Abstract
Background
Hepatocellular carcinoma (HCC) is the third leading cause of cancer-related death internationally, it is necessary to reappraise evidences of HCC cells involving the portal vein, especially considering tumor size.
Materials and methods
Histopathological evidence and dynamic evidences of radiology and cytology from publication were collected and analyzed.
Results
Frequencies of microscopic portal vein involvement (MPVI) and microscopic intrahepatic metastasis (MIM) in resected specimens with single nodule HCC were lower than that of multi nodule HCC, although not significantly. Early HCC (≤1.5 cm) was with extremely low to 0 frequencies of MPVI and MIM. HCC >5 cm showed a tendency of flowing HCC cells into portal vein, which was coincident with significantly high frequency (64.1 %) of MPVI for HCC >5 cm. There were no significant difference of frequencies of MPVI and MIM between groups of tumor ≤2, ≤3, and ≤5 cm.
Conclusions
Single nodule HCC >5 cm needs anatomic resection and the root of portal vein should be firstly ligated because of tendency of flowing HCC cells into portal vein. For single nodule HCC ≤2 cm, there was a risk of about 16.2 % of MPVI, and a risk of about 16.2–26.4 % of MPVI for those single nodule HCC ≤5 cm, however, there was a risk of extremely low to 0 of MPVI for early HCC (≤1.5 cm). Surgeons have to balance liver reserve and risk of MPVI for HCC ≤5 cm before deciding anatomic or nonanatomic resection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the third leading cause of cancer-related death internationally [1]. It was internationally estimated for the year 2000 that HCC was the fifth most common cancer in men and the eighth most common cancer in women [2]. Eastern Asia, Middle Africa, and some countries of Western Africa are the areas with highest risk of HCC prevalence. Patients with HCC showed an overall population-based 1- and 3-year survival of 20 and 5 % respectively, which was unsatisfying, however, 5-year survival of patients with resectable HCC ranged widely from 35 to 70 % according to literature [3–8].
Although there are kinds of treatment modalities for HCC, hepatic resection is a widely accepted treatment modality for HCC. Hepatic resection is an aggressive treatment for selected HCC patients, and only which can provide potentially curative options for HCC [9–11].There were lots of clinical analysis considering the outcome between nonanatomic and anatomic resection based on Couinaud’s segments of liver anatomy since 1980s, attempting to provide clinical evidences of whether nonanatomic and anatomic resection showed superiority, however, the result remains controversial.
One may be curious, if there is any supportive theory for the performance of anatomic resection for HCC, because nonanatomic or limited resection can be performed not so technically demanded and can contribute to more liver remnant reservation. The supportive theory should be the following 3 points: 1. Couinaud’s portal segments of liver anatomy; 2. HCC cells tend to invade the portal vein, tumor subsequently spread into the regional hepatic regions and result in satellite nodules, anatomic resection can eradicate venous tumor thrombi present within the anatomically resected domain [12, 13]; 3. Microscopic vascular invasion is a strong predictor of outcome following hepatic resection and liver transplantation of HCC [14–17]. Couinaud’s portal segments of liver anatomy and microscopic vascular invasion as strong prognostic predictors are now globally accepted.
That HCC cells tend to invade the portal vein or have high frequent invasion to portal vein was gradually present in literature since early 1980s. In 1983, Makuuchi M. et al. [12] reported that microscopic tumor thrombus in the portal venous branch was found in 73 % of 62 patients with HCC less than 5 cm, which seems the first description of frequency of HCC cells invading portal vein. Although there were similar reports subsequently, most of which did not aim to focus on frequency of HCC cells invading portal vein. Moreover, thanks to the development of imaging modality, biomarkers, and surveillance guideline, more and smaller HCC with early stage can be detected [18–21]. Then how often do HCC cells invade portal vein, especially for HCC with smaller size? Therefore, it is necessary to reappraise evidences of HCC cells involving the portal vein, especially considering tumor size.
Materials and methods
Methods of evidence acquisition and data sources
In order to revisit and reappraise evidences of HCC cells invading the portal vein, the following evidence acquisitions were applied. The first acquisition was the frequency of microscopic portal vein involvement (MPVI, including portal vein invasion and portal vein tumor thrombus) and microscopic intrahepatic metastasis (MIM) in resected specimens and attention was paid to tumor size, which is histopathological evidence. The second acquisition was radiology and cytology evidence regarding tumor to the associated portal vein, which is dynamic evidence.
Studies were identified by searching MEDLINE and PubMed databases for articles with keywords “portal invasion and HCC”, “anatomic resection and HCC”, “anatomical resection and HCC”, “systematic hepatectomy and HCC”, “segmentation resection and HCC”, Additional papers and book chapters were identified by a manual search of references from reviewed articles.
Statistics
Data were presented as mean ± S.D. values. For statistical analyses, Student’s t test was used to compare data between single nodule and multi nodule. If data were not of normality with tests for normality, Wilcoxon two-sample test was applied. Spearman’s correlation coefficient analysis was used for identifying correlation between MPVI and MIM in resected specimens. ANOVA was applied for analyzing difference between groups of different tumor sizes. Significance levels of p < 0.05 were considered as statistically significant.
Results
A total of 409 literatures were found, and literatures of recurrence HCC, macroscopic vascular invasion, only microscopic vascular invasion that including portal and hepatic veins were excluded. For the first acquisition of histopathological evidence, 70 literatures regarding portal vein involvement and/or micrometastasis were identified, from which 65 series were used for statistics (Table 1) [22–68]. There were 3 literatures of radiology and 2 literatures of cytology of dynamic evidences.
Frequencies of MPVI and MIM in resected specimens
There were 58/65 (89.2 %) series with consecutive cases in patient collection. The consecutive period of each series ranged from 2–21 years (12.3 ± 5.3); the case number of each series ranged from 5–1,139 cases (169.5 ± 193).
Frequency of MPVI in resected specimens of each series was (26.4 ± 17.3) %, ranging from 0–73 %, and frequency of MIM in resected specimens of each series was (21.5 ± 16.5) %, ranging from 0–66.7 %.There were 5 series (110 cases) with tumors ≤1.5 cm and single nodule (early HCC), frequency of MPVI in resected specimens was 0.5 % (3 of 4 series were 0), and frequency of MIM was 0.
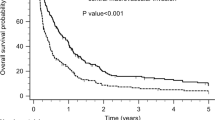
Spearman’s correlation coefficient analysis revealed that, among 22 series with both data of MPVI and MIM, there was significant correlation between MPVI and MIM in resected specimens, the coefficient was 0.60, p = 0.0035 (Fig. 1).
When the data was stratified by single nodule or multi nodules, frequency of MPVI in resected specimens with single nodule of each series was (21.6 ± 17) %, ranging from 0–64.1 %, however, frequency of MPVI in resected specimens with multi nodules of each series was (28.5 ± 12.8) %, ranging from 7.1–48.2 %, and there was no significance between single nodule or multi nodules (p = 0.156). Frequency of MIM in resected specimens with single nodule of each series was (18.8 ± 16.6) %, ranging from 0–66.7 %, however, frequency of MIM in resected specimens with multi nodules of each series was (23.1 ± 15.7) %, ranging from 0–62.9 %, and there was no significance between single nodule or multi nodules (p = 0.363).
Then data was stratified by tumor size and all tumors were with single nodule (Table 2). It was obvious that early HCC was with very low frequency of MPVI and MIM, almost with frequency of 0. ANOVA result showed that there were no significant difference between groups of tumor ≤2, ≤3, and ≤5 cm, however, group of tumor >5 cm showed significantly higher frequency.
Dynamic evidences of radiology and cytology
There were 3 literatures regarding radiology about relation between tumor and surrounding vessels. Nakashima T. firstly proposed that using barium infusion in HCC, arterial branches acted as afferent vessels, and capillarized sinusoids and portal branches as efferent channels, almost all intrahepatic metastases should result from portal vein invasion of HCC in 1976 [69].Okamoto E.et al. [22] in 1987 reported that in 15 resected HCC specimens, barium sulfate solution was injected directly into the tumor, in 12 cirrhotic specimens, the portal branches were clearly visualized, while hepatic vein branches were not or only faintly stained, the frequency was 80 % (12/15). In 1996, Toyosaka A. also injected radiopaque media to HCC of 23 specimens, in which 74 % (17/23) showed fully visualized portal branches, while hepatic vein branches were not filled at all. In the remaining 26 %, both portal and hepatic vein branches were opacified, but the portal vein branch was always filled more predominantly [70].
There were 2 literatures regarding cytology about relation between tumor and surrounding vessels. In 1990, Yamamoto M. et al. [71] reported that saline solution was injected into the hepatic artery of 27 livers with HCC, samples were collected through the portal and the hepatic vein. HCC cells were detected significantly in 14.8 % (4/27) from the portal vein, 5.3 % (1/19) from the hepatic vein were not significantly detected, tumors >5 cm in diameter showed a tendency of flowing HCC cells into portal vein. In 1992, Yamanaka N.et al. [32] reported that blood samples were taken from portal veins of 31 HCC patients receiving hepatic resection, which were then stained and screened for HCC cells, the total recovery rate of HCC cells was 22.58 % (7/31). Recovery rate of HCC cells was 0 for tumor ≤5 cm, 38 % for tumor ≤10 cm but >5 cm, and 80 % for tumor >10 cm.
Discussion
Anatomic resection is the removal of liver segment confined by tumor-bearing portal tributaries, whereas nonanatomic resection is the removal of the tumor with adequate margin. Anatomic resection became intact and popular, especially in Japan since 1981 when Makuuchi M. [72] proposed systematic sub-segmentectomy and blue dye injection into the relating feeding portal vein to confirm the portal tributaries that lack landmarks on the surface of liver, however, the superiority of anatomic or nonanatomic resection remains controversial.
It is necessary to reappraise evidences of HCC cells involving the portal vein which is one supportive point of anatomic resection, because HCC can be diagnosed earlier nowadays, the frequency of HCC cells invading the portal vein microscopically may be different from that reported in 1980s and 1990s, especially when considering the size of tumor.
In the total 409 literatures, there are many studies only focusing on microvascular invasion or micrometastasis, rather than MPVI or MIM, because it is difficult to distinguish intracapsular portal vein from hepatic vein; such literatures were excluded in current research. The accurate intracapsular portal vein involvement remains a limitation of current research because the consensus of histological criteria of identifying intracapsular portal vein involvement has not yet been established [64].
MIM can be consequence of spread of tumor through portal invasion [7, 42], which was also demonstrated in current research that MPVI was significantly correlated with MIM. MIM was also observed in current research. 89.2 % of included series in current research were consecutive, with average 12.3 years and 169.5 cases for each series, which can contribute to less bias from literatures. The average frequency of MPVI in resected specimens was 26.4 and 21.5 % for frequency of MIM from overall 65 series, and we only encountered 3 frequencies of MPVI and 1 frequency of MIM, which were more than 50 %. It seems not so frequent when compared to the top 73 % [12].
Gross type, tumor size, tumor number, and tumor differentiation were tumor characteristics, which can be prognostic factors. The frequencies of MPVI and MIM were stratified by tumor size and tumor number in current research. Although there were no significant differences of frequencies of MPVI and MIM between single nodule and multi nodule HCC, frequencies of MPVI and MIM of HCC with single nodule were lower than that of HCC with multi nodules.
It was reported that early HCC was with significant smaller size (usually no more than 1.5 cm) when compared to other types of HCC [39].There were 5 series with such kind of early HCC that were all single nodule HCC. These series were included to stratification of HCC ≤1.5 cm. It was obvious that early HCC was with extremely low frequencies of MPVI and MIM, almost with no MPVI and MIM. For those single nodule HCC ≤2, ≤3, ≤5, and >5 cm, frequencies of MPVI and MIM of single nodule HCC >5 cm were the significantly highest, however, frequencies of MPVI and MIM between single nodule HCC ≤2, ≤3, and ≤5 cm were not significantly different.
Radiology and cytology of dynamic evidences also revealed that portal vein acted as efferent vessel for HCC, which maybe the reason that there was higher frequency of portal vein involvement than hepatic vein involvement. HCC >5 cm showed a tendency of flowing HCC cells into portal vein, which was coincident with significantly high frequency (64.1 %) of MPVI for HCC >5 cm.
There were several limitations in current research besides unclear accurate intracapsular portal vein involvement. Data were not stratified by gross type and tumor differentiation which were important characteristics as tumor size and tumor number. Furthermore, case number and patient inclusion criteria of each consecutive series varied, which could be negative to homogenous and veracity of current research.
Conclusion
In conclusion, the frequency of MPVI of single nodule HCC was lower than that of multi nodule HCC. For single nodule HCC >5 cm, the frequency (64.1 %) of MPVI was significantly high, which needs anatomic resection and the root of portal vein should be firstly ligated because of tendency of flowing HCC cells into portal vein. For single nodule HCC ≤2 cm, there was a risk of about 16.2 % of MPVI, and a risk of about 16.2–26.4 % of MPVI for those single nodule HCC ≤5 cm, however, there was a risk of extremely low to 0 of MPVI for early HCC (≤1.5 cm). Surgeons have to balance liver reserve and risk of MPVI for HCC ≤5 cm before deciding anatomic or nonanatomic resection.
References
Parkin DM (2001) Global cancer statistics in the year 2000. Lancet Oncol 2:533–543
Bosch FX, Ribes J, Diaz M et al (2004) Primary liver cancer: worldwide incidence and trends. Gastroenterology 127:S5–S16
Davila JA, El-Serag HB (2006) Racial differences in survival of hepatocellular carcinoma in the United States: a population-based study. Clin Gastroenterol Hepatol 4:104–110
Duffy JP, Hiatt JR, Busuttil RW (2008) Surgical resection of hepatocellular carcinoma. Cancer J 14:100–110
Bruix J, Llovet JM (2002) Prognostic prediction and treatment strategy in hepatocellular carcinoma. Hepatology 35:519–524
Gozzetti G, Mazziotti A, Grazi GL et al (1993) Surgical experience with 168 primary liver cell carcinomas treated with hepatic resection. J Surg Oncol Suppl 3:59–61
Fuster J, García-Valdecasas JC, Grande L et al (1996) Hepatocellular carcinoma and cirrhosis. Results of surgical treatment in a European series. Ann Surg 223:297–302
Franco D, Capussotti L, Smadja C et al (1990) Resection of hepatocellular carcinomas. Results in 72 European patients with cirrhosis. Gastroenterology 98:733–738
Fong Y, Sun RL, Jarnagin W et al (1999) An analysis of 412 cases of hepatocellular carcinoma at a western center. Ann Surg 229:790–799; discussion 799–800.
Poon RT, Fan ST, Lo CM et al (2001) Improving survival results after resection of hepatocellular carcinoma: a prospective study of 377 patients over 10 years. Ann Surg 234:63–70
Liu JH, Chen PW, Asch SM et al (2004) Surgery for hepatocellular carcinoma: does it improve survival? Ann Surg Oncol 11:298–303
Makuuchi M, Hasegawa H, Yamazaki S (1985) Ultrasonically guided subsegmentectomy. Surg Gynecol Obstet 161:346–350
Takayama T, Makuuchi M (1996) Intraoperative ultrasonography and other techniques for segmental resections. Surg Oncol Clin N Am 5:261–269
Vauthey JN, Lauwers GY, Esnaola NF et al (2002) Simplified staging for hepatocellular carcinoma. J Clin Oncol 20:1527–1536
Llovet JM, Bru C, Bruix J (1999) Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis 19:329–338
Pawlik TM, Poon RT, Abdalla EK et al (2005) International Cooperative Study Group on Hepatocellular Carcinoma. Critical appraisal of the clinical and pathologic predictors of survival after resection of large hepatocellular carcinoma. Arch Surg 140:450–457
Nathan H, Schulick RD, Choti MA et al (2009) Predictors of survival after resection of early hepatocellular carcinoma. Ann Surg 249:799–805
Sheu JC, Sung JL, Chen DS et al (1985) Early detection of hepatocellular carcinoma by real-time ultrasonography: a prospective study. Cancer 56:660–666
Tinkle CL, Haas-Kogan D (2012) Hepatocellular carcinoma: natural history, current management, and emerging tools. Biologics 6:207–219
Bruix J, Sherman M (2011) Management of hepatocellular carcinoma: an update. Hepatology 53:1020–1022
Yao FY (2006) Should surveillance for hepatocellular carcinoma be increased in patients with cirrhosis and small liver nodules? Nat Clin Pract Gastroenterol Hepatol 3:544–545
Okamoto E, Yamanaka N, Toyosaka A et al (1987) Current status of hepatic resection in the treatment of hepatocellular carcinoma. In: Okuda K, Ishak KG (eds) Neoplasms of the liver. Springer-Verlag, Tokyo, pp 359–361
Shirabe K, Kanematsu T, Matsumata T et al (1991) Factors linked to early recurrence of small hepatocellular carcinoma after hepatectomy: univariate and multivariate analyses. Hepatology 14:802–805
Makuuchi M, Hasegawa H, Yamazaki S (1985) Ultrasonically guided subsegmentectomy. Surg Gynecol Obstet 162:346–350
Hsu HC, Shue JC, Lin YH et al (1985) Prognostic histologic features of resected small hepatocellular carcinoma (HCC) in Taiwan: a comparison with resected large HCC. Cancer 56:672–680
Kanai T, Hirohashi S, Upton MP et al (1987) Pathology of small hepatocellular carcinoma: a proposal for a new gross classification. Cancer 60:810–819
Ercolani G, Grazi GL, Ravaioli M et al (2003) Liver resection for hepatocellular carcinoma on cirrhosis: univariate and multivariate analysis of risk factorsfor intrahepatic recurrence. Ann Surg 237:536–543
Wakasa K, Sakurai M, Okamura J et al (1985) Pathological study of small hepatocellular carcinoma: frequency of their invasion. Virchows Arch A Pathol Anat Histopathol 407:259–270
Adachi E, Maeda T, Kajiyama K et al (1996) Factors correlated with portal venous invasion by hepatocellular carcinoma: univariate and multivariate analyses of 232 resected cases without preoperative treatments. Cancer 77:2022–2031
Kang CM, Choi GH, Kim DH et al (2010) Revisiting the role of nonanatomic resection of small (<or = 4 cm) and single hepatocellular carcinoma in patients with well-preserved liver function. J Surg Res 160:81–89
Yamamoto J, Kosuge T, Takayama T et al (1996) Recurrence of hepatocellular carcinoma after surgery. Br J Surg 83:1219–1222
Yamanaka N, Okamoto E, Fujihara S et al (1992) Do the tumor cells of hepatocellular carcinomas dislodge into the portal venous stream during hepatic resection? Cancer 70:2263–2267
Ueno S, Kubo F, Sakoda M et al (2008) Efficacy of anatomic resection vs nonanatomic resection for small nodular hepatocellular carcinoma based on gross classification. J Hepatobiliary Pancreat Surg 15:493–500
Yamamoto M, Takasaki K, Ohtsubo T et al (2001) Effectiveness of systematized hepatectomy with Glisson’s pedicle transection at the hepatic hilus for small nodular hepatocellular carcinoma: retrospective analysis. Surgery 130:443–448
Regimbeau JM, Kianmanesh R, Farges O et al (2002) Extent of liver resection influences the outcome in patients with cirrhosis and small hepatocellular carcinoma. Surgery 131:311–317
Tanaka K, Shimada H, Matsumoto C et al (2008) Anatomic versus limited nonanatomic resection for solitary hepatocellular carcinoma. Surgery 143:607–615
Dahiya D, Wu TJ, Lee CF et al (2010) Minor versus major hepatic resection for small hepatocellular carcinoma (HCC) in cirrhotic patients: a 20-year experience. Surgery 147:676–685
Nakashima Y, Nakashima O, Tanaka M et al (2003) Portal vein invasion and intrahepatic micrometastasis in small hepatocellular carcinoma by gross type. Hepatol Res 26:142–147
Takayama T, Makuuchi M, Hirohashi S et al (1998) Early hepatocellular carcinoma as an entity with a high rate of surgical cure. Hepatology 28:1241–1246
Kojiro M (2005) Histopathology of liver cancers. Best Pract Res Clin Gastroenterol 19:39–62
Lai EC, Ng IO, Ng MM et al (1990) Long-term results of resection for large hepatocellular carcinoma: a multivariate analysis of clinicopathological features. Hepatology 11:815–818
Okusaka T, Okada S, Ueno H et al (2002) Satellite lesions in patients with small hepatocellular carcinoma with reference to clinicopathologic features. Cancer 95:1931–1937
Kubo S, Taukamoto T, Hirohashi K et al (2003) Appropriate surgical management of small hepatocellular carcinomas in patients infected with hepatitis C virus. World J Surg 27:437–442. doi:10.1007/s00268-002-6475-5
Kubo S, Tanaka H, Takemura S et al (2007) Surgical treatment for hepatocellular carcinoma detected after successful interferon therapy. Surg Today 37:285–290
Hasegawa K, Kokudo N, Imamura H et al (2005) Prognostic impact of anatomic resection for hepatocellular carcinoma. Ann Surg 242:252–259
Roayaie S, Obeidat K, Sposito C et al (2013) Resection of hepatocellular cancer ≤2 cm: results from two western centers. Hepatology 57:1426–1435
Shindoh J, Hasegawa K, Inoue Y et al (2013) Risk factors of post-operative recurrence and adequate surgical approach to improve long-term outcomes of hepatocellular carcinoma. HPB (Oxford). 15:31–39
Ochiai T, Sonoyama T, Kikuchi S et al (2007) Anatomic wide hepatectomy for treatment of hepatocellular carcinoma. J Cancer Res Clin Oncol 133:563–569
Imamura H, Matsuyama Y, Tanaka E et al (2003) Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol 38:200–207
Sasaki A, Iwashita Y, Shibata K et al (2006) Preoperative transcatheter arterial chemoembolization reduces long-term survival rate after hepatic resection for resectable hepatocellular carcinoma. Eur J Surg Oncol 32:773–779
Chiappa A, Zbar AP, Audisio RA et al (2000) Factors affecting survival and long-term outcome in the cirrhotic patient undergoing hepatic resection for hepatocellular carcinoma. Eur J Surg Oncol 26:387–392
Kobayashi A, Miyagawa S, Miwa S et al (2008) Prognostic impact of anatomical resection on early and late intrahepatic recurrence in patients with hepatocellular carcinoma. J Hepatobiliary Pancreat Surg 15:515–521
Kamiyama T, Nakanishi K, Yokoo H et al (2012) Analysis of the risk factors for early death due to disease recurrence or progression within 1 year after hepatectomy in patients with hepatocellular carcinoma. World J Surg Oncol. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3407774/pdf/1477-7819-10-107.pdf
Shirabe K, Kajiyama K, Harimoto N et al (2009) Prognosis of hepatocellular carcinoma accompanied by microscopic portal vein invasion. World J Gastroenterol 15:2632–2637
Kamiyama T, Nakanishi K, Yokoo H et al (2010) theimpact of anatomical resection for hepatocellular carcinoma that meets the milan criteria. J Surg Oncol 101:54–60
Nanashima A, Tobinaga S, Kunizaki M et al (2010) Strategy of treatment for hepatocellular carcinomas with vascular infiltration in patients undergoing hepatectomy. J Surg Oncol 101:557–563
Sawada T, Kubota K, Kita J et al (2011) Clinical outcome of hepatectomy for hepatocellular carcinomas ≤2 cm. World J Surg 35:377–385. doi:10.1007/s00268-010-0851-3
Fujita N, Aishima S, Iguchi T et al (2011) Histologic classification of microscopic portal venous invasion to predict prognosis in hepatocellular carcinoma. Hum Pathol 42:1531–1538
Giuliante F, Ardito F, Pinna AD et al (2012) Liver Resection for Hepatocellular Carcinoma <3cm: results of an Italian Multicenter Study on 588 Patients. J Am Coll Surg 215:244–254
Takeishi K, Shirabe K, Muto J et al (2011) Clinicopathological features and outcomes of young patients with hepatocellular carcinoma after hepatectomy. World J Surg 35:1063–1071. doi:10.1007/s00268-011-1017-7
Shimada S, Kamiyama T, Yokoo H et al (2013) Clinicopathological characteristics and prognostic factors in young patients after hepatectomy for hepatocellular carcinoma. World J Surg Oncol 11:52
Kim JM, Kwon CH, Joh JW et al (2013) C-reactive protein may be a prognostic factor in hepatocellular carcinoma with malignant portal vein invasion. World J Surg Oncol 11:92
Shirabe K, Kajiyama K, Abe T et al (2009) Predictors of microscopic portal vein invasion by hepatocellular carcinoma: measurement of portal perfusion defect area ratio. J Gastroenterol Hepatol 24:1431–1436
Ohashi M, Wakai T, Korita PV et al (2010) Histological evaluation of intracapsular venous invasion for discrimination between portal and hepatic venous invasion in hepatocellular carcinoma. J Gastroenterol Hepatol 25:143–149
Shimada M, Rikimaru T, Hamatsu T et al (2001) The role of macroscopic classification in nodular-type hepatocellular carcinoma. Am J Surg 182:177–182
Utsunomiya T, Shimada M, Taguchi KI et al (2000) Clinicopathologic features and postoperative prognosis of multicentric small hepatocellular carcinoma. J Am Coll Surg 190:331–335
Yamamoto M, Takasaki K, Otsubo T et al (2004) Favorable surgical outcomes in patients with early hepatocellular carcinoma. Ann Surg 239:395–399
Sumie S, Kuromatsu R, Okuda K et al (2008) Microvascular invasion in patients with hepatocellular carcinoma and its predictable clinicopathological factors. Ann Surg Oncol 15:1375–1382
Nakashima T (1976) Vascular changes and hemodynamic in hepatocellular carcinoma. In: Okuda K, Peters RL (eds) Hepatocellular carcinoma. Wiley, New York, pp 169–203
Toyosaka A, Okamoto E, Mitsunobu M, et al (1996) Pathologic and radiographic studies of intrahepatic metastasis in hepatocellular carcinoma; the role of efferent vessels. HPB Surg 10:97–103; discussion 103–104.
Yamamoto M, Takasaki K, Yagawa A et al (1990) Cancer cells in the portal and hepatic veins of resected specimens of hepatocellular carcinomas. Gan No Rinsho 36:2123–2125 In Japanese
Makuuchi M, Hasegawa H, Yamazaki S (1981) Intraoperative ultrasonic examination for hepatectomy. Jpn J Clin Oncol 11:367–390
Acknowledgments
This work was supported in part by National Natural Science Fund for Young Scholars of China (81000177, Yuesi Zhong), National Natural Science Fund of China (81272642, Ruiyun Xu and 81470860, Yuesi Zhong) and Japan–China Sasakawa Medical Fellowship.
Conflict of interest
There is no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhong, Y., Deng, M. & Xu, R. Reappraisal of Evidence of Microscopic Portal Vein Involvement by Hepatocellular Carcinoma Cells with Stratification of Tumor Size. World J Surg 39, 1142–1149 (2015). https://doi.org/10.1007/s00268-014-2807-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2807-5