Abstract
Background
No studies have compared robot-assisted transaxillary thyroidectomy (RATT) and minimally invasive video-assisted thyroidectomy (MIVAT) regarding cosmetic outcome and satisfaction
Methods
Patients matching the inclusion criteria (benign nodule less than 4 cm and thyroid volume less than 30 mL) were randomly allotted to undergo MIVAT (group A) or RATT (group B). Cosmetic result, overall satisfaction, operative time, and complications were evaluated.
Results
A total of 62 patients underwent hemithyroidectomy (30 in group A and 32 in group B). All patients were women, with the exception of one man in each group. The mean patient age was 36.9 years (group A) and 32.5 years (group B). Total operative time (intubation–extubation) was shorter in group A (71.6 min) than in group B (120.4 min). Complications included one transient laryngeal nerve injury in each group and one subcutaneous hematoma in group B. Postoperative hospital stay was longer in group B (1.85 days) than in group A (1.15 days). On the PASQ questionnaire, “scar appearance” and “satisfaction with appearance” scores were better in group A than in group B. In the Short Form (SF-36) 36-Item Health Survey Questionnaire, domains of “social activity” and “general health” were better in group B than in group A, whereas “bodily pain” scored higher in group B than in group A.
Conclusions
RATT seems not to supersede MIVAT in terms of satisfaction when comparing two groups of patients undergoing thyroidectomy for benign disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the first report of endoscopic parathyroidectomy in 1996 [1], countless endoscopic and minimally invasive procedures have been developed with the aim of obtaining the safest approach with the best cosmetic result and postoperative outcome after thyroidectomy.
Aiming to shift the scar from the neck, several endoscopic approaches, including transaxillary endoscopic thyroidectomy [2, 3], the breast approach [4], the anterior chest wall approach using a flap-lifting system [5], the axillobilateral-breast approach [6], the bilateral axillo-breast approach [7], and transareola single-site endoscopic thyroidectomy [8] have been proposed, most often by surgeons in Far Eastern countries. Several trials have shown that most of these techniques achieved the goal of shifting the operative scar better than traditional cervicotomy [9–12] for both benign and malignant disease. However, these endoscopic approaches have also proved to be technically challenging because of two-dimensional vision and inadequate instrumentation; above all, they cannot be considered minimally invasive [3, 13, 14].
As a consequence, minimally invasive video-assisted thyroidectomy (MIVAT), proposed in 1998 [15], with its central cervical access, gained larger popularity in Europe and became the most widespread minimally invasive endoscopic technique for thyroidectomy in North America [16]. Several studies reported MIVAT as safe, easily reproducible, and achieving optimal results compared with traditional cervicotomy in cosmetic outcome, postoperative pain, and postoperative course, not only for benign disease but also for low-risk and intermediate-risk papillary carcinoma [17–25].
In recent years, the da Vinci S surgical robotic system was developed to improve the weak points of endoscopic surgery, and recent studies have reported that robot-assisted transaxillary thyroidectomy (RATT), introduced by Chung in South Korea in 2009 [26, 27], is feasible, safe, and has excellent cosmetic results. The robotic approach easily surpasses the endoscopic techniques performed with conventional laparoscopic instrumentation through the same access because it permits magnified and enhanced three-dimensional vision, provides a fourth arm that can be used to retract the thyroid lobe, and allows extended freedom of motion of the robotic instruments as well as comfortable surgeon ergonomics. The first aim of this technique is an optimal cosmetic result, and indeed, RATT represents a “scarless in the neck” operation. In fact, several studies that have compared RATT with axillary endoscopic thyroidectomies have reported that the robotic approach provides better cosmetic results and superior patient satisfaction [28–32]. More recently, an alternative “scarless in the neck” approach that takes advantage of the robotic system is the “robotic facelift thyroidectomy” proposed by Terris and Singer in 2012 and performed through a postauricular and occipital hairline (facelift) incision [33].
The enthusiasm generated by the introduction of these new robot-assisted techniques is seriously limited by their cost, which is much higher than those of the traditional approach and video-assisted thyroidectomy. Broome et al report a 217 % increased cost of robotic thyroidectomy compared with traditional thyroidectomy, and this greater expense could well be prohibitive in countries with a flat reimbursement schedule [34–36].
In the context of this wide and varied panorama of different approaches designed to reach the best cosmetic result, to the best of our knowledge, there are no published studies comparing RATT and MIVAT. We therefore initiated the present study to prospectively compare two groups of thyroid surgery patients randomly allotted to MIVAT or RATT.
Patients and methods
Study design
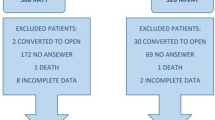
This prospective, double-arm study recruited 62 patients undergoing hemithyroidectomy between January 2012 and September 2013 at the Department of Surgery, University of Pisa. Eligibility criteria were benign disease, maximum nodule diameter up to 4 cm, and total thyroid volume of less than 30 mL. Excluded were patients with symptoms attributable to the thyroid nodule (dysphagia, dyspnea, dysphonia), so as not to affect the validity of the SF-36 questionnaire findings. In addition, patients with malignant disease, intrathoracic goiter, previous neck operation or neck irradiation, and those who required central or lateral compartment lymphadenectomy, permanent medication for pain, and anticoagulation medication were excluded. All patients provided an informed consent for the study.
Among 376 patients referred to our department during the study period with uninodular benign thyroid benign disease who were scheduled for surgery, 62 matched the inclusion criteria and were randomly allotted to undergo hemithyroidectomy by the MIVAT technique (group A) or hemithyroidectomy by the RATT procedure (group B). These patients, who were previously informed of the randomization to one of these two techniques, were assigned the day before surgery by draw, with a sealed envelope containing “MIVAT” or “RATT.”
Study end points were mainly two specific outcomes of the procedures: cosmetic result and overall patient satisfaction. Also, operative time and length of hospital stay were considered, both involving important differences in costs of the two different procedures.
Complications were also assessed, even though a statistical comparison was not possible because of the very limited incidence of complications in patients undergoing thyroid surgery.
Surgical treatment
MIVAT
MIVAT was performed with the patient supine, without neck extension, through a central, transverse 1.5 cm incision placed two fingers above the sternal notch. Operative space was maintained by external use of small retractors. A 30° 5 mm endoscope was used during the endoscopic step. Under endoscopic vision, the upper pedicle was dissected and divided with a Harmonic Scalpel. The recurrent nerve and parathyroid glands were identified and isolated. After extraction of the lobe, hemithyroidectomy was achieved. Hemostasis was obtained by Harmonic Scalpel and titanium clips (5 mm). Subcuticular stitches and glue were used to close the wound. Drains were never used.
RATT
The da Vinci S system (Intuitive Surgical Inc.) was used in all procedures. The patient was placed supine with one arm extended over the shoulder. The working space was created using the standard technique through a 5–7 cm skin incision along the anterior border of the pectoralis major muscle. A Chung’s retractor was used to maintain the operative space. Only three robotic arms were used in all operations. During the docking of the robot, the dual-channel endoscope was positioned on the central robotic arm, the Harmonic curved shears were positioned on the upper side arm, and the Maryland dissector (Intuitive Surgical) was positioned on the lower side arm.
The operation started with dissection of the upper pedicle. Under endoscopic view, the upper pole was dragged downward with the Maryland dissector. The upper thyroid vessels were exposed then sealed and interrupted with the Harmonic shears, very close to the thyroid capsule to avoid any damage to the external branch of the upper laryngeal nerve. The Maryland dissector was then used to retract the thyroid lobe medially, and the surgeon started the identification of the recurrent laryngeal nerve, dissecting the tracheoesophageal groove with the Harmonic shears, both bluntly and by cutting. In the same manner, the parathyroid glands were identified and preserved. Once the critical structures were identified, the thyroid lobe was dissected with the Harmonic scalpel and the specimen was removed. A drain was left in the operative space, and the skin was closed with intradermal reabsorbable suture.
Assessment of surgical complications
Direct fiberoptic laryngoscopy was performed in all patients immediately before and 3 months after thyroidectomy to assess vocal cord motility. Recurrent laryngeal nerve injury was considered permanent if persistent 6 months after surgery. Hypoparathyroidism assessment was not considered necessary because all procedures were simple hemithyroidectomies.
Analysis of epidemiological data, follow-up, and cosmetic and satisfaction outcome assessment
Data were collected on age, sex, body mass index (BMI), thyroid volume, nodule diameter, skin-to-skin operative time, total time from intubation to extubation, final histology report, complications, and length of postoperative hospital stay. The cosmetic result was evaluated after 2 months by the by the Patient Scar Assessment Questionnaire (PSAQ). Overall satisfaction was evaluated after 1 month by the SF-36 questionnaire. The completed questionnaires were retrieved by means of a telephone interview by a researcher directly involved in the study but not in the surgery (A.B.).
PSAQ
The PSAQ was used with the aim of providing a valid measure of each patient’s perception of scarring. This scale, designed specifically for the assessment of linear scars, is composed of four subscales: scar appearance, consciousness, satisfaction with scar appearance, and satisfaction with scar symptoms. The symptoms subscale was omitted because of its poor reliability in this kind of scar. For each subscale, a higher score reflects a poorer outcome. The reliability of this scale has been demonstrated in several studies, in particular, to evaluate scars after thyroid and parathyroid surgery [36, 37].
SF-36 2 health survey (version 2.0)
SF-36 2 questionnaire was used to evaluate the burden of surgery. The SF-36 is a multipurpose, short-form health survey that has proven to be useful in the assessment of a patient’s quality of life (QoL). It is composed of eight subscales, each highlighting a different aspect of a patient’s QoL: physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional, and mental health. For this tool, a lower score indicates a poorer QoL [38].
Statistical analysis
We used the Kolmogorov–Smirnov test to check normality of data distribution. The introductory phase was concluded with a statistical power analysis (ex post) to estimate the sample size required for the specific tests. The 1 − β value of the significant variables was >0.8, assuring a low risk of type II error and an appropriate sample size. We used the Mann-Whitney test and the t test to assess continuous variables and the χ 2 test for categorical variables. The analysis was performed with SPSS 17.0.1 software (SPSS Inc, Chicago, IL).
Results
A total of 62 patients matched the inclusion criteria previously mentioned and underwent hemithyroidectomy. Of those 62 patients, 30 were allotted to group A (MIVAT) and 32 to group B (RATT).
The remaining 314 patients with uninodular benign disease scheduled for surgery in the same period were excluded from the study and underwent hemythyroidectomy by a traditional approach (standard cervicotomy) for the following reasons: the diameter of the thyroid nodule was larger than 4 cm in 279 cases, compressive symptoms attributable to the thyroid nodule were present in 21 cases, patients refused to enter the study in 14 cases.
The groups were well matched for age, sex ratio, nodule diameter, and BMI (Table 1). There were 29 women and 1 man in group A and 31 women and 1 man in group B. Patients were a mean age of 36.9 ± 9.6 years (range 21–62 years) in group A and 32.5 ± 11.25 years (range 18–73 years) group B. There were 16 right lobectomies and 14 left lobectomies in group A, and 15 right lobectomies and 17 left lobectomies in group B. No conversions to open cervicotomy were required.
The preoperative diagnosis was 21 nodular goiters and 9 microfollicular nodules in group A and 19 nodular goiters, 3 toxic adenomas, and 10 microfollicular nodules in group B. The final histology report showed benign disease in all patients except two microfoci of papillary carcinoma (0.3 and 0.5 mm) in two patients in group A and three microfoci of papillary carcinoma (0.1, 0.2, and 0.6 mm) in group B (Table 1).
Operative time (open to close time in the MIVAT group and open to close time [without docking time] in the RATT group) was significantly shorter in the MIVAT group (group A), at 46.5 ± 10.5 min (range 30–70 min) than in the RATT group (group B), at and 85.25 ± 48.76 min (range 19–220 min). Total surgical time (intubation–extubation time, including draping of the operative space and docking time in group B) was significantly shorter in group A (71.6 ± 13.3; range 50–95 min) than in group B (121.5 ± 46.8; range 74–325 min; p < 0.0001) (Table 1).
Complications consisted of one transient recurrent laryngeal nerve injury in each group and one subcutaneous hematoma over the major pectoralis fascia in group B. Hematoma was diagnosed by ultrasound on the first postoperative day and conservatively treated, both with ultrasound-guided evacuation of the blood and with antibiotics administration. There were no long-term complications, as the recurrent nerve injury in both patients healed completely in two months.
Postoperative stay was 1.85 days in group B, which was significantly longer than the 1.15 days in group A (p < 0.0001). This extension of the hospital stay was due to the necessity of keeping the drain (which is not used in group A patients) for longer than one day in most of the group B patients.
Assessment of cosmetic result and overall satisfaction
On the PASQ, the appearance and satisfaction with appearance scores were both significantly higher in group B than in group A, at 16.93 ± 3.78 versus 13.62 ± 2.94 (p < 0.0001) and 15.71 ± 4.60 versus 12.03 ± 3.65 (p < 0.018), and the remaining variables (consciousness and satisfaction with symptoms) were comparable. These results mean that patients who underwent MIVAT (group A) were more satisfied with their scar than those who underwent RATT (group B).
Scores for the SF-36 domains of social activity and general health were significantly higher in group B than in group A [90.01 ± 23.41 vs 74.03 ± 27.34 (p < 0.006) and 90.70 ± 12.10 vs 78.51 ± 17.71 (p < 0.0001)], showing that patients undergoing RATT have a better perception of their general state of health and are more likely to participate in social activities than patients undergoing MIVAT. Scores for bodily pain were significantly higher in group A than in group B (96.82 ± 7.99 vs 81.67 ± 21.43; p < 0.0005), indicating that patients undergoing MIVAT experienced less tenderness than patients undergoing RATT. Scores for the remaining domains (physical functioning, role-physical, vitality, role-emotional, and mental health) were comparable in the two groups. Results are summarized in Table 2.
Discussion
To our knowledge, this is the first prospective randomized study comparing cosmetic and overall satisfaction after MIVAT and RATT for the treatment of benign disease. Concerning this primary end point of the study, RATT seems not to supersede MIVAT when comparing two groups of patients undergoing thyroidectomy for benign disease, although nodule diameter was significantly larger in the RATT group.
In particular, the PSAQ questionnaire, which specifically evaluates the scar, highlighted that the axillary scar, even if hidden in a remote site, is less appreciated than the scar produced by MIVAT, although the latter is more evident. The appearance and satisfaction with scar appearance scores (Table 2) significantly favored MIVAT. This might be due mainly to the length of the scar after RATT, which is necessarily longer, and less obviously because the axillary skin incision, which is placed in the border of the pectoralis major muscle and does not follow the natural skin folds, might result in poorer healing. Although not all agree about the superiority of small incisions in the neck [37], it is worthwhile noting that other studies [39] reaffirm that the cosmetic result after MIVAT, evaluated with a mean follow-up of almost 2 years with two scales: observer scar assessment score and patient scar assessment score, was classified as excellent, with 1.3 points on a 4-point scale.
For the SF-36 questionnaire, we found that patients undergoing RATT had a better perception of their general state of health and were more likely to participate in social activities after surgery, but they also scored higher on the bodily pain domain at prolonged follow-up.
Since its introduction, the RATT procedure has yielded in published studies better patient outcomes than open thyroidectomy, including lower postoperative pain and increased cosmetic satisfaction [31, 32]. If the increased cosmetic satisfaction provided by RATT and reported by these published series seems reasonable when comparing RATT with traditional cervicotomy because of the hidden location of the skin incision, the lower postoperative pain after RATT is difficult to understand. The difficulty comes from comparing patients undergoing a “maximally invasive” operation (dissection of a large flap over the major pectoralis fascia from the axilla to the neck) and patients undergoing cervicotomy, where, most of the time, in expert hands, an incision not larger than 6–8 cm can allow a perfect thyroidectomy but where also a subcutaneous flap is necessary as is hyperextension of the neck, which might be responsible for a large part of the postoperative distress after conventional surgery. These two technical features are overcome in MIVAT, which is performed through a 1.5 cm incision with the patient in the supine position and does not require dissection of a subcutaneous flap. For this reason in several articles [21–24, 38–40] MIVAT proved to allow a superior cosmetic result and a better cosmetic outcome in patients with small thyroid nodules. The drawback of this operation though is that, like conventional thyroidectomy, it is performed on a very visible part of the body.
For these reasons, it seemed reasonable to try a comparison between two endoscopic procedures, both of them considered cosmetic, rather than comparing either of them with traditional thyroidectomy.
In spite of the significant limits imposed by the sharp cost increase associated with RATT, it has an advantage over MIVAT in that it allows treatment of larger lesions (up to 6 cm in size) and therefore allows recruiting larger numbers of patients. In fact, one of the major limits of MIVAT is the strict limitation imposed by the maximum thyroid volume (30 mL) and nodule diameter (3 cm), which narrows the patients who can benefit from the MIVAT procedure to 10–15 % of patients being considered for thyroid surgery [17]. Conversely, because the dimensional limit for RATT is 5–6 cm, a larger number of patients will benefit from a cosmetic operation while complaining of larger goiters [26]. This point must not be overlooked as a consistent advantage of the robotic technique compared with MIVAT, especially in Europe, where goiter is endemic and mean thyroid volumes are higher than in the Far East.
In the present series there were no differences with regard to complications, but a statistical comparison was not possible because of the small incidence of complications after thyroid surgery no matter which procedure is employed. Both MIVAT and RATT benefit from the magnification provided by the endoscope (and a 3D image for the robotic approach). Several reports have shown a complication rate similar to traditional thyroidectomy for endoscopic operations [41–44]. Hypoparathyroidism was not evaluated in the present series because all patients underwent hemithyroidectomy, which almost always excludes the risk that this important complication will occur.
When analyzing the length of the surgical procedure, we found (Table 1) that the two groups differed significantly. Total time was significantly longer in the RATT group (121.5 ± 46.8 min; range 74–325 min) than in the MIVAT group (71.6 ± 13.3 min; range 50–95 min; p < 0.0001). That must be considered an important disadvantage of RATT; if we consider both the longer operative time and the longer length of hospital stay it must be said that this cosmetic procedure implies a significant increase in costs that is not paralleled by an increased satisfaction of the patients. In fact, in our series, the bodily pain score on the SF-36 questionnaire was higher in group B than in group A (Table 1). The problem of a correct allocation of resources, of course, exceeds the aims of the present study. Furthermore, a cost analysis would not have been performed because of the difficulty in comparing costs in different countries and under different health systems, but other researchers have already stressed that the simple traslocation of a scar from the neck to the axilla probably does not justify the added expense [45].
In conclusion, the results that we found most surprising were those reflecting patient satisfaction with scar appearance as assessed by the PSAQ “appearance” and “satisfaction with scar appearance” subscales (Table 2): this demonstrates that relocating the wound from the neck to a less visible area, such as the axilla, is not enough to meet the full expectations of the patients, probably because the axilla scar is still considered to be too long and its appearance is less likely to improve over time because it cannot be placed in a skin crease. Our results appear to be in agreement with the words of Duh, “For now… neck incisions… are here to stay” [46].
References
Gagner M (1996) Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg 83:875
Ikeda Y, Takami H, Niimi M et al (2002) Endoscopic thyroidectomy and parathyroidectomy by the axillary approach. A preliminary report. Surg Endosc 16:92–95
Yoon JH, Park CH, Chung WY (2006) Gasless endoscopic thyroidectomy via an axillary approach: experience of 30 cases. Surg Laparosc Endosc Percutan Tech 16:226–231
Ohgami M, Ishii S, Arisawa Y et al (2000) Scarless endoscopic thyroidectomy: breast approach for better cosmesis. Surg Laparosc Endosc Percutan Tech 10:1–4
Cho YU, Park IJ, Choi KH et al (2007) Gasless endoscopic thyroidectomy via an anterior chest wall approach using a flap-lifting system. Yonsei Med J 48:480–487
Bärlehner E, Benhidjeb T (2007) Cervical scarless endoscopic thyroidectomy: axillo-bilateral-breast approach (ABBA). Surg Endosc 22:154–157
Choe JH, Kim SW, Chung KW et al (2007) Endoscopic thyroidectomy using a new bilateral axillo-breast approach. World J Surg 31:601–606. doi:10.1007/s00268-006-0481-y
Shan YZ, Zhou LM, Yu ZF et al (2012) Comparison between transareola single site endoscopic thyroidectomy and minimally invasive video-assisted thyroidectomy. J Int Med Res 40:2213–2219
Ikeda Y, Takami H, Sasaki Y et al (2003) Clinical benefits in endoscopic thyroidectomy by the axillary approach. J Am Coll Surg 196:189–195
Ikeda Y, Takami H, Sasaki Y et al (2002) Comparative study of thyroidectomies. Endoscopic surgery versus conventional open surgery. Surg Endosc 16:1741–1745
Ikeda Y, Takami H, Sasaki Y et al (2004) Are there significant benefits of minimally invasive endoscopic thyroidectomy? World J Surg 28:1075–1078. doi:10.1007/s00268-004-7655-2
Chung YS, Choe JH, Kang KH et al (2007) Endoscopic thyroidectomy for thyroid malignancies: comparison with conventional open thyroidectomy. World J Surg 31:2302–2308. doi:10.1007/s00268-007-9117-0
Kang SW, Jeong JJ, Yun JS et al (2009) Gasless endoscopic thyroidectomy using transaxillary approach: surgical outcome of 581 patients. Endocr J 56:361–369
Ikeda Y, Takami H, Sasaki Y et al (2000) Endoscopic neck surgery by axillary approach. J Am Coll Surg 191:336–340
Miccoli P, Berti P, Conte M et al (1999) Minimally invasive surgery for small thyroid nodules: preliminary report. J Endocrinol Invest 22:849–851
Terris DJ, Angelos P, Steward DL et al (2008) Minimally invasive video assisted thyroidectomy: a multiinstitutional North American experience. Arch Otolaryngol Head Neck Surg 134:81–84
Minuto MN, Berti P, Miccoli M et al (2012) Minimally invasive video-assisted thyroidectomy: an analysis of results and a revision of indications. Surg Endosc 26:818–822
Radford PD, Ferguson MS, Magill JC et al (2011) Meta-analysis of minimally invasive video-assisted thyroidectomy. Laryngoscope 121:1675–1681
Byrd JK, Nguyen SA, Ketcham A et al (2010) Minimally invasive video-assisted thyroidectomy versus conventional thyroidectomy: a cost-effective analysis. Otolaryngol Head Neck Surg 143:789–794
Miccoli P, Rago R, Massi M et al (2010) Standard versus video-assisted thyroidectomy: objective postoperative pain evaluation. Surg Endosc 24:2415–2417
Miccoli P, Materazzi G, Berti P (2010) Minimally invasive thyroidectomy in the treatment of well differentiated thyroid cancers: indications and limits. Curr Opin Otolaryngol Head Neck Surg 18:114–118
Miccoli P, Pinchera A, Materazzi G et al (2009) Surgical treatment of low-and intermediate-risk papillary thyroid cancer with minimally invasive video-assisted thyroidectomy. J Clin Endocrinol Metab 94:1618–1622
Miccoli P, Minuto MN, Ugolini C et al (2008) Minimally invasive video-assisted thyroidectomy for benign thyroid disease: an evidence-based review. World J Surg 32:1333–1340. doi:10.1007/s00268-008-9479-y
Miccoli P, Materazzi G (2004) Minimally invasive, video-assisted thyroidectomy (MIVAT). Surg Clin North Am 84:735–741
Miccoli P, Berti P, Raffaelli M et al (2001) Comparison between minimally invasive video-assisted thyroidectomy and conventional thyroidectomy: a prospective randomized study. Surgery 130:1039–1043
Kang SW, Lee SC, Lee SH et al (2009) Robotic thyroid surgery using a gasless, transaxillary approach and the da Vinci S system: the operative outcomes of 338 consecutive patients. Surgery 146:1048–1055
Kang SW, Jeong JJ, Nam KH et al (2009) Robot-assisted endoscopic thyroidectomy for thyroid malignancies using a gasless transaxillary approach. J Am Coll Surg 209:1–7
Lee J, Chung WY (2013) Robotic thyroidectomy and neck dissection: past present and future. Cancer J 19:151–161
Jackson NR, Yao L, Tufano RP et al (2014) Safety of robotic thyroidectomy approaches: meta-analysis and systematic review. Head Neck 36:137–143
Yi O, Yoon JH, Lee YM et al (2013) Technical and oncologic safety of robotic thyroid surgery. Ann Surg Oncol 20:1927–1933
Aliyev S, Taskin HE, Agcaoglu O et al (2013) Robotic transaxillary total thyroidectomy through a single axillary incision. Surgery 153:705–710
Chung WY (2012) Pros of robotic transaxillary thyroid surgery: its impact on cancer control and surgical quality. Thyroid 22:986–987
Terris DJ, Singer MC (2012) Robotic facelift thyroidectomy: facilitating remote access surgery. Head Neck 34:746–747
Broome JT, Pomeroy S, Solorzano CC (2012) Expense of robotic thyroidectomy: a cost analysis at a single institution. Arch Surg 147:1102–1106
Inabnet WB 3rd (2012) Robotic thyroidectomy: must we drive a luxury sedan to arrive at our destination safely? Thyroid 22:988–990
Cabot JC, Lee CR, Brunaud L et al (2012) Robotic and endoscopic transaxillary thyroidectomies may be cost prohibitive when compared to standard cervical thyroidectomy: a cost analysis. Surgery 152:1016–1024
Economopoulos KP, Petralias A, Linos E et al (2012) Psychometric evaluation of Patient Scar Assessment Questionnaire following thyroid and parathyroid surgery. Thyroid 22:145–150
Linos D, Economopoulos KP, Kiriakopoulos A et al (2013) Scar perceptions after thyroid and parathyroid surgery: comparison of minimal and conventional approaches. Surgery 153:400–407
Sahm M, Schwarz B, Schmidt S et al (2011) Long-term cosmetic result after minimally invasive video-assisted thyroidectomy. Surg Endosc 25:3202–3208
Bellantone R, Lombardi CP, Bossola M et al (2002) Video-assisted vs conventional thyroid lobectomy: a randomized trial. Arch Surg 137:301–304
Garratt A, Schmidt L, Mackintosh A et al (2002) Quality of life measurement: bibliographic study of patient assessed health outcome measures (Review). BMJ 324(7351):1417
Lee J, Nah KY, Kim RM et al (2010) Differences in postoperative outcomes, function, and cosmesis: open versus robotic thyroidectomy. Surg Endosc 24:3186–3194
Tae K, Kim KY, Yun BR et al (2012) Functional voice and swallowing outcomes after robotic thyroidectomy by a gasless unilateral axillo-breast approach: comparison with open thyroidectomy. Surg Endosc 26:1871–1877
Tae K, Ji YB, Jeong JH et al (2011) Robotic thyroidectomy by a gasless unilateral axillo-breast or axillary approach: our early experiences. Surg Endosc 25:221–228
Perier N (2012) Why I have abandoned robot assisted transaxillary thyroid surgery. Surgery 152:1025–1026
Duh QY (2011) Robot assisted endoscopic thyroidectomy: has the time come to abandon neck incisions? Ann Surg 253:1067–1068
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Materazzi, G., Fregoli, L., Manzini, G. et al. Cosmetic Result and Overall Satisfaction after Minimally Invasive Video-assisted Thyroidectomy (MIVAT) versus Robot-assisted Transaxillary Thyroidectomy (RATT): A Prospective Randomized Study. World J Surg 38, 1282–1288 (2014). https://doi.org/10.1007/s00268-014-2483-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2483-5