poor oncological outcome is a further criticism levelled at ALPPS. This point should, however, be interpreted prudently, as a large proportion of the patients undergoing the ALPPS procedure are the so-called borderline patients, who per se have a poorer outcome due to their high tumor load and aggressive tumor biology [43]. Furthermore, most ALPPS studies were performed with a relatively small number of patients and an inhomogeneous patient cohort over a short observation period [29, 44]. In a recently published meta-analysis by Schadde et al. [39], the morbidity (>IIIa complications) and 30-day mortality rates observed in 295 patients were 44 and 11 %, respectively. This is generally comparable to the limited data for two-stage hepatectomy [7, 40, 45]. The proportion of patients that could not undergo the second stage was merely 2 %, in contrast to 8–30 % in case of two-stage hepatectomy [45]. Despite all the justified criticism which it has attracted, it should be borne in mind that the ALPPS procedure is often the last chance of a potentially curative treatment. Nevertheless, given the high morbidity and mortality rates, careful patient selection is required.
The main limiting factors in this study are its retrospective design and the small number of patients. In addition to this, the statements on morbidity and mortality, as well as the outcome with our inhomogeneous patient cohort, have only limited validity. Furthermore, the follow-up period is still relatively short.
Conclusion
By facilitating the rapid and effective growth of the future liver remnant, the ALPPS procedure may be a suitable alternative for patients after insufficient PVE or indeed the last chance of a potentially curative treatment in this situation. In spite of this, the high morbidity and mortality rates, even in the hands of highly experienced hepatobiliary surgeons, as well as the lack of data on the long-term oncological outcome, should not be ignored. A prudent indication for the use of ALPPS in selected patients, the evaluation of new ALPPS techniques (partial ALPPS, RFA-ALPPS) and randomized controlled trials (RCTs) are essential prerequisites for establishing this procedure as another useful option in the armamentarium of the experienced hepatobiliary surgeon.
References
Agrawal S, Belghiti J (2011) Oncologic resection for malignant tumors of the liver. Ann Surg 253:656–665
Clavien PA, Petrowsky H, DeOliveira ML, Graf R (2007) Strategies for safer liver surgery and partial liver transplantation. N Engl J Med 356:1545–1559
Lam VW, Spiro C, Laurence JM, Johnston E, Hollands MJ, Pleass HC, Richardson AJ (2012) A systematic review of clinical response and survival outcomes of downsizing systemic chemotherapy and rescue liver surgery in patients with initially unresectable colorectal liver metastases. Ann Surg Oncol 19:1292–1301
Makuuchi M, Thai BL, Takayasu K, Takayama T, Kosuge T, Gunvén P et al (1990) Preoperative portal embolization to increase safety of major hepatectomy for hilar bile duct carcinoma: a preliminary report. Surgery 107:521–527
Azoulay D, Castaing D, Krissat J, Smail A, Hargreaves GM, Lemoine A et al (2000) Percutaneous portal vein embolization increases the feasibility and safety of major liver resection for hepatocellular carcinoma in injured liver. Ann Surg 232:665–672
Adam R, Laurent A, Azoulay D, Castaing D, Bismuth H (2000) Two-stage hepatectomy: a planned strategy to treat irresectable liver tumors. Ann Surg 232:777–785
Jaeck D, Oussoultzoglou E, Rosso E, Greget M, Weber JC, Bachellier P (2004) A two-stage hepatectomy procedure combined with portal vein embolization to achieve curative resection for initially unresectable multiple and bilobar colorectal liver metastases. Ann Surg 240:1037–1049 (discussion 1049–51)
van Lienden KP, van den Esschert JW, de Graaf W, Bipat S, Lameris JS, van Gulik TM, van Delden OM (2013) Portal vein embolization before liver resection: a systematic review. Cardiovasc Intervent Radiol 36:25–34
Wicherts DA, Miller R, de Haas RJ, Bitsakou G, Vibert E, Veilhan LA et al (2008) Long-term results of two-stage hepatectomy for irresectable colorectal cancer liver metastases. Ann Surg 248:994–1005
Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, Farkas SA et al (2012) Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg 255:405–414
de Santibañes E, Clavien PA (2012) Playing Play-Doh to prevent postoperative liver failure: the “ALPPS” approach. Ann Surg 255:415–417
Khan AZ, Morris-Stiff G, Makuuchi M (2009) Patterns of chemotherapy-induced hepatic injury and their implications for patients undergoing liver resection for colorectal liver metastases. J Hepatobiliary Pancreat Surg 16:137–144
Lehmann K, Rickenbacher A, Weber A, Pestalozzi BC, Clavien PA (2012) Chemotherapy before liver resection of colorectal metastases: friend or foe? Ann Surg 255:237–247
van der Vorst JR, van Dam RM, van Stiphout RS, van den Broek MA, Hollander IH, Kessels AG, Dejong CH (2010) Virtual liver resection and volumetric analysis of the future liver remnant using open source image processing software. World J Surg 34:2426–2433
Lang SA, Loss M, Schlitt HJ (2013) “In-situ Split” (ISS) liver resection: new aspects of technique and indication. Zentralbl Chir 139:212–219
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Balzan S, Belghiti J, Farges O, Ogata S, Sauvanet A, Delefosse D, Durand F (2005) The, “50–50 criteria” on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg 242:824–828 (discussion 828–9)
Kinoshita H, Sakai K, Hirohashi K, Igawa S, Yamasaki O, Kubo S (1986) Preoperative portal vein embolization for hepatocellular carcinoma. World J Surg 10:803–808
de Graaf W, van Lienden KP, van den Esschert JW, Bennink RJ, van Gulik TM (2011) Increase in future remnant liver function after preoperative portal vein embolization. Br J Surg 98:825–834
Abulkhir A, Limongelli P, Healey AJ, Damrah O, Tait P, Jackson J et al (2008) Preoperative portal vein embolization for major liver resection: a meta-analysis. Ann Surg 247:49–57
Kishi Y, Madoff DC, Abdalla EK, Palavecino M, Ribero D, Chun YS, Vauthey JN (2008) Is embolization of segment 4 portal veins before extended right hepatectomy justified? Surgery 144:744–751
Nagino M, Kanai M, Morioka A, Yamamoto H, Kawabata Y, Hayakawa N, Nimura Y (2000) Portal and arterial embolization before extensive liver resection in patients with markedly poor functional reserve. J Vasc Interv Radiol 11:1063–1068
Kokudo N, Tada K, Seki M, Ohta H, Azekura K, Ueno M et al (2001) Proliferative activity of intrahepatic colorectal metastases after preoperative hemihepatic portal vein embolization. Hepatology 34:267–272
Shindoh J, Vauthey J-N, Zimmitti G, Curley SA, Huang SY, Mahvash A et al (2013) Analysis of the efficacy of portal vein embolization for patients with extensive liver malignancy and very low future liver remnant volume, including a comparison with the associating liver partition with portal vein ligation for staged hepatectomy approach. J Am Coll Surg 217:126–133
de Graaf W, van den Esschert JW, van Lienden KP, van Gulik TM (2009) Induction of tumor growth after preoperative portal vein embolization: is it a real problem? Ann Surg Oncol 16:423–430
Elias D, De Baere T, Roche A, Ducreux M, Leclere J, Lasser P (1999) During liver regeneration following right portal embolization the growth rate of liver metastases is more rapid than that of the liver parenchyma. Br J Surg 86:784–788
Heinrich S, Jochum W, Graf R, Clavien PA (2006) Portal vein ligation and partial hepatectomy differentially influence growth of intrahepatic metastasis and liver regeneration in mice. J Hepatol 45:35–42
Wicherts DA, de Haas RJ, Andreani P, Sotirov D, Salloum C, Castaing D et al (2010) Impact of portal vein embolization on long-term survival of patients with primarily unresectable colorectal liver metastases. Br J Surg 97:240–250
Alvarez FA, Ardiles V, de Santibañes E (2013) The ALPPS approach for the management of colorectal carcinoma liver metastases current colorectal cancer reports 9:168–177
Schadde E, Ardiles V, Slankamenac K, Tschuor C, Sergeant G, Amacker N et al (2014) ALPPS offers a better chance of complete resection in patients with primarily unresectable liver tumors compared with conventional-staged hepatectomies: results of a multicenter analysis. World J Surg 38:1510–1519
de Santibañes E, Alvarez FA, Ardiles V (2012) How to avoid postoperative liver failure: a novel method. World J Surg 36:125–128
Knoefel WT, Gabor I, Rehders A, Alexander A, Krausch M, Schulte am Esch J et al (2013) In situ liver transection with portal vein ligation for rapid growth of the future liver remnant in two-stage liver resection. Br J Surg 100:388–394
Nadalin S, Capobianco I, Li J, Girotti P, Königsrainer I, Königsrainer A (2014) Indications and limits for associating liver partition and portal vein ligation for staged hepatectomy (ALPPS). Lessons learned from 15 cases at a single centre. Z Gastroenterol 52:35–42
Hernandez-Alejandro R, Bertens KA, Pineda-Solis K, Croome KP (2015) Can we improve the morbidity and mortality associated with the associating liver partition with portal vein ligation for staged hepatectomy (ALPPS) procedure in the management of colorectal liver metastases? Surgery 157:194–201
Truant S, Scatton O, Dokmak S, Regimbeau JM, Lucidi V, Laurent A et al (2015) Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): impact of the inter-stages course on morbi-mortality and implications for management. Eur J Surg Oncol 41:674–682
Schlegel A, Lesurtel M, Melloul E, Limani P, Tschuor C, Graf R et al (2014) ALPPS: from human to mice highlighting accelerated and novel mechanisms of liver regeneration. Ann Surg 260:839–846 (discussion 846–7)
Dokmak S, Belghiti J (2012) Which limits to the “ALPPS” approach? Ann Surg 256:e6 (author reply e16–e6; author reply e17)
Kokudo N, Shindoh J (2013) How can we safely climb the ALPPS? Updates Surg 65:175–177
Schadde E, Ardiles V, Robles-Campos R, Malago M, Machado M, Hernandez-Alejandro R et al (2014) Early survival and safety of ALPPS: first report of the international ALPPS registry. Ann Surg 260:829–838
Brouquet A, Abdalla EK, Kopetz S, Garrett CR, Overman MJ, Eng C et al (2011) High survival rate after two-stage resection of advanced colorectal liver metastases: response-based selection and complete resection define outcome. J Clin Oncol 29:1083–1090
Alvarez FA, Ardiles V, de Santibañes M, Pekolj J, de Santibañes E (2015) Associating liver partition and portal vein ligation for staged hepatectomy offers high oncological feasibility with adequate patient safety: a prospective study at a single center. Ann Surg 261:723–732
Petrowsky H, Györi G, de Oliveira M, Lesurtel M, Clavien PA (2015) Is partial-ALPPS safer than ALPPS? A single-center experience. Ann Surg 261:e90–e92
Oldhafer KJ, Donati M, Jenner RM, Stang A, Stavrou GA (2013) ALPPS for patients with colorectal liver metastases: effective liver hypertrophy, but early tumor recurrence. World J Surg 38:1504–1509
Schadde E, Schnitzbauer AA, Tschuor C, Raptis DA, Bechstein WO, Clavien PA (2014) Systematic review and meta-analysis of feasibility, safety, and efficacy of a novel procedure: associating liver partition and portal vein ligation for staged hepatectomy. Ann Surg Oncol 22:3109–3120
Lam VW, Laurence JM, Johnston E, Hollands MJ, Pleass HC, Richardson AJ (2013) A systematic review of two-stage hepatectomy in patients with initially unresectable colorectal liver metastases. HPB (Oxford) 15:483–491
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors reported no conflicts of interest.
Rights and permissions
About this article
Cite this article
Ulmer, T.F., de Jong, C., Andert, A. et al. ALPPS Procedure in Insufficient Hypertrophy After Portal Vein Embolization (PVE). World J Surg 41, 250–257 (2017). https://doi.org/10.1007/s00268-016-3662-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3662-3