Abstract
Background
Femoral hernias are frequently operated on as an emergency. Emergency procedures for femoral hernia are associated with an almost tenfold increase in postoperative mortality, while no increase is seen for elective procedures, compared with a background population.
Objective
The aim of this study was to compare whether symptoms from femoral hernias and healthcare contacts prior to surgery differ between patients who have elective and patients who have emergency surgery.
Methods
A total of 1,967 individuals operated on for a femoral hernia over 1997–2006 were sent a questionnaire on symptoms experienced and contact with the healthcare system prior to surgery for their hernia. Answers were matched with data from the Swedish Hernia Register.
Results
A total of 1,441 (73.3 %) patients responded. Awareness of their hernia prior to surgery was denied by 53.3 % (231/433) of those who underwent an emergency procedure. Of the emergency operated patients, 31.3 % (135/432) negated symptoms in the affected groin prior to surgery and 22.2 % (96/432) had neither groin nor other symptoms. Elective patients had a considerably higher contact frequency with their general practitioner, as well as the surgical outpatient department, prior to surgery compared with patients undergoing emergency surgery (p < 0.001).
Conclusions
Patients who have elective and patients who have emergency femoral hernia surgery differ in previous symptoms and healthcare contacts. Patients who need emergency surgery are often unaware of their hernia and frequently completely asymptomatic prior to incarceration. Early diagnosis and expedient surgery is warranted, but the lack of symptoms hinders earlier detection and intervention in most cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Femoral hernias account for 2–4 % of groin hernias [1–3], but are clinically important since they are associated with a higher rate of emergency surgery and bowel resection [4–8]. Emergency procedures for femoral hernia are associated with a tenfold increase in postoperative mortality. Elective procedures do not increase mortality, even in elderly patients. [3, 9, 10] Recurrence is more common after femoral than inguinal hernia surgery. [1, 3] The risk for recurrence is higher after suture than mesh repair. [3] In Sweden, suture repairs, especially non-defined techniques, are more common in emergency procedures. [11]
The natural course of femoral hernia is poorly described. Several factors could influence the risk for incarceration and need for emergency surgery. One possible way to avoid emergency surgery is to decrease the time between onset of symptoms and contact with the healthcare system. Another approach may be to increase the awareness of femoral hernia and the risk for incarceration among general practitioners and surgeons. Early referral and expedient surgery could, at least in theory, result in avoided emergency surgery. A prerequisite for that is a time gap between the first symptoms of the hernia and its subsequent incarceration, within which the hernia can be detected, referred, and operated under optimal conditions.
Given the low incidence of femoral hernia, good-quality randomized studies are difficult to perform. Smaller studies from single centers suggest that patients with femoral hernia incarceration have a short history of hernia [12–16]. The aim of this study was to compare if symptoms from femoral hernias preceding emergency surgery differ from those in patients who have elective surgery. A secondary aim was to compare if the groups differed in healthcare contacts prior to surgery.
Materials and methods
A questionnaire on symptoms and healthcare contacts regarding the hernia prior to surgery was sent to femoral hernia patients. Patients were identified through the Swedish Hernia Register (SHR), a prospective national register of groin hernia procedures in patients older than 15 years. Register contents and its annually performed validation have been previously described [3, 17]. Between 1997 and 2006, a total of 3,451 femoral or combined hernia (with a femoral component) repairs were registered in the SHR. Patients with more than one groin hernia procedure were excluded since they might be confused regarding which repaired hernia the questionnaire referred to. The personal identity numbers [18] of the remaining patients were matched with the Swedish Population Register, to exclude patients deceased or without known address. In May 2008, the questionnaire (see full questionnaire in Online Resource 1) was sent to the remaining 1,967 patients with repair of a unilateral, primary femoral hernia. Two reminders were sent to non-responders. Figure 1 is a flow chart of the patient cohort.
Patients were asked about their awareness of the hernia prior to admittance for surgery. Presence of groin or other symptoms more than 2 weeks before surgery was addressed. Healthcare contact with either a general practitioner and/or a surgeon due to the hernia prior to admission for surgery was recorded. Patients were also asked to estimate how long, if at all, before the procedure they had been on the waiting list for surgery. Patient records were requested for 100 of the responding emergency patients for verification of their recollection of surgical consult and being on a waiting list for surgery.
Statistical analyses were performed with Stata/IC 12.1 for Windows (StataCorp LP, College Station, TX, USA). Differences in characteristics of responders (available for analysis, according to Fig. 1) and non-responders were tested using the Chi squared test and Wilcoxon rank-sum test. Pearson’s Chi squared test and logistic regression were used to compare answers from emergency and elective patients. Separate logistic regression models were used for each of the outcomes: ‘awareness of hernia’, ‘groin symptoms’, ‘any symptoms’, ‘consulted general practitioner’, ‘consulted surgeon’, and ‘on waiting list’. Apart from emergency versus elective procedure, variables included sex, age (below or above the 75th percentile), right- versus left-sided hernia, body mass index (BMI; above or below the 25th percentile), and combined versus solitary femoral hernia. Each variable was tested in a univariate analysis. Statistically significant variables and those considered of special interest, such as sex, were brought into a multivariate analysis. BMI was not recorded in the SHR protocol during the early part of the study period and data were only available for 485 (33.7 %) patients. Due to multiple testing, a Bonferroni-adjusted significance level of 0.0015 was used to account for the increased possibility of type-I error. p values and confidence intervals presented are accordingly adjusted.
Subset analyses were performed on data from the patients in the cohort who had surgery in 2002–2006 (the 5 most recent years).
The study was approved by the Regional Ethics Committee in Uppsala, Sweden. The study was performed in accordance with the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) statement. [19]
Results
Response rate and reasons for not participating are shown in Fig. 1. Median follow-up time for responders was 4.7 years (range 1.5–11.8). The median age at the time of surgery was 58 years (range 16–94), and the sex distribution was 27.6 % (397) male and 72.4 % (1,044) female. A total of 442 (30.7 %) patients had emergency repair of the hernia, whereas 999 (69.3 %) had an elective repair.
Non-responders were older, with a median age of 62 years (p < 0.001) and less often female (355/526 women, p = 0.032). Time elapsed between surgery and the beginning of the study did not differ between responders and non-responders (median 4.5 years for responders and 4.8 for non-responders, p = 0.163), nor did the frequency of emergency procedures differ (184/526, 35.0 %, in non-responders, p = 0.069).
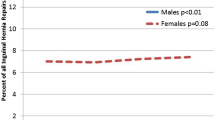
Six questions were analyzed using multivariate logistic regression models. There was a significant difference in answers from emergency patients compared with elective patients, for all of the six questions (Bonferroni-adjusted p < 0.001 in all six cases). Results from these comparisons are shown in Table 1. In the univariate analyses, neither side of the hernia nor BMI influenced the response to any of the six questions; they were therefore not included in the multivariate analyses.
‘Awareness of the hernia prior to admission for surgery’ tended to be less common for patients in the uppermost age quartile (odds ratio [OR] 0.64, 95 % confidence interval [CI] 0.41–1.00), in addition to emergency patients. Regarding ‘groin symptoms at least 2 weeks before surgery’, ‘lack of any symptoms at least 2 weeks before surgery’, ‘previous contact with the general practitioner’ and ‘on the waiting list prior to surgery’, the only difference seen was between electively and emergently treated hernias. ‘Previous contact with a surgeon’ regarding the hernia was less common among emergency patients and patients in the uppermost age quartile (OR 0.60, 95 % CI 0.38–0.93). Hernia anatomy (solitary femoral vs. combined) seemed of importance in univariate analyses, but did not influence the answer to any question in the multivariate analyses. Subset (patients operated in the latter part of the period) analysis results only differed from the entire cohort on one account; in the subset analyses, the association between awareness of the hernia and age in the uppermost quartile was not seen (OR 0.67, 95 % CI 0.39–1.14).
Among emergency patients, 53.3 % (231/433) reported that they had not been aware of the hernia prior to surgery. Table 2 accounts for how long those aware of the hernia had been so. Groin symptoms longer than 2 weeks before surgery were reported by 95.6 % (948/992) of patients with an elective repair and by 68.8 % (297/432) of patients with an emergency repair. The frequencies of specific symptoms from the groin are listed in Table 3. Among emergency-treated patients, 22.2 % (Table 1) stated that they had neither groin nor other symptoms. Elective patients reported a complete lack of symptoms in 3.9 % (39/992) of cases. Among emergency-operated patients, 10.9 % (48/440) stated that they were already on the waiting list for surgery when they had their emergency procedure. Time on waiting list was reported as less than 1 month by 12.3 % (72/584) in the elective group and by 29.2 % (14/48) in the emergency group, p = 0.035.
Of the 100 patient records sought for validation purposes, 98 were retrieved. The validation included 22.2 % of the responding patients who had emergency procedures. Nine (9.2 %) were found to have been on a waiting list prior to their emergency procedure; the agreement between questionnaire and patient records was 87.8 %. The agreement was lower regarding surgical consult prior to the emergency procedure (74.4 %). According to patient records, 20.2 % (19/94) had consulted with a surgeon regarding the hernia, whereas 35.1 % (33/94) of those patients whose records were reviewed reported contact with a surgeon in the questionnaire.
Discussion
The differences in symptoms and healthcare contacts between the patient groups were substantial. Emergency-treated femoral hernias were often not known to the patient prior to surgery. Symptoms from the groin often presented only shortly before incarceration. Almost 30 % of the emergency cases already on the waiting list for surgery had only been on it for less than 1 month.
This population-based study addresses the well known problem of emergency presentation of femoral hernias and the associated increase in postoperative mortality. It corroborates the results from previous smaller case series. Retrospective studies always carry the risk of recall bias, especially when the time elapsed after the event is long. The main findings in this study were no different when restricting analysis to the cohort from the last 5 years of the time period, indicating that the time factor had limited impact on recollection.
The frequency of femoral hernia makes it difficult to gather sufficiently large prospective cohorts in a reasonable period of time; the fact that they are often operated during on-call, increasing the risk for incomplete inclusion and missing data, make randomized studies even harder to carry out. Considering this, a study such as this one may provide the best evidence in answering the question at hand. Some elective patients reported no surgical consult or not being on the waiting list prior to surgery. This may cause concern for underestimation of symptoms and healthcare contacts in the study. The assessed patient records of more than one-fifth of the emergency patients showed that the study does not underestimate their previous healthcare contacts.
There were considerable differences in symptoms prior to surgery between patients with a femoral hernia who had emergency and those who had elective surgery. Slightly less than half of emergency patients were aware of their hernia prior to surgery. A third denied having any symptoms from the groin earlier than 2 weeks prior to surgery. Previously published studies [12–15] show that the first sign of femoral hernia is at emergency admission for a clear majority of patients with an emergency procedure. This explains the difficulty in identifying these hernias early enough to repair them electively. In this study, almost 65 % were either unaware of their hernia, or had only been aware of it for less than 1 month prior to incarceration. This is in accordance with other studies, implying a generally short hernia history before incarceration [14, 16, 20]. It also supports the view that it is difficult to hasten the diagnosis of femoral hernia in the healthcare system. A recent British study based on linked data from primary and secondary healthcare records shows that over 80 % of patients admitted as an emergency presented to their general practitioner for the first time within 7 days of admission [21].
Of the emergency-repaired patients, 10 % stated that they were diagnosed with a hernia and put on the surgical waiting list prior to admission for the emergency procedure. Their statements were corroborated by the finding that 9 % of the emergency patients whose records were assessed were on the waiting list. This was a higher figure than in earlier published series [22, 23], where none of the patients presenting with an incarcerated femoral hernia had previously been diagnosed. Each of these series comprised very few emergency femoral hernias. Rai et al. [20] and McEntee et al. [12] report 1 and 4 %, respectively, of emergency patients on the waiting list prior to surgery, but those cohorts consist of both inguinal and femoral hernia. The 10 % of emergency cases in this study who answered that they were scheduled for elective surgery stated a significantly shorter time on the waiting list than elective cases. Almost 30 % of them reported less than 1 month on the list. The natural course of femoral hernia is not completely clear. Gallegos et al. [24] relates 22 % incarceration at 1 month and 45 % at 21 months. That study, and others on patient series [12, 14, 16, 22], imply that incarcerated femoral hernia may constitute a subgroup that initially present with incarceration or imminent incarceration. This larger population-based study supports their findings. As it is difficult to know which subgroup a specific hernia belongs to, the recommendation that elective surgery for femoral hernia should be given high priority is justified [3, 25].
This study did not show any of the patient characteristics to be associated with a higher risk for incarceration without prior symptoms. Patients over 70 years had groin and other symptoms to the same extent as younger patients. They were not as often aware that they had a hernia and had less often consulted a surgeon. The sex of the patient affected neither symptoms of a hernia nor the seeking of medical advice. The use of the rather conservative Bonferroni correction introduces a risk that weaker risk factors remain undetected. A Swedish study [26] has shown that femoral hernia presenting with incarceration is over-represented among patients with a low BMI.
About half of the emergency patients who stated that they were unaware of the hernia reported that they had experienced some symptom from the affected groin more than 2 weeks prior to surgery. If this is the case, increasing the awareness of femoral hernia within the population may help bring patients to earlier diagnosis. Could a screening program reduce mortality by bringing patients to earlier diagnosis? Considerable demands would be placed on such a program, since many femoral hernias incarcerate shortly after presentation. The chosen population would need to be examined regularly at short intervals and it seems unlikely that a cost-benefit analysis would support such a program.
Improving management of patients with symptoms of hernia incarceration or intestinal obstruction at the emergency department may be a more feasible approach. Several studies imply that the time from incarceration to diagnosis and from decision to operate to induction of anesthesia [15, 27, 28] is unnecessarily and sometimes fatally long.
Conclusion
Patients who have emergency and elective procedures for femoral hernia differ greatly. Patients who present with incarceration are often previously unknown to the healthcare system. Furthermore, a majority are themselves unaware of the hernia when the incarceration occurs. Many have not had any symptoms that might have led them to suspect a hernia. Thus, the most effective way of addressing the excess mortality associated with emergency femoral hernia repair seems to be continuing efforts to improve management of patients attending the emergency department for incarcerated or imminent incarceration of a femoral hernia.
References
Glassow F (1985) Femoral hernia: review of 2,105 repairs in a 17 year period. Am J Surg 150:353–356
Bay-Nielsen M, Kehlet H, Strand L et al (2001) Quality assessment of 26,304 herniorrhaphies in Denmark: a prospective nationwide study. Lancet 358:1124–1128
Dahlstrand U, Wollert S, Nordin P et al (2009) Emergency femoral hernia repair: a study based on a national register. Ann Surg 249:672–676
Kulah B, Kulacoglu IH, Oruc MT et al (2001) Presentation and outcome of incarcerated external hernias in adults. Am J Surg 181:101–104
Kurt N, Oncel M, Ozkan Z et al (2003) Risk and outcome of bowel resection in patients with incarcerated groin hernias: retrospective study. World J Surg 27:741–743. doi:10.1007/s00268-003-6826-x
Alvarez JA, Baldonedo RF, Bear IG et al (2004) Incarcerated groin hernias in adults: presentation and outcome. Hernia 8:121–126
Ge BJ, Huang Q, Liu LM et al (2010) Risk factors for bowel resection and outcome in patients with incarcerated groin hernias. Hernia 14:259–264
van den Heuvel B, Dwars BJ, Klassen DR et al (2011) Is surgical repair of an asymptomatic groin hernia appropriate? A review. Hernia 15:251–259
Gunnarsson U, Degerman M, Davidsson A et al (1999) Is elective hernia repair worthwhile in old patients? Eur J Surg 165:326–332
Nilsson H, Stylianidis G, Haapamaki M et al (2007) Mortality after groin hernia surgery. Ann Surg 245:656–660
Dahlstrand U, Sandblom G, Nordin P et al (2011) Chronic pain after femoral hernia repair: a cross-sectional study. Ann Surg 254:1017–1021
McEntee GP, O’Carroll A, Mooney B et al (1989) Timing of strangulation in adult hernias. Br J Surg 76:725–726
Roth N, Gangl O, Havlicek W et al (2010) The impact of emergency surgery on results of femoral hernia repair. Eur Surg 42:299–303
Alani A, Page B, O’Dwyer PJ (2006) Prospective study on the presentation and outcome of patients with an acute hernia. Hernia 10:62–65
Tiernan JP, Katsarelis H, Garner JP et al (2010) Excellent outcomes after emergency groin hernia repair. Hernia 14:485–488
Malek S, Torella F, Edwards PR (2004) Emergency repair of groin herniae: outcome and implications for elective surgery waiting times. Int J Clin Pract 58:207–209
Nilsson E, Haapaniemi S, Gruber G et al (1998) Methods of repair and risk for reoperation in Swedish hernia surgery from 1992 to 1996. Br J Surg 85:1686–1691
Ludvigsson JF, Otterblad-Olausson P, Pettersson BU et al (2009) The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol 24:659–667
von Elm E, Altman DG, Egger M et al (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370:1453–1457
Rai S, Chandra SS, Smile SR (1998) A study of the risk of strangulation and obstruction in groin hernias. Aust N Z J Surg 68:650–654
Humes DJ, Radcliffe RS, Camm C et al (2013) Population-based study of presentation and adverse outcomes after femoral hernia surgery. Br J Surg 100:1827–1832
Suppiah A, Gatt M, Barandiaran J et al (2007) Outcomes of emergency and elective femoral hernia surgery in four district general hospitals: a 4-year study. Hernia 11:509–512
Abi-Haidar Y, Sanchez V, Itani K (2011) Risk factors and outcomes of acute versus elective groin hernia surgery. J Am Coll Surg 213:363–369
Gallegos NC, Dawson J, Jarvis M et al (1991) Risk of strangulation in groin hernias. Br J Surg 78:1171–1173
Simons MP, Aufenacker T, Bay-Nielsen M et al (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403
Rosemar A, Angerås U, Rosengren A et al (2010) Effect of body mass index on groin hernia surgery. Ann Surg 252:397–401
Nilsson H, Nilsson E, Angeras U et al (2011) Mortality after groin hernia surgery: delay of treatment and cause of death. Hernia 15(3):301–307
Kjaergaard J, Bay-Nielsen M, Kehlet H (2010) Mortality following emergency groin hernia surgery in Denmark. Hernia 14:351–355
Acknowledgments
The work was funded by grants from Uppsala-Örebro Regional Research Council and Stockholm County Council.
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dahlstrand, U., Sandblom, G., Wollert, S. et al. Limited Potential for Prevention of Emergency Surgery for Femoral Hernia. World J Surg 38, 1931–1936 (2014). https://doi.org/10.1007/s00268-014-2539-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2539-6