Abstract
Background
Breast magnetic resonance imaging (MRI) has shown high sensitivity in determining tumor extent, multifocality, and occult contralateral breast cancer. Low specificity, unnecessary mastectomies, and costs are arguments against MRI. The purpose of this study was to determine whether preoperative breast MRI would affect primary surgical management, reduce reexcision/reoperation procedures, and influence the choice of neoadjuvant treatment in patients with newly diagnosed breast cancer.
Methods
This prospective, randomized, multicenter study included 440 breast cancer patients younger than aged 56 years from three, Swedish, large-volume breast units. Patients were randomly allocated on a 1:1 basis to either preoperative staging with breast MRI (n = 220) or no breast MRI (n = 220) (control group). Treatment planning of all patients was discussed at multidisciplinary team conferences.
Results
In patients randomized to the MRI group, who had an observed higher percentage of planned breast-conserving surgery (BCS) compared with the control group, a change from suggested breast conservation to mastectomy occurred in 23 of 153 (15 %) patients. Breast MRI provided additional information in 83 of 220 (38 %) patients, which caused a change in treatment plan in 40 (18 %). The breast reoperation rate was significantly lower in the MRI group: 11 of 220 (5 %) versus 33 of 220 (15 %) in the control group (p < 0.001). The number of mastectomies, axillary reoperations, and the number of patients receiving neoadjuvant chemotherapy after definitive treatment did not differ significantly between the groups.
Conclusions
Preoperative staging with breast MRI in women younger than age 56 years altered the treatment plan in 18 % of the patients. Although a higher MRI-related conversion rate from breast conservation to mastectomy was found, the final numbers of mastectomies did not differ between the two groups. The breast reoperation rate in the MRI group was significantly reduced.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Triple assessment, including clinical, radiological (mammography and ultrasonography (US)), and cytological/histological examination is the “gold standard” for the evaluation of breast cancer. After preoperative workup, patients are presented at a multidisciplinary team conference (MDT), where tentative treatment plans are confirmed. Although these diagnostic modalities together will contribute to accurate staging in the majority of cases, false-negative results occur both in the detection and in the appreciation of the size of the lesion [1]. Conventional imaging modalities have proven inferior to diagnose lobular carcinomas and malignant lesions in dense breast tissue, more frequently found in young women and in women taking hormone replacement therapy [2, 3]. In order to obtain clear surgical margins, tumor mapping is essential, because involved margins may result in reexcision or conversion to mastectomy.
Breast magnetic resonance imaging (MRI) is currently not a standard diagnostic tool in primary breast cancer staging but can serve as a complement in the workup of complex cases with inconclusive mammography and US findings [4]. MRI is a highly sensitive diagnostic method with the ability to detect small tumors in dense breasts. It is considered to be cost-effective as a screening tool in young breast cancer gene mutation carriers [5–7]. MRI is also an adjunct in evaluating neoadjuvant treatment response [8].
Although the use of preoperative breast MRI is increasing, controversy still exists whether preoperative staging with breast MRI improves short-term surgical outcome. A recently published review confers that information gained from routine use of preoperative MRI causes “an unfavorable harm benefit ratio” [9].
The intention of this study was to investigate the value of breast MRI as a complement to triple assessment of breast cancer in young women. We presumed that women with dense breasts would benefit most from breast MRI, although breast density was not an inclusion criterion. Therefore, only women <56 years, most likely to be pre- or perimenopausal, were included.
The purposes of this trial were to evaluate whether breast MRI altered the surgical management, reduced the reexcision/reoperation rates, and if preoperative MRI would influence the decision to recommend neoadjuvant treatment.
Patients and methods
Women younger than age 56 years with newly diagnosed invasive and/or noninvasive breast cancer were included in this prospective, randomized, multicenter trial. Patients were recruited from three Swedish large-volume breast units Capio S:t Göran´s Hospital (Site A), Karolinska University Hospital (Site B), and Västmanland County Hospital (Site C). Sites A and B each diagnose and treat close to 500 primary breast cancers annually, whereas site C treats 250 breast cancers yearly. Study inclusion commenced on December 2007 at Sites A and B. Site C started inclusion in February 2009. The last study patient was included in March 2011. A total of 668 patients with both clinical and screen-detected cancers were considered eligible. The age limit was chosen to include women with an increased risk for multifocal and bilateral disease and with dense breast tissue [10]. Breast density according to Wolfe’s parenchymal pattern was recorded separately after study closure by one of the authors (GI) [11]. Exclusion criteria were previous malignant disease in the ipsilateral breast, pregnancy/lactation, kidney disease, metal implants, overweight and reduced mobility, claustrophobia, mental illness, and difficulties in comprehension of the study.
Diagnosis was confirmed with fine-needle aspiration cytology or with core-needle biopsy. Nonpalpable tumors were indicated by US-guided tattooing using a carbon suspension or by US-guided needle wire localization. If not visible on US, stereotaxic tumor indication was performed with either carbon technique or hook wires. Subsequently, individual treatment recommendations were confirmed during a weekly MDT. The choice of primary surgical treatment was based on tumor stage, tumor size in relation to the breast size, and biological characteristics of the tumor, as well as patient preferences. Patients with lymph node metastases were eligible for neoadjuvant treatment and participated in neoadjuvant chemotherapy studies. Tumor size was not a prime determinant for neoadjuvant treatment, but tumor size in relation to the breast size was taken into account. Sentinel node biopsy was performed according to national guidelines and axillary lymph node dissection was done in the case of micro and/or macrometastases.
Demographic data and clinical information were collected retrospectively from medical records. Details regarding all image findings (mammography, US, and/or breast MRI), such as presence/absence of multifocality, altered tumor extent, contralateral findings, and pathological lymph nodes, were registered.
Randomization
Eligible patients were asked to participate in the study by the breast surgeon when the cancer diagnosis was confirmed. Written, informed consent was obtained from all participants. Patients entered the trial by means of a telephone call to the randomization center (Regional Oncological Center, Stockholm) made by either the breast nurse specialist or by the surgeon. A computer-generated algorithm was used for randomization and patients were assigned to preoperative breast MRI or no MRI (control group) on a 1:1 basis. The clinical pathway differed somewhat between the units, but in most cases the randomization took place after disclosure of cancer diagnosis and before the pretreatment MDT. A minority of patients were randomized after pretreatment MDT. Subsequently patients’ inclusion in the trial was stated in the clinical chart.
MRI procedures
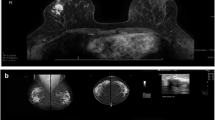
The MRI examinations were performed at Sites A and C. No MRI examinations were performed at Site B. MRI examinations at Site A were performed on a 1.5T MRI system (Signa HDxt®, GE Healthcare). All examinations were performed in the prone position using an 8-channel breast coil. The imaging protocol included a STIR sequence in the axial plane followed by fat-saturated, T1-weighted, contrast-enhanced, dynamic scans (Vibrant® Multi-Phase sequence) in the sagittal plane repeated seven times (including a precontrast sequence) with 90-s time interval. The dynamic sequences were then immediately followed by a fat-saturated, T1-weighted, high-resolution, 3D sequence in the axial plane. Omniscan® (GE Healthcare) gadolinium contrast material was used with 0.2 ml/kg power injected at 3 ml/s. At Site C, the MRI examinations were performed using a 1.5T MRI system (Symphony, Siemens VA30). All examinations were performed in the prone position using a 4-channel breast coil. The precontrast imaging protocol included STIR and T2-weighted sequences in the axial plane and a non-fat-saturated T1-weighted sequence in the coronary plane. The contrast-enhanced, dynamic scans were acquired in the axial plane using a fat-saturated, T1-weighted, multiphase sequence (Vibe®), repeated seven times (including a precontrast sequence) with a 90-s time interval. Dotarem® (Guerbet) gadolinium contrast material was used with 0.2 ml/kg power injected at 2 ml/s. Postprocessing of all contrast-enhanced dynamic scans performed at Site A was performed using a breast MRI computer-aided evaluation software (CADstream, version 4.1 Confirma®). No such aid was used at Site C.
Further diagnostic workup
Patients underwent breast MRI within 2 weeks of randomization at Site A or Site C. If breast MRI findings were consistent with the diagnostic findings before MRI, the initial treatment plan was implemented and the patient was informed of the result by telephone call or letter. Incremental MRI findings, BI-RADS 3 or more were further investigated and included altered tumor extent, multifocality, contralateral lesions, or atypical lymph nodes. Altered tumor extent referred to a larger or smaller tumor detected with MRI compared with mammography/US findings. A size difference more than 1 cm was chosen as a cutoff value. Multifocality was defined as multiple tumors separated from each other, regardless of the distance between each lesion. In the majority of incremental findings, a second-look US examination was performed that targeted the lesion in question and if identified, US-guided tissue sampling was made for confirmation. In October 2009, MRI-guided biopsy was introduced at Site A, but only three patients had this procedure within the study. In a few cases, a second breast-MRI for follow-up was recommended within 3–6 months of primary treatment.
Patients with new information from breast MRI were discussed at a second pretreatment MDT where appropriate amendments were made. Patients allocated to the control group were planned for no further imaging in addition to mammography and US (Fig. 1).
Surgical procedure and specimen handling
The goal was to excise the tumor with macroscopic margins of at least a 10 mm. After BCS tumor specimen X-ray/US was routinely performed. Sentinel node biopsy was sent for frozen-section analysis. The excised tumor was submitted for postoperative histopathological processing.
All patients were discussed during the postoperative MDT. Clear margins were defined as tumor not touching the inked surface for invasive breast carcinomas. In DCIS cases, according to Swedish guidelines, grade and postoperative therapy decided whether margins ≤10 mm should be accepted [12]. If equivocal tumor margins, e.g., when the pathologists could not secure clear margins for instance due to fragmented fatty breast tissue, tumor extent and tumor biology was taken into consideration and would impact the decision to reexcise or perform a mastectomy or not to reoperate. Axillary lymph node clearance was recommended to those who had lymph node micro or macrometastases not previously detected [13, 14]. Postoperative adjuvant treatment recommendations followed national or regional treatment guidelines [12, 15].
The Regional Ethical Review Board in Stockholm approved the study, Dnr 2007/4:8, 2008/2020-32, and 2009/224-32.
Statistics
With the assumption that 10 % of MRI examinations would provide new information leading to a change in management, the number of patients needed in the study was estimated to be 440. The power calculation is supported by data from a study that included 267 patients where breast MRI altered planned surgical management in 26 % of patients [16].
The main findings are presented with descriptive statistics of estimated proportion subdivided for randomization groups. Pearson’s Chi-square test was used for the following calculations: testing the hypothesis of equal distribution of planned treatment between randomization groups, testing if the proportion of altered clinical treatment differed between the two study groups, and testing if the proportion of reoperations differed after performed surgery between randomization groups. Odds ratio and 95 % intervals were calculated for the chances of a breast reoperation and conversion to mastectomy for a subset of patients initially scheduled for breast-conserving surgery. A p value <0.05 was considered statically significant. Analysis was not adjusted for surgical method. All analyses were performed with IBM SPSS Statistics version 20.
Role of the funding sources
The sponsors of the trial financed all breast MRI examinations but had no role in the study design, data collection, data analyses, or in the writing of the manuscript.
Results
A total of 440 women entered the trial: 211 at Site A, 167 at Site B, and 62 patients at Site C. Two hundred twenty patients were randomized to the breast MRI group and 220 to the control group. Ten subjects randomized to MRI never underwent this study but were included in the MRI group according to the intention-to-treat principle (Fig. 1). Baseline characteristics are shown in Table 1.
Pre-randomization treatment planning
Patients randomized to the MRI group had a significantly higher rate of planned BCS (153/220, 70 %) compared with the control group (132/220, 60 %). However, the overall distribution of planned treatment (type of surgery/neoadjuvant chemotherapy) and further diagnostic workup in the two groups before randomization did not differ significantly.
MRI results
In 83 of 220 patients (38 %), breast MRI revealed incremental information. The additional findings are listed in Table 2. As a consequence, 56 patients underwent targeted second-look US. In 44 patients, the lesions were detected and a biopsy performed. Four patients required second-look MRI and three were biopsied. Eleven patients with MRI-detected lesions repeated MRI after 3–6 months. No further investigations were required nor changes in treatment plans occurred for the remaining 12 patients. There was no significant difference in menopausal status or breast density between the subsets of patients with or without incremental MRI findings. Time from diagnosis to primary treatment was equal in both groups; thus MRI did not prolong waiting time.
Altered treatment
In the MRI group, patients primarily scheduled for BCS showed a significantly higher rate of conversion to mastectomy as final treatment; 30 of 153 (20 %) compared with 13 of 132 (10 %) in the control group (odds ratio = 2.3; 95 % confidence interval [CI] 1.1–4.5; p = 0.024; Appendix). Six patients not originally planned for neoadjuvant chemotherapy were allocated to chemotherapy preoperatively, whereas one patient planned for neoadjuvant chemotherapy received surgery as primary treatment (Table 3).
Altered treatment due to MRI findings occurred in 40 of 220 (18 %) patients (Table 4). Twenty-two patients converted from BCS to mastectomy and 15 patients underwent axillary clearance instead of sentinel node biopsy. One of these converted from mastectomy to BCS. As a consequence of MRI findings, three patients received neoadjuvant chemotherapy instead of surgery as primary treatment and one patient received a mastectomy instead of neoadjuvant chemotherapy. Contralateral findings were described in 24 of 220 patients, which resulted in four unanticipated contralateral BCS and two mastectomies. In the remaining 43 of 83 patients, MRI findings did not alter the primary treatment plan. For both study groups, altered pre-randomization planning also could be due to results of further diagnostic workup with mammography and UL or patients’ preferences (Table 3).
Reoperation rates
The overall breast reoperation rate in the MRI group was significantly lower than in the control group (p < 0.001). The ipsilateral breast reoperation rate was 11 of 220 (5 %) and 33 of 220 (15 %) respectively in the two groups. One patient in the MRI group underwent reexcision in the contralateral breast, which is not included in the calculation. Two patients in the control group were reoperated twice in the ipsilateral breast, and one of these patients also needed a repeated procedure in the contralateral breast. No significant difference in axillary reoperation rates between the groups was found.
Reoperation rates after BCS
The reoperation rates in the subset of patients initially planned for BCS were 8 of 153 (5 %) in the MRI group and 29 of 132 (22 %) in the control group (p < 0.0001).
Definitive treatment
BCS rates were 123 of 220 (56 %) in the MRI group and 129 of 220 (59 %) in the control group, and the mastectomy rates were 43 and 41 % respectively. Of those 29 and 28 patients in each group receiving neoadjuvant chemotherapy, 3 and 2 patients respectively with metastatic disease never had surgery (Fig. 1).
Discussion
In this study, preoperative breast MRI did provide additional information: both in the ipsi- and the contralateral breast and in the axilla that altered the surgical management in 18 %. An increased number of patients planned for BCS received mastectomy after MRI and fewer reoperations occurred in this group. Neoadjuvant chemotherapy rates were similar in both groups. Until now, only two randomized studies have assessed the efficacy of breast MRI regarding the surgical outcome in women with newly diagnosed breast cancer [17, 18]. Both trials failed to show any additional benefit of breast MRI to standard assessment.
This trial is the third randomized, prospective study. It specifically selected young women with symptomatic and screen-detected breast cancer, younger than age 56 years, where breast MRI is supposed to have the greatest impact. Because it is difficult to ascertain the influence of sex hormones on breast density on an individual level, pre- as well as perimenopausal women were included. The number of planned BCS was higher in the MRI group than in the control group: 153 versus 132. Because both groups were evenly distributed concerning age, menopausal status, screen detected cancer, breast density, and mammographic tumor extent the main reason for the unbalance is assumed to be related to chance. Tumor size in relation to breast volume was not analyzed. At pretreatment MDT, most patients’ participation in preoperative MRI of the breast (POMB) was known, but the allocated treatment arm was unknown in the vast majority of cases. It could not be ruled out that the unblinded randomization design could have influenced the unbalanced planned treatment. The higher number of planned BCS in the MRI group per se, increased the risk for reoperation in the MRI group, but the breast reoperation (reexcision/mastectomy conversion) rate in this group was found to be significantly lower than in the control group. The final numbers of mastectomies were equal in both study groups as was the proportion of patients receiving neoadjuvant treatment.
The results presented in our study are contradictory to prior randomized studies. The COMICE trial included women with biopsy verified breast cancer; all planned for BCS with reexcision rates as study endpoint. Reoperation rates were not significantly lower in the MRI group. The authors of the COMICE trial pointed to limitations in their study, e.g., its inclusion of patients from a number of small centers where technical factors and varying degree of experience among involved radiologists could have influenced the MRI results [17].
In the MONET trial, the second, randomized, controlled trial, only patients with nonpalpable BI-RADS 3-5 lesions were included and randomized to MRI or to no MRI in addition to standard assessment. The MONET trial assessed the reexcision rates after primary surgery. The number of reexcisions in that study was paradoxically higher in the MRI group compared with the control group. The number of mastectomies did not differ between the groups. The MONET trial could be questioned for being underpowered, as only one third of the included patients had confirmed malignant lesions, whereas in the POMB study all randomized patients had a verified cancer diagnosis.
A limitation of the present study is that not all MRI-detected lesions were biopsy-proven, which is strongly favored by Kuhl et al. [19]. The reason is that the result of the biopsy would not have changed the type of surgery performed in these cases. US-guided tissue sampling was used in two thirds of the patients with new information from MRI when the result could influence further treatment. Only a few patients underwent MRI-guided biopsies, because the method was available only during the late part of the study. The additional MRI information led to a reduction of planned BCS and increased the number of mastectomies, which in turn reduced the reoperation rate.
A meta-analysis of nonrandomized studies assessing the impact of preoperative breast MRI on surgical management by Houssami et al. implies that more extensive, unnecessary surgery is performed in patients due to MRI, thus corroborating the COMICE but not the MONET trial [9]. Our data support that preoperative breast MRI as an adjunctive image modality affects the clinical management in women with breast cancer who are younger than age 56 years. The additional information gained from preoperative MRI in relation to histopathological results, disease-free survival, and health-related economic consequences will be addressed in future studies.
Conclusions
Although a higher MRI-related conversion rate from breast-conserving surgery to mastectomy was found, the final numbers of mastectomies did not differ between the two groups. Furthermore, preoperative staging with breast MRI was significantly associated with a reduced in-breast reoperation rate.
References
Drew P, Turnbull L, Chatterjee S et al (1999) Prospective comparison of standard triple assessment and dynamic magnetic resonance imaging of the breast for the evaluation of symptomatic breast lesion. Ann Surg 230(5):680
Rodenko GN, Harms SE, Pruneda JM et al (1996) MR imaging in the management before surgery of lobular carcinoma of the breast: correlation with pathology. Am J Roentgenol 167(6):1415–1419
Carney P, Miglioretti D, Bonnie C et al (2003) Individual and combined effects of age, breast density, and hormone replacement therapy use on the accuracy of screening mammography. Ann Intern Med 138:168–175
Van Goethem M, Tjalma W, Schelfout K et al (2006) Magnetic resonance imaging in breast cancer. Eur J Surg Oncol 32(9):901–910
Berg WA, Gutierrez L, NessAiver MS et al (2004) Diagnostic accuracy of mammography, clinical examination, US and MR imaging in preoperative assessment of breast cancer. Radiology 233:830–849
Plevritis SK, Kurian AW, Sigal BM et al (2006) Cost-effectiveness of screening BRCA1/2 mutation carriers with breast magnetic resonance imaging. JAMA 295(20):2374–2384
Saslow D, Boetes C, Burke W et al (2007) American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin 57(2):75–89
Atkins JJ, Appleton CM, Fisher CS et al (2013) Which imaging modality is superior for prediction of response to neoadjuvant chemotherapy in patients with triple negative breast cancer? J Oncol 2013:964863
Houssami N, Turner R, Morrow M (2013) Preoperative magnetic resonance imaging in breast cancer meta-analysis of surgical outcomes. Ann Surg 257:249–255
Checka CM, Chun JE, Schnabel FR et al (2012) The relationship of mammographic density and age: implication for breast cancer screening. Am J Roentgenol 198(3):292–295
Wolfe JN, Albert S, Belle S et al (1983) Brest parenchymal patterns and their relationship to risk for having or developing carcinoma. Radiol Clin North Am 21:127–136
Bergkvist L, Frisell J, Swedish Breast Cancer Group, Swedish Society of Breast Surgeons (2005) Multicentre validation study of sentinel node biopsy for staging in breast cancer. Br J Surg 92(10):1221–1224
Andersson Y, Frisell J, Sylvan M et al (2013) Causes of false-negative sentinel node biopsy in patients with breast cancer. Br J Surg 100(6):775–783
Bedrosian I, Mick R, Orel SG et al (2003) Changes in the surgical management of patients with breast carcinoma based on preoperative magnetic resonance imaging. Cancer 98(3):468–473
Turnbull L, Brown S, Harvey I et al (2010) Comparative effectiveness of MRI in breast cancer (COMICE) trial: a randomised controlled trial. Lancet 375:563–571
Peters NH, van Esser S, van den Bosch MA et al (2011) Preoperative MRI and surgical management in patients with nonpalpable breast cancer: the MONET—randomised controlled trial. Eur J Cancer 47(6):879–886
Kuhl C, Kuhn W, Braun M et al (2007) Pre-operative staging of breast cancer with breast MRI: one step forward, two steps back? Breast 16:S34–S44
Acknowledgments
The authors thank the medical staff and surgeons at the breast units for the inclusion of patients. Particular thanks to: Anders Adolfsson, Åsa Aspelin, Jan Frisell, Eva Frodis, Eva Hagel, Henry Letocha, Katrina Thingvall, and Birgitte Wilczek. The work was supported by stipends and Grants from, Capio St Göran´s Hospital Research Foundation, Center for Clinical Research, CKF, Uppsala University, Västerås, Johan & Jakob Söderberg Foundation, King Gustaf V’s Jubilee Foundation, Paula Brunetti Jacovone Foundation, Independent Order of Odd Fellow Stockholm, Percy Falk Foundation, Stockholm County Council, Swedish Surgical Society, The Swedish Breast Cancer Association (BRO), Västmanland County Council
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Appendix
Rights and permissions
About this article
Cite this article
Gonzalez, V., Sandelin, K., Karlsson, A. et al. Preoperative MRI of the Breast (POMB) Influences Primary Treatment in Breast Cancer: A Prospective, Randomized, Multicenter Study. World J Surg 38, 1685–1693 (2014). https://doi.org/10.1007/s00268-014-2605-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2605-0