Abstract
Background
Multiple trauma continues to have a high incidence worldwide. Trauma is the leading cause of death among people between the ages of 10 and 40. The Advanced Trauma Life Support (ATLS) is the most widely accepted method for the initial control and treatment of multiple trauma patients. It is based on the following hypothesis: The application of the ATLS program may reduce preventable or potentially preventable deaths in trauma patients.
Materials and methods
The present article reports a retrospective study based on the records of prospectively evaluated trauma patients between January 2007 and December 2012. Trauma patients over the age of 18 admitted to the critical care unit or patients who died before hospital admission were included. A multidisciplinary committee looked for errors in the management of each patient and classified deaths into preventable, potentially preventable, or nonpreventable. We recorded the number of specialists at our center who had received training in the ATLS program.
Results
A total of 898 trauma patients were registered. The mean injury severity score was 21 (SD 15), and the mortality rate was 10.7 % (96 cases). There were 14 cases (14.6 %) of preventable or potentially preventable death. The main errors were delay in initiating suitable treatment and performing a computed tomography scan in cases of hemodynamic instability, followed by initiation of incorrect treatment or omission of an essential procedure. As the number of ATLS-trained professionals increases, the rates of potentially preventable or preventable death fall.
Conclusions
Well-founded protocols such as the ATLS can help provide the preparation health professionals need. In our hospital environment, ATLS training has helped to reduce preventable or potentially preventable mortality among trauma patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Multiple trauma continues to have a high incidence worldwide [1]. In developed countries, trauma is the leading cause of death among people between the ages of 10 and 40. Nine people die every minute after violent injuries, and car accidents cause more than a million deaths a year worldwide [1]. Moreover, mortality is not the only problem: Donald Trunkey’s claim, “for every death, two patients remain permanently disabled” [2], first published in 1982, holds true today.
Epidemiological studies predict a progressive increase in traumatic injuries by the year 2030 [3]. These kinds of injuries involve a considerable loss in terms of years of productive life, and they raise health care costs and disability rates; besides the undeniable human drama, they also have a significant socio-economic impact [4].
In an effort to stem this upward trend, the use of a standardized and widely accepted method for the initial control of multiple trauma patients and for the establishment of treatment priorities is essential. Today, the Advanced Trauma Life Support (ATLS) protocol is the most widely accepted method worldwide for the initial control and treatment of multiple trauma patients [5].
Since the adoption of the protocol, investigators have published the results obtained in several countries and have compared mortality rates in trauma patients before and after the application of ATLS. In 1992, in a study in Trinidad and Tobago, Ariyanayagam et al. [6] observed a decrease in mortality from 49 to 46 % after applying the ATLS method and in the following year Ali et al. [7], in the same country, recorded a reduction in mortality associated with traumatic injury from 67.5 to 33.5 %. In 2003, in the Netherlands, Van Olden et al. [8] reported a decrease in mortality from 48 to 31 % after applying the ATLS method; a year later, studying mortality in the first 60 min after the patient’s arrival at the hospital, the same group observed a fall from 24 to 0 % [9].
The morbidity and mortality in trauma patients treated according to the ATLS protocol in conjunction with other methodologies have also been analyzed. Hashmi et al. [10] assessed the risk of complications and mortality before and after applying several approaches, including ATLS, and reported a lower rate of complications and mortality after the introduction of those protocols. Analyzing the implementation of several criteria included in the ATLS at rural level in the United States, Hedges et al. [11] found an increase in survival among the most severely injured patients.
In Catalonia, Spain, one study [12] of the application of clinical indicators in the treatment of multiple trauma patients based on the ATLS protocol found a reduction in complications, but not in mortality. A retrospective study in Greece [13] published in 2011 concluded that patients attended by physicians trained in ATLS presented higher mortality (3.7 vs 2 %). However, that study had clear methodological shortcomings. In 2009, a Cochrane review [4] found no articles that met the quality criteria for comparing results before and after introduction of the ATLS training program. The review concluded that there was no evidence that the method improves prognosis of multiple trauma patients.
In the light of these conflicting results, the present study was carried out to test the hypothesis that the application of the ATLS program may reduce the occurrence of avoidable errors. The use of the ATLS method provides a systematic approach to treatment and establishes priorities that support better outcomes for trauma patients. The ATLS method optimizes the treatment of trauma patients and helps reduce avoidable treatment errors or oversights, that could lead to preventable or potentially preventable deaths. Trauma represents the “perfect storm” for the development of collateral damage. The need to make rapid decisions, the impossibility of completing a full medical record, and the limited availability of human and material resources are among the main causes of error in the treatment of these patients. The aim of the present study was to analyze whether training in the ATLS protocol reduces preventable or potentially preventable mortality in trauma patients.
Materials and methods
This retrospective study is based on the records of prospectively evaluated trauma patients between January 2007 and December 2012. The study was performed in a tertiary care center in Catalonia, Spain. In Spain there are three care levels, defined according to the degree of complexity of available medical care. A tertiary level hospital is the highest level. In Catalonia, in addition to institutions at the three care levels, there are also referral centers for trauma patients. Our hospital is such a referral center, although it is not characterized as a trauma center because there are no such facilities in our country.
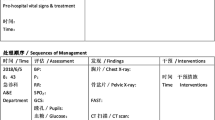
All multiple trauma patients over the age of 18 admitted to the critical care unit were included, as were those who died before hospital admission. The following variables were recorded for each case: age, gender, mechanism of injury, injury severity score (ISS) [14], revised trauma score (RTS) [15], prehospital and hospital vital signs (blood pressure, heart rate, respiratory rate, glasgow coma scale, temperature and oxygen saturation), laboratory tests (leukocytes, hemoglobin, prothrombin time, glycemia, lactic acid and base excess), diagnosis and treatment of each injury, complications, and outcome. In case of death, the date and the cause were specified.
A multidisciplinary committee of anesthesiologists, surgeons, intensivists, neurosurgeons, and radiologists looked for errors in the management of each patient and possible missed injuries. The majority of committee members were ATLS course instructors who had not been directly involved in patient treatment.
To analyze each case we used clinical information from medical and nursing reports, constant register clinics, lab reports, the radiology report, and the therapeutic report. The analysis was done by following a similar method to nominal group technique.
On the basis of the analysis of the errors, deaths were classified into three groups: preventable, potentially preventable, or nonpreventable. Preventable death was defined as death that would have been avoided if an error had not been made. Potentially preventable death presented an error, but it was impossible to establish whether death would have occurred in any case. Nonpreventable death was defined as death that would have occurred whether or not there were errors in patient management. Using data provided by the Spanish Association of Surgeons, we recorded the number of specialists at our center who had received training in the ATLS program and also the year in which they attended the course.
Statistical analysis
Data for each patient were recorded prospectively and introduced into a Microsoft ACCESS database in protected format to prevent the entry of erroneous or out of range data. Continuous data were described as means and standard deviation, and analyzed with Student’s t test if the distribution was normal or with nonparametric methods otherwise. Discontinuous data were presented as percentages and were analyzed by the Chi square or Mantel–Haenszel test, if there were more than two ordered categories. p scores of <0.05 were considered significant. No corrections were made for multiple analyses. The IBM SPSS Statistics 21.0 program was used for statistical calculation.
Results
We registered 898 trauma patients. Most patients were male (76 %) with a mean age of 45 (SD 64) years and had suffered blunt trauma (93.5 %). The mean ISS was 21 (SD 15), and the mortality rate was 10.7 % (96 cases) (Table 1). The 96 patients who died had a mean ISS of 42 (SD 24), significantly higher (p < 0.001) than the mean total score for the series. Most were men (68 %) with a mean age of 55 years, and almost all (99 %) had suffered blunt trauma (Table 1). There were 14 cases (14.6 %) of preventable or potentially preventable death. The remaining 82 deaths (85.4 %) were nonpreventable (Table 1). Patients with preventable or potentially preventable death were also mainly men (64 %) with a mean age of 52 years. All had blunt trauma. Mean ISS was 42 (SD 16); there were no differences with respect to the total group of patients who died (Table 1).
The main cause of death in the whole series was neurological (43 cases, 44.8 %), followed by hypovolemic shock (27 cases, 28.1 %) (Table 1). The main cause of death in patients with preventable or potentially preventable death was hypovolemic shock (10 cases, 71.4 %). There was a significant difference with respect to the overall group (p = 0.027), in which, as mentioned, the main cause of death was neurological. One patient with preventable or potentially preventable death died of respiratory causes due to uncontrolled pain, and three died of neurological causes due to delay or failure to perform the required neurosurgical intervention (Table 1).
Of the 14 patients with preventable or potentially preventable death, 12 cases were preventable and two were potentially preventable. All other deaths (82) were nonpreventable; in 34 of them (41.4 %), errors were made during patient management (Table 2).
The main errors in the management of the trauma patients who died were delay in initiating suitable treatment and performing a computed tomography (CT) scan in cases of hemodynamic instability. The frequency of these errors was similar across groups (preventable, potentially preventable, or nonpreventable) (Table 3).
In the preventable or potentially preventable mortality groups, the second most frequent type of error was initiation of incorrect treatment or omission of an essential procedure. In the nonpreventable death group, the second most common type of error was failure to perform a chest X-ray or pelvic X-ray during the primary survey, or failure to perform a focused assessment with sonography for trauma (FAST) scan when required (Table 3).
According to data provided by the Spanish Association of Surgeons, the number of specialists at our hospital with ATLS accreditation has increased significantly since 2007. As the number of ATLS-trained professionals increases, the rates of potentially preventable or preventable death fall (Fig. 1).
Discussion
Our series comprised 898 multiple trauma patients with a mean ISS of 21.3 and a mortality of 10.7 %. These figures are similar to those published in previous studies, which record mortality rates of 10 % for ISS ≤ 15 and up to 20 % for ISS ≥ 15 [16–19]. Patients who died had significantly higher mean ISS than the series as a whole (42 vs 21.3), but the ISS did not differ significantly between the different types of mortality (preventable, potentially preventable, and nonpreventable; see Table 1).
Fourteen patients (14.6 %) presented preventable or potentially preventable mortality. A review of trauma patients reported figures for preventable or potentially preventable mortality ranging from 0.4 to 39.6 % [20]. Figures ≤2 % have been quoted as acceptable for high-level trauma centers [21]; one study at a high-level trauma center with a large number of case studies (2,594 cases) reported a preventable mortality rate of 2.5 % [22]. Our results are not comparable because our study sample (96 patients) is much smaller, although obviously a high-level trauma center will have greater experience in treating these patients. A European study [23] with a similar number of cases to ours (62 deaths) obtained figures of preventable or potentially preventable mortality of 29 %, although the number of cases of preventable mortality was considerably lower than ours.
In the group of patients as a whole, the main cause of death was neurological, followed by hypovolemic shock and multiorgan failure. When mortality is preventable or potentially preventable, the leading cause of death is significantly different, with hypovolemic shock being the most frequent event (Table 1). These data are in agreement with those reported in other studies: the main cause of error associated with preventable or potentially preventable death is hemorrhage control [22, 24, 25].
The main errors recorded in our study were delay in initiating suitable treatment and in performing computed tomography in patients with hemodynamic instability. These were common to all types of mortality, and they also corroborate results reported in previous reports [22, 24, 25]. Most errors occur in the primary survey, during the ABC stage of the ATLS protocol. Other errors, such as inadequate treatment of an unstable patient, are also observed in all series [22, 24, 25].
As noted in the Introduction, there are no methodologically high-quality studies that affirm that implementation of the ATLS protocol [4] improves the prognosis of patients with multiple trauma. Nevertheless, physicians in many countries receive ATLS training in order to be able to treat these patients. The present study demonstrates that ATLS training has a positive impact on trauma patient outcomes. Although there are some limitations of the study, we can see that as the number of physicians with ATLS accreditation at our center increases, our data reflect clinically significant improvements, with a marked decrease in preventable and potentially preventable deaths (Fig. 1).
In some articles [10, 11] the improvement observed in the treatment of these patients is not attributable to the application of the ATLS protocol alone, but to its combination with other methodologies. At our center, apart from the progressive increase in staff with ATLS accreditation, there were no other changes in the management of multiple trauma patients during the study period. Trauma patients are always treated in a specific bay by a multidisciplinary medical team led by a team leader; an alarm code is used to alert the entire team, usually before the patient’s arrival in hospital, and chest and pelvis radiography are available in the bay without having to move the patient. A FAST scan, radiology and interventional radiology are available 24 h a day, 365 days a year. Multiple trauma sessions are held monthly, and patients are registered prospectively in a protected database. The updates of the protocols for the treatment of these patients have always been based on ATLS principles. So we can attribute the improvement in preventable and potentially preventable mortality to the application of the ATLS protocol.
Our current rate of preventable or potentially preventable mortality is 5.3 %, close to the rate recommended for high-level trauma centers [21]. The progressive reduction in these rates was achieved by avoiding errors during in the management of hypovolemic shock through the application of the systematic method and priorities described in ATLS.
In our view, it is very important that health professionals who are occasionally required to treat multiple trauma patients should have a clear idea of the procedures they should follow. In the case of professionals who routinely treat these patients in well-equipped facilities this is absolutely essential. We believe that clear, well-founded protocols such as ATLS can help to provide the preparation needed. In our hospital, ATLS training has helped to reduce preventable or potentially preventable mortality among trauma patients.
References
World Health Organization (2008) World report on road traffic injury prevention. Department of Injuries and Violence Prevention, World Health Organization
Trunkey DD (1982) On the nature of things that go bang in the night. Surgery 92:123–132
Mathers CD, Loncar D (2006) Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 3(11):e442
Jayaraman S, Sethi D (2009) Advanced trauma life support training for hospital staff. Cochrane Database Syst Rev 15(2):CD004173
American College of Surgeons (2012) Advanced Trauma Life Support (ATLS), vol 9. American College of Surgeons Committee on Trauma, Chicago
Ariyanayagam DC, Naraynsingh V, Maraj I (1992) The impact of the ATLS course on traffic accident mortality in Trinidad and Tobago. West Indian Med J 41:72–74
Ali J, Adam R, Butler AK et al (1993) Trauma outcome improves following the Advanced Trauma Life Support Program in a developing country. J Trauma 34:890–899
Van Olden GD, Meeuwis JD, Bolhuis HW et al (2004) Advanced trauma life support study: quality of diagnostic and therapeutic procedures. J Trauma 57:381–384
Van Olden GD, Meeuwis JD, Bolhuis HW et al (2004) Clinical impact of advanced trauma life support. Am J Emerg Med 22:522–525
Hashmi ZG, Haider AH, Zafar SN et al (2013) Hospital-based trauma quality improvement initiatives: first step toward improving trauma outcomes in the developing world. J Trauma Acute Care Surg 75:60–68
Hedges JR, Adams AL, Gunnels MD (2002) ATLS practices and survival at rural level III trauma hospitals, 1995–1999. Prehosp Emerg Care 6:299–305
Navarro S, Koo M, Orrego C et al (2013) Estudio para la mejora de la atención hospitalaria inicial del patient politraumatizado: proyecto TRAUMACAT. Med Clin. doi:10.1016/j.medcli.2013.07.001
Drimousis PG, Theodorou D, Toutouzas K et al (2011) Advanced Trauma Life Support certified physicians in a non trauma system setting: is it enough? Resuscitation 82:180–184
Baker SP, O’Neill B, Haddon W et al (1974) The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 14:187–196
Champion HR, Sacco W, Copes WS et al (1989) A revision of the trauma score. J Trauma 29:623–662
Cooper A, Hannan E, Bessey P et al (2000) Examination of the volume–mortality relationship for New York State Trauma Centers. J Trauma 48:16
Füglistaler-Montali I, Attenberger G, Füglistaler P et al (2009) In search of benchmarking for mortality following multiple trauma: a Swiss trauma center experience. World J Surg 33:2477–2489. doi:10.1007/s00268-009-0193-1
Sampalis JS, Lavoie A, Boukas S et al (1995) Trauma center designation: initial impact on trauma-related mortality. J Trauma 39:232–239
Champion H, Copes W, Sacco W et al (1990) The Major Trauma Outcome Study: establishing national norms for trauma care. J Trauma 30:1356–1365
Constanti CH, Domingues C, de Sousa RMC et al (2012) Preventable trauma deaths. Rev Saúde Pública 46:2
Hoyt DB, Coimbra R (2007) Trauma systems. Surg Clin North Am 87:21–35, v–vi
Gruen RL, Jurkocich GJ, McIntyre LK et al (2006) Patterns of errors contributing to trauma mortality. Lessons learned from 2594 deaths. Ann Surg 244:371–380
Saltzherr TP, Wendt KW, Nieoboer P et al (2011) Preventability of trauma deaths in a Dutch Level 1 trauma centre. Injury 42:870–873
Ivatury RR, Guilford K, Malhotra AK et al (2008) Patient safety in trauma: maximal impact management errors at a level I trauma center. J Trauma 64:265–270
Teixeira PGR, Inaba K, Hadjizacharia P et al (2007) Preventable or potentially preventable mortality at a mature trauma center. J Trauma 63:1338–1346
Acknowledgments
The authors are grateful to Ana López Carballedo of the Spanish Association of Surgeons, and Laura Moya Forés; special thanks are also due to Rosa Jam and Lluïsa Aguilà.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Navarro, S., Montmany, S., Rebasa, P. et al. Impact of ATLS Training on Preventable and Potentially Preventable Deaths. World J Surg 38, 2273–2278 (2014). https://doi.org/10.1007/s00268-014-2587-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2587-y