Abstract
Objectives
Postoperative wound disruption is associated with high morbidity and mortality. We sought to identify the risk factors and outcomes of wound disruption following colorectal resection.
Methods
The American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database was used to examine the clinical data of patients who underwent colorectal resection from 2005 to 2013. Multivariate regression analysis was performed to identify risk factors of wound disruption.
Results
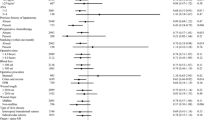
We sampled a total of 164,297 patients who underwent colorectal resection. Of these, 2073 (1.3 %) had wound disruption. Patients with wound disruption had significantly higher mortality (5.1 vs. 1.9 %, AOR: 1.46, P = 0.01). The highest risk of wound disruption was seen in patients with wound infection (4.8 vs. 0.9 %, AOR: 4.11, P < 0.01). A number of factors are associated with wound disruption such as chronic steroid use (AOR: 1.71, P < 0.01), smoking (AOR: 1.60, P < 0.01), obesity (AOR: 1.57, P < 0.01), operation length more than 3 h (AOR: 1.56, P < 0.01), severe Chronic Obstructive Pulmonary Disease (COPD) (AOR: 1.36, P < 0.01), urgent/emergent admission (AOR: 1.31, P = 0.01), and serum Albumin Level <3 g/dL (AOR: 1.27, P < 0.01). Laparoscopic surgery had significantly lower risk of wound disruption compared to open surgery (AOR: 0.61, P < 0.01).
Conclusion
Wound disruption occurs in 1.3 % of colorectal resections, and it correlates with mortality of patients. Wound infection is the strongest predictor of wound disruption. Chronic steroid use, obesity, severe COPD, prolonged operation, non-elective admission, and serum albumin level are strongly associated with wound disruption. Utilization of the laparoscopic approach may decrease the risk of wound disruption when possible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postoperative wound disruption or separation of the layers of a surgical wound with disruption of the fascia is a serious complication which is associated with increased morbidity, mortality, length of hospitalization, and hospital costs [1, 2]. It is estimated that 1–3 % of surgical patients develop wound disruption [3]. Despite improvements in contemporary perioperative care, data do not show any significant decrease in rate of wound disruption, and wound disruption still remains a major cause of morbidity in surgical patients [3].
Although the development of wound disruption is closely related to the surgical technique of wound closure, local and systemic factors have significant influence on surgical wound healing [4]. Furthermore, factors such as obesity, jaundice, malignancy, diabetes mellitus, and wound infection have been reported as predictors of wound disruption [4, 5]. Recent published articles report on the benefits of prophylactic retention sutures and rectus sheath relaxing incisions in high-risk patients [2, 4, 6]. However, there are no specific guidelines of preventive strategies of wound disruption for high-risk patients. Using a nationwide database, this study aims to report the trends and the contemporary status of wound disruption following colorectal surgery in the United States (US), characterize reducible risk factors, and identify high-risk patients for wound disruption in colorectal surgery.
Materials and methods
Data for this study were collected within the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) Participant User Files (PUF) for 2005 through 2013. ACS NSQIP is the leading nationally validated, risk-adjusted, outcomes-based program to measure and improve the quality of surgical care in the United States [7]. This study evaluated preoperative to 30-day postoperative outcomes of patients who underwent colorectal resections using the appropriate procedure codes as specified by the current procedural terminology (CPT) codes. These codes include 44140–44160, 44204–44212, 44227, 44625, 45110-45114, 45119, 45120, 45123, 45126, 45135, 45397, 45402, 45550, and 45395. Patients who underwent colorectal surgery without colorectal resection, patients younger than 18 years, patients who had infected or open wounds during admission, and patients who had surgical abdominal wound other than wound class II (clean contaminated) were excluded from this study. Patient diagnoses were defined based on the International Classification of Diseases, 9th Revision, clinical modifications (ICD-9-CM) codes. Wound disruption was defined as separation of the layers of a surgical wound, which may be partial or complete, with disruption of the fascia within 30 days of the operation according to the standard definition of American College of Surgeons [7].
Potential variables used in the analysis included baseline demographics (age, sex, and race), comorbidities, surgical approach (open vs. laparoscopic), operation length, admission type (emergent vs. non-emergent), and the most recent preoperative blood chemical values of serum albumin level, serum and white blood cell count. Definitions for NSQIP collected data points according to American College of surgeons (ACS) definition are available online in the NSQIP user guide and also are listed in Table 1 [8]. Also, anemia was defined as hematocrit less than ten. Primary end points investigated were preoperative and operative factors which had significant associations with postoperative wound dehiscence. Secondary endpoints investigated were associations between postoperative wound infection and wound disruption.
Statistical analysis
Statistical analyses were performed using the SPSS® software, Version 22 (SPSS Inc., Chicago, IL). The main analysis of the study was multivariable analysis. Logistic regression analysis was used to estimate the association between categorical variables and postoperative wound disruption, and multivariate analysis using linear regression was used for the continuous variables. For each correlation, the adjusted odds ratio (AOR) with a 95 % confidence interval was calculated and reported. P values less than 0.05 were considered statistically significant. Adjustments were made for all variables of the study. In order to report performance measures of the regression analysis model, Cox & Snell R 2 of the regression analysis model was reported, which was 0.013.
Results
Overall, 164,297 patients who underwent colorectal resection were identified. The median age of patients was 63 years old; the majority of the patients were Caucasian (85.7 %) and female (52 %). Patients with and without wound disruption were compared for demographic data and comorbidities factors which are reported in Table 2.
The overall rate of postoperative wound disruption was 1.3 %. There was a steady decrease in rate of wound disruption during the study period from 1.6 % in 2005 to 1.1 % in 2013. Overall, 52.9 % of patients with wound disruption underwent reoperation in 30 days after surgery. The median day of diagnosis of wound disruption was 10 days after operation and 43.8 % of wound disruption events happened after discharge from hospital (Fig. 1). Further, wound infection existed in 36.7 % of the patients with wound disruption. Among patients with wound disruption and wound infection, 86.3 % had wound infection prior to wound disruption and 13.7 % developed wound infection after wound disruption. Also, 5.6 % of patients with wound infection had wound disruption (761/13,691).
The risk-adjusted analysis for factors associated with wound disruption is reported in Table 3. The strongest predictor of wound disruption was wound infection (AOR: 4.11, P < 0.01). Among comorbid conditions, chronic steroid use had the strongest association with wound disruption. Also the ASA score was associated with wound disruption. Also, patients with a serum albumin level lower than three g/dL had a significantly higher risk of wound disruption compared to patients with a serum albumin level more than 3.5 g/dL (Fig. 2; Table 2). With regard to types of procedures, patients who underwent pelvic exenteration (3.5 %) had the highest rate of wound disruption. Following adjustment, pelvic exenteration was associated with a substantial risk of wound disruption compared to other procedures (AOR: 2.22, P = 0.03).
Following risk adjustment, wound disruption had a significant effect on mortality of patients (5.1 vs. 1.9 %, AOR: 1.46, P = 0.01). Also, patients who had wound disruption had 1 week longer postoperative hospitalization compared to patients without the complication (adjusted mean difference: 7 days, 7.22–7.96, P < 0.01). Complications of sepsis, septic shock, intra-abdominal infections, hospitalization more than 1 month, return to operation room, and deep vein thrombosis were significantly higher in patients with wound disruption (Table 4).
Discussion
Our analysis reinforces the serious effects of wound disruption on outcomes of surgical patients. Our study shows the mortality of patients with wound disruption to be twice that of patients without wound disruption. Also, we found an increased risk of sepsis, septic shock, prolonged hospitalization, deep vein thrombosis, intra-abdominal infection, and reoperation in patients with wound disruption. High mortality, morbidity, hospitalization length, and hospital cost of patients with wound disruption were reported previously [4, 5, 9, 10]. However, comparison of outcomes of patients with and without wound disruption should be judged with caution as these two groups of patients are not two homogeneous groups of patients and their comorbidities and severity of disease varied broadly. Although we adjusted our results with multiple factors, it is not possible to adjust for all covariants. Nevertheless, investigating high-risk patients and implementing risk factor modification prior to surgery may decrease the morbidity and mortality of patients.
Wound disruption is a preventable morbidity in colorectal surgery. This study introduces a number of perioperative factors which have associations with wound disruption. While previous reports noted low serum albumin level, chronic lung disease, wound infection, and obesity as risk factors of wound disruption in surgical patients [4, 5, 10, 11], we further identified 13 other factors which had associations with wound disruption. Considering a number of risk factors are reducible, preventive strategies with the focus on reducing the risk factors should be planned. Overall, wound infection is the strongest predictor of wound disruption. We found the risk of wound disruption increases more than four times in presence of wound infection. Effect of wound infection on wound disruption has been cited multiple times in literature [11–13]. Among comorbid conditions, chronic use of steroids was the factor with the strongest association with wound disruption. The adverse effects of corticosteroids on wound healing have been cited previously [14, 15]. The adverse effects are explained by interactions of corticosteroids in the process of fibroblast proliferation, collagen synthesis, angiogenesis, wound contraction, and re-epithelialization of surgical wound [15]. In addition, recent studies reported adverse effects of steroid use in colonic anastomosis [16, 17]. We suggest steroids should be tapered out or at least reduced before surgery whenever possible. Vitamin A can ameliorate the deleterious effects of steroids on wound healing when they cannot be reduced [18]. We further demonstrated that the serum albumin level can predict the risk of postoperative wound dehiscence (Fig. 2). Serum albumin level has been linked to the patients’ nutritional status and mortality and morbidity of colorectal patients [19–22]. This correlation is in line with previous reports of an association between malnutrition and wound disruption [4, 9]. Improving the nutritional status in patients with nutritional deficiencies seems logical. However, serum albumin level is not a reliable marker of nutritional status in presence of physiological stress and high CRP levels [23, 24]. Evaluating methods for nutritional status other than serum albumin level should be used for patients with high CRP.
Obesity increases risk of wound dehiscence. We found the lowest rates of wound disruption occur in patients with a normal BMI (18.5–24.9) and the highest rates of wound disruption occur in patients with BMI greater than forty. The association between obesity and wound healing has long been established [25]. Obese patients may benefit from nutritional support with A, B complex, and C vitamins prior to operation [25].
In line with literature, our results show that a laparoscopic approach is associated with a decrease in the risk of wound disruption [26]. Although the inherent selection bias of laparoscopic compared to open surgery makes comparison difficult, we found that laparoscopic surgery is associated with a decrease in risk of wound disruption by 39 % compared to open operation. However, emergently admitted patients more often have wound disruption and it is difficult to establish the feasibility and benefits of a laparoscopic approach for these patients. Utilization of laparoscopic surgery in abdominal emergencies needs more investigation.
Among colorectal procedures, pelvic exenteration has the highest risk of postoperative wound disruption. We found a two-time higher risk of wound disruption after pelvic exenteration compared to a partial colectomy. It can be related to the higher rate of wound infection and disruption in perineal wound compared to abdominal wound [27, 28]. Wound dehiscence was previously reported as a one of the common complications of pelvic exenteration by Wydra [27]. Preventive strategies such as the vacuum wound closure system in high-risk patients undergoing pelvic exenteration warrant consideration. Advantages of vacuum assisted closure on healing of perineal surgical wound have been reported in literature [29, 30]. Although vacuum wound closure does not reduce the bacterial load of surgical wound, a significant reduction of wound surface area using vacuum assisted closure may have positive effects on wound healing [31].
Our study results show that 43.8 % of wound disruption events occur after hospital discharge in colorectal surgery. Also, we found that postoperative day eight was the time with the highest incidence of wound disruption (Fig. 1) which is in line with the previously reported postoperative period of 6–8 day as the most common day of wound disruption by Begum [5]. Considering a significant percentage of wound disruption events occur following hospital discharge, it seems logical to take all necessary steps to prevent this complication after discharge. Currently there is no specific postoperative strategy for prevention of wound disruption.
The treatment of wound disruption is associated with unsatisfactory results [11, 32–34]. The decision is usually made according to the size of the fascia defect, presence or absence of evisceration, general condition of patients, and presence of infection [11]. However, the postoperative incidence rate of incisional hernia has been reported 19–45 % in literature [11, 32–34]. The available options include primary closure of fascia and skin, temporary packing, use of prosthetic mesh, or skin closure only [11, 32]. In about half of cases, as our data also revealed, the patient will receive surgical closure immediately [11, 32, 35]. However, suture repair in patients with obvious tissue necrosis, infection, and loss of the abdominal wall is associated with a 50 % rate of failure [36]. In such patients, we would suggest closure of the wound only after debridement of the necrotic tissue and control of any infection until granulation tissue appears [11, 32]. Non-operative management with only skin closure, accepting an inevitable hernia, is possible for patients with small defects [11, 32]. Also, if the general status of the patient does not support immediate surgery, non-operative management with temporary packing or skin closure is suggested [11, 32]. We found 52.9 % of patients with wound disruption underwent reoperation within 30 days after surgery. However, considering the retrospective nature of this study due to using patients’ discharge data, the reported rate may be lower than the actual rate of need for reoperation following wound disruption. Also, our result shows 43.8 % of wound disruption events occurred after discharge, so some of the patients may have been re-operated in NSQIP non-participant hospitals and we could not track them. Finally, we have no data on rate of ultimate hernia formation or hernia repair on this group of patients.
Study limitations
The retrospective nature of this study makes any conclusions difficult. The surgical technique is one of the most important factors associated with wound disruption and the ACS NSQIP database lacks information regarding type and length of surgical incision, place of the surgical incision (abdominal vs. perineal) as well as the closing technique of the fascia and surgical wound [37]. We compared clinical factors of patients with and without wound disruption. However, these two groups of patients were not homogeneous regarding indication for surgery, stage of the disease, type of procedure, and surgical approach. Although we adjusted study results with the multiple factors, we could not adjust them for the stage of the disease which can affect the results. In addition, NSQIP does not provide any details regarding long term outcomes of closure of surgical wound in patients with wound disruption as incisional hernia is reported in 43 % of patients who suffer wound disruption [3]. NSQIP database also does not include some details such as the utilization of drains in surgery and dosage and type of the corticosteroid drugs, which may impact risk for wound disruption [1]. Despite these limitations, in our knowledge, this study is the first nationwide report on wound disruption in colorectal resection procedures using multivariate analysis.
Conclusion
Overall, 1.3 % of colorectal operations are complicated with wound disruption, and 43.8 % of these events happen after hospital discharge. Wound disruption increases mortality and hospitalization length of surgical patients significantly. Wound infection is the strongest predictor of wound disruption. Chronic steroid use, obesity, and serum albumin level are significantly associated with wound disruption. Considering a number of risk factors are reducible, preventive strategies should be designed for high-risk patients. Pelvic exenteration procedure has the highest procedure-specific risk of wound disruption. Strategies to decrease the rate of wound infection and correcting nutritional deficiencies of patients as well as utilization of laparoscopic surgery may lead to a decreased rate of wound disruption.
References
Cöl C, Soran A, Cöl M (1998) Can postoperative abdominal wound dehiscence be predicted? Tokai J Exp Clin Med 23:123–127
Khorgami Z, Shoar S, Laghaie B, Aminian A, Hosseini Araghi N, Soroush A (2013) Prophylactic retention sutures in midline laparotomy in high-risk patients for wound dehiscence: a randomized controlled trial. J Surg Res 180:238–243
Hahler B (2006) Surgical wound dehiscence. Medsurg Nurs 15:296–300; quiz 301
Mäkelä JT, Kiviniemi H, Juvonen T, Laitinen S (1995) Factors influencing wound dehiscence after midline laparotomy. Am J Surg 170:387–390
Begum B, Zaman R, Ahmed M, Ali S (2008) Burst abdomen-A preventable morbidity. Mymensingh Med J 17:63–66
Marwah S, Marwah N, Singh M, Kapoor A, Karwasra RK (2005) Addition of rectus sheath relaxation incisions to emergency midline laparotomy for peritonitis to prevent fascial dehiscence. World J Surg 29:235–239
National surgical quality improvement program (2005). American College of Surgeons, Chicago. Cited 17 Jan 2012. www.acsnsqip.org
User guide for the 2011 participant use data file. American College of Surgeons national surgical quality improvement program (2012). http://site.acsnsqip.org/wp-content/uploads/2012/03/2011-User-Guide_Final.pdf. Cited April 2015
Rodríguez-Hermosa JI, Codina-Cazador A, Ruiz B, Roig J, Gironès J, Pujadas M et al (2005) Risk factors for acute abdominal wall dehiscence after laparotomy in adults. Cir Esp 77:280–286
Shanmugam VK, Fernandez S, Evans KK, McNish S, Banerjee A, Couch K et al (2015) Postoperative wound dehiscence: predictors and associations. Wound Repair Regen 23:184–190
van Ramshorst GH, Eker HH, Harlaar JJ, Nijens KJ, Jeekel J, Lange JF (2010) Therapeutic alternatives for burst abdomen. Surg Technol Int 19:111–119
Gürleyik G (2001) Factors affecting disruption of surgical abdominal incisions in early postoperative period. Ulus Travma Derg 7:96–99
Yahchouchy-Chouillard E, Aura T, Picone O, Etienne JC, Fingerhut A (2003) Incisional hernias. I. Related risk factors. Dig Surg 20:3–9
Wicke C, Halliday B, Allen D, Roche NS, Scheuenstuhl H, Spencer MM et al (2000) Effects of steroids and retinoids on wound healing. Arch Surg 135:1265–1270
Anstead GM (1998) Steroids, retinoids, and wound healing. Adv Wound Care 11:277–285
Baca B, Ozben V, Boler DE, Onur E, Hamzaoglu I, Karahasanoglu T et al (2010) Effect of corticosteroid dose and duration of administration on colonic anastomosis. Inflamm Bowel Dis 16:2162–2167
Eubanks TR, Greenberg JJ, Dobrin PB, Harford FJ, Gamelli RL (1997) The effects of different corticosteroids on the healing colon anastomosis and cecum in a rat model. Am Surg 63:266–269
Phillips JD, Kim CS, Fonkalsrud EW, Zeng H, Dindar H (1992) Effects of chronic corticosteroids and vitamin A on the healing of intestinal anastomoses. Am J Surg 163:71–77
Lohsiriwat V, Chinswangwatanakul V, Lohsiriwat S, Akaraviputh T, Boonnuch W, Methasade A et al (2007) Hypoalbuminemia is a predictor of delayed postoperative bowel function and poor surgical outcomes in right-sided colon cancer patients. Asia Pac J Clin Nutr 16:213–217
Lohsiriwat V, Lohsiriwat D, Boonnuch W, Chinswangwatanakul V, Akaraviputh T, Lert-Akayamanee N (2008) Pre-operative hypoalbuminemia is a major risk factor for postoperative complications following rectal cancer surgery. World J Gastroenterol 14:1248–1251
Gibbs J, Cull W, Henderson W, Daley J, Hur K, Khuri SF (1999) Preoperative serum albumin level as a predictor of operative mortality and morbidity: results from the National VA Surgical Risk Study. Arch Surg 134:36–42
Fuhrman MP, Charney P, Mueller CM (2004) Hepatic proteins and nutrition assessment. J Am Diet Assoc 104:1258–1264
Gabay C, Kushner I (1999) Acute-phase proteins and other systemic responses to inflammation. N Engl J Med 340:448–454
Banh L (2006) Serum proteins as markers of nutrition: what are we treating? Pract Gastroenterol 30:46–64
Pierpont YN, Dinh TP, Salas RE, Johnson EL, Wright TG, Robson MC et al (2014) Obesity and surgical wound healing: a current review. ISRN Obes 2014:638936
Moghadamyeghaneh Z, Masoomi H, Mills SD, Carmichael JC, Pigazzi A, Nguyen NT, et al (2014) Outcomes of conversion of laparoscopic colorectal surgery to open surgery. JSLS 18:e2014.00230. doi:10.4293/JSLS.2014.00230
Wydra D, Emerich J, Sawicki S, Ciach K, Marciniak A (2006) Major complications following exenteration in cases of pelvic malignancy: a 10-year experience. World J Gastroenterol 12:1115–1119
Artioukh DY, Smith RA, Gokul K (2007) Risk factors for impaired healing of the perineal wound after abdominoperineal resection of rectum for carcinoma. Colorectal Dis 9:362–367
Cresti S, Ouaïssi M, Sielezneff I, Chaix JB, Pirro N, Berthet B et al (2008) Advantage of vacuum assisted closure on healing of wound associated with omentoplasty after abdominoperineal excision: a case report. World J Surg Oncol 6:136
Gümüş N (2009) Vacuum-assisted closure of perineal war wound related to rectum. Eplasty 9:e55
Mouës CM, Vos MC, van den Bemd GJ, Stijnen T, Hovius SE (2004) Bacterial load in relation to vacuum-assisted closure wound therapy: a prospective randomized trial. Wound Repair Regen 12:11–17
Cliby WA (2002) Abdominal incision wound breakdown. Clin Obstet Gynecol 45:507–517
Grace RH, Cox SJ (1973) Incidence of incisional hernia following dehiscence of the abdominal wound. Proc R Soc Med 66:1091–1092
White H, Cook J, Ward M (1977) Abdominal wound dehiscence. A 10-year survey from a district general hospital. Ann R Coll Surg Engl 59:337–341
Fleischer GM, Rennert A, Rühmer M (2000) Infected abdominal wall and burst abdomen. Chirurg 71:754–762
Carlson MA (1997) Acute wound failure. Surg Clin North Am 77:607–636
Israelsson LA, Millbourn D (2013) Prevention of incisional hernias: how to close a midline incision. Surg Clin North Am 93:1027–1040
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moghadamyeghaneh, Z., Hanna, M.H., Carmichael, J.C. et al. Wound Disruption Following Colorectal Operations. World J Surg 39, 2999–3007 (2015). https://doi.org/10.1007/s00268-015-3208-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-3208-0