Abstract
Background
Microvascular infiltration (MVI) is considered a necessary step in the metastatic evolution of hepatocellular carcinoma (HCC), but its prognostic value after liver resection (LR) is uncertain. We studied the clinical value of MVI compared to the Milan criteria in a consecutive series of patients submitted to radical LR.
Methods
A total of 441 patients were retrospectively evaluated. MVI and the Milan criteria were analyzed and compared as prognostic factors for overall and disease-free survival (DFS).
Results
MVI was present in 189 patients (42.8 %). Grading, satellitosis, size of cancer, and alfa fetoprotein value were significantly related to MVI, which was present in 34.3 and 53.2 % of Milan+ and Milan− patients, respectively (p = 0.00001). Both MVI and the Milan criteria were associated with a lower overall and DFS, but only the Milan criteria were associated with the rate of early recurrence and the feasibility of a curative treatment of the recurrence. The application of MVI parameters to patients classified by the Milan criteria further selects the outcome in Milan+ patients (5-year survival rate of 54.1 and 67.9 %, respectively, in the presence or absence of MVI) but not in Milan− patients.
Conclusions
MVI is related to survival after LR for HCC, but the clinical value of this information is limited. In Milan+ patients, the absence of MVI selects the cases with better prognosis. In the presence of a liver recurrence, the Milan criteria related to the primary HCC show a better prognostic accuracy and have clinical relevance in the decision-making process.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Liver resection (LR) and orthotopic liver transplantation (OLT) are the best radical treatments of hepatocellular carcinoma (HCC) [1]. The Milan criteria, proposed by Mazzaferro et al. [2] more than 15 years ago for the selection of patients for OLT, provide the simplest definition of “early” cancer and are now considered useful for patients thought to be candidates for LR too [1, 3, 4]. For HCC within the Milan criteria (Milan+; single HCC <5 cm or <3 nodules, each <3 cm in size), LR is well accepted in presence of normal liver function; long-term overall survival (OS) is similar to OLT, but a higher rate of recurrence is expected [5]. A growing experience was recently presented favoring LR for patients outside these criteria (Milan−), exploiting, in selected series, better results than could be achieved with other nonsurgical therapies. Accordingly, the search for prognostic factors must be directed both to Milan+ and Milan− patients, with the aim to select, beyond the Milan criteria, the subgroup of patients who can benefit from a curative therapy.
Among the patients who undergo operation, microvascular infiltration (MVI) is considered crucial for survival [6–10]; the invasion of the peripheral portal vein is regarded as the anatomic prerequisite and the main way to spread cancer cells both in the hepatic circulation and the systemic circulation [9]. The value of MVI is particularly stressed after OLT, because the long-term result in these patients is not satisfactory [8, 11]; as a consequence, preoperative factors that are statistically related to MVI have clinical relevance. In contrast, for patients referred for LR, the significance of MVI is not widely accepted. In particular, there isn’t a well-defined correlation between overall and disease-free survival (DFS), nor to specific types of recurrence, which can be cured at significantly different rates. A predictive value of MVI regarding these considerations could be important in establishing the different phases of therapy; first, for the choice between surgery and the percutaneous ablation therapies, such as percutaneous ethanol injection (PEI) and radiofrequency ablation (RFA), which should be favored when a high recurrence rate would be expected. Furthermore, MVI could lead to a personalized postoperative follow-up, or prompt selection of adjuvant treatments after surgery or even to a preemptive OLT [12]. Finally, in case of recurrence, MVI in the primary tumor could be a useful guide for the choice of the right therapy for recurrence.
In the present article, we review our experience with LR for HCC over a 20 year period. This retrospective study was designed to assess the clinical value of both the Milan criteria and MVI, analyzed as a single predictive factor or in combination, in the complex choice of therapy for primary and recurrent HCC.
Materials and methods
Four hundred eighty-one patients who underwent LR for HCC at the Surgical Clinic of the University of Brescia-Italy in the period 1990–2009, are the subjects of the study. Patients were considered suitable for surgery if all the nodules were resectable with an adequate residual volume and if the Child-Pugh classification was A; age was not a limiting factor. All the resections were considered radical when a free margin was obtained and the first US 3 months after surgery was negative. Type of hepatectomy was assessed according to Couinaud segmentation and defined as in the Brisbane classification [13]. Surgical resection was considered major if three or more liver segments were removed.
MVI was defined as the presence of clusters of cancer cells floating in the vascular space lined by endothelial cells [14]. The evaluation was performed just at the periphery of the nodule [14]; in the doubtful cases, immunohistochemical analysis with CD34 (monoclonal antibody specific for endothelium and muscular layer) was carried out. The Milan criteria were recorded as previously reported. Age, cirrhosis, hepatitis B virus (HBV) antigen, hepatitis C virus (HCV) antibodies, and alpha fetoprotein (AFP) were clinical factors, and size of HCC, number of nodules, satellitosis (defined as tumors <2 cm in size and located <2 cm from the main tumor [14]), presence of capsule, capsule infiltration, and grading according to Edmondson and Steiner [15] were pathological features compared between MVI+ and MVI− patients. In a subgroup of 67 patients with single <5 cm HCC, proliferative activity (MIB1, YLEM KCP505), antioncogenes p53 (DAKO D07M7001) and Bcl2 (DAKO M0887) were studied with monoclonal antibodies in a standardized fashion (two observers, acting separately in a double-blind fashion in optical microscopy at 400 magnification by 10 fields, examining at least 2,000 cells). The MIB 1 score was the average of the nuclear positivity, 5 % being the lower reference value; for p53 and Bcl2 only one reaction was enough for positivity.
After surgery, the patients were followed as previously described [16]. Liver recurrence was classed as early or late (cutoff at 24 months), marginal or distant from the resection surface, single/double or multinodular/diffuse according to the number of lesions scattered in the different segments [16]. When a diffuse intrahepatic or systemic recurrence occurred in the first 6 months we defined it as an early fatal recurrence (EFR) [17]. Finally, the recurrence was also classed according to the Milan criteria [2]. The therapeutic strategy of the recurrence followed the same criteria we used for the primary cancer; PEI and RFA were considered as potentially radical treatments, above all in the case of contraindication to another LR. OS and DFS were assessed in the entire population, then according to the presence or absence of MVI both as a single prognostic factor and as an adjunct to the Milan classification.
This study was approved by the University Institutional Board (approval number: decree N. 39-2012).
Statistical analysis
Statistical analysis was carried out with Microsoft Excel and SPSS version 18.0 for Windows: discrete variables were compared by the χ2 test. Survival rates and curves were determined using the Actuarial method and compared using the Mantel–Haenszel test. Multivariate analysis was performed with the Cox regression proportional hazards model with forward and backward stepwise, forward selection, and backward selection algorithms to identify independent factors. Statistical significance was defined as p < 0.05.
Results
MVI in specimens after primary resection
Among the population of 441 patients, 343 were males and 98 females; mean age was 66 years (range 32–85 years). According to the Milan criteria, 242 patients (54.8 %) were Milan+ and 199 patients were Milan− because of HCC larger than 5 cm (89 patients) or multinodular (110 patients). MVI was present in 189 patients (42.8 %, group 1) and absent in the remaining 252 patients (57.2 %, group 2). The following features were significantly related to the presence of MVI: AFP value (at a cut-off of 200 ng/ml), size of HCC, grading, and presence of satellites (Table 1). The rate of MVI was 37.4 % if 0–1 predictive feature was present (361 patients), 67.1 % if 2–3 factors were contemporary present (76 patients), and 75 % if all 4 criteria were positive (4 patients). No relation was noted between MVI and either Mib1 value or the expression of antioncogenes. According to the Milan classification, MVI was detected in 34.3 % Milan+ and in 53.2 % Milan− HCC (p = 0.00001). At multivariate analysis, grading (risk ratio 8.11, p = 0.001) and Milan classification (risk ratio 3.55, p = 0.02) maintained their value as predictive factors of MVI (Table 2).
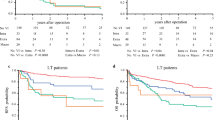
Perioperative and long-term survival of the patients
Twenty-one patients died after surgery (mortality rate 4.7 %), and 16 patients were lost in the postoperative period. Thus the survival analysis concerns the remaining 404 patients, who were followed for 43.4 months on average (range 4–181 months). The OS rate was 89.1, 65.6, and 53.2 % at 1, 3, and 5 years after surgery. Survival was different according to MVI (91.7, 72.2, and 58.9 % in MVI− patients and 85.2, 55.8, 44.8 % in MVI+ patients; p = 0.001) (Fig. 1) and to the Milan criteria (94.6, 76.7, 64.1 % in Milan+ patients and 82.3, 51.9, 39.7 % in Milan− patients; p = 0.00001) (Fig. 2). Among the 242 patients with Milan+ HCC, survival was lower in MVI+ patients (93.2, 71.6, and 54.1 %) than in MVI− patients (95.3, 79.2, 67.9 %; p = 0.03). In contrast, for Milan− patients, MVI status did not modify the final outcome, survival being 78.7, 42.6, and 37.1 % in MVI+ patients and 85.9, 60.9, and 42.4 % in MVI− patients; p = 0.09.
Disease-free survival
Liver recurrence was diagnosed in 217 patients (49.2 %), mainly (76 % of cases) in the first 2 years after surgery (early recurrence). Recurrence was marginal in 11 patients and distant from the resection site in 206 patients. The recurrent HCC appeared as a single/oligonodular lesion in 115 patients and diffuse/multinodular in 91 patients, classed as Milan+ in 114 patients and Milan− in 103 patients. EFR occurred in 37 patients. The recurrence rate was 47.1 and 51.8 % in Milan+ and Milan− patients and 49.7 and 48.8 %, respectively, in MVI+ and MVI− HCC (n.s.). The rate of events was not different when MVI was considered for the two different classes of patients classified according to the Milan criteria; the patients with the two most favorable situations—i.e., Milan+ and MVI− negative HCC, suffered a recurrence rate (52.3 %) comparable to that of the patients with the two unfavorable situations, i.e., Milan− and MVI+ HCC (61.7 %; p = 0.4). DFS at 1, 3, and 5 years was 73, 47.6, and 43.9 % in MVI+ patients and 79.7, 58.3, and 54.3 % in MVI– patients (p = 0.008); according to the Milan criteria, the rate was 84.7 %, 61.6 %, 56.2 % (Milan+ patients) and 72.9, 56.3, and 54.8 % (Milan– patients; p = 0,26). Early and multinodular recurrences were more frequent both in MVI+ patients and in Milan− patients, but only the Milan criteria proved to be a predictive factor for an EFR (10.5 % in Milan+ patients and 24.2 % in Milan− patients; p = 0.007) (Table 3).
Treatment of liver recurrences
Eighty-nine patients were submitted to a curative procedure for a liver recurrence (relative rate 41 %); re-resection in 39 patients, PEI in 31 patients, and RFA in 19 patients. A curative treatment was feasible in 35.7 % of the early recurrences and in 57.7 % of the late recurrences (p = 0.005) and was related to the Milan classification of primary HCC (55.2 % for Milan+ and 25.2 % in Milan− HCC; p < 0.0001), not to MVI status (51.4 % in MVI− and 37.2 % in MVI+; p = 0.3) (Table 2). The rate of radical therapy didn’t change inside any Milan classification in relation to MVI status (Table 4).
After the curative treatment of the recurrence, survival rate was 93.2, 82.0, and 75.2 %. No features of the recurrence were related to survival; only delay of appearance (before or after 1 year) was significant (mean survival of 52.1 and 62.3 months, respectively; p = 0.04). Survival was related to grading, number of nodules, and Milan classification of the primary HCC, but not to MVI status (mean survival of 62 and 55 months in MVI− and MVI+ patients) (Table 5); any of the predictive factors maintained value in the multivariate analysis. For the 39 patients who underwent a second LR, survival was almost the same in MVI+ and MVI− recurrent HCC.
Discussion
Our study shows that MVI is frequently observed in the surgical specimen after LR for HCC. The MVI rate in the present series (42.8 %) is significantly higher than after OLT (24 %) [11]. It is likely, as suggested by Poon et al. [6], that this reflects the selection forced by time wasted on the waiting list for OLT. According to our results, HCCs with MVI are generally of large size (>5 cm), with satellite nodules, a high value of AFP, and poor grading, factors that, individually or in combination, have been considered in several surgical series to be of negative prognostic value. The probability of MVI increases significantly when more than one factor is present in the same patient. In fact these correlations are statistically significant but without an absolute value; poor cellular grading as well as satellite lesions have been discovered at a significant rate (37.5 and 57.5 %) of MVI− HCC too. Furthermore, MVI is not related to the replicative activity of HCC, as assessed by Mib 1 score, and to p53 and bcl 2 positivity, reliable markers of aggressiveness in many cancer conditions. So, according to our data, MVI is only one of the several indexes of cancer malignancy. In a previous series of 213 patients, we demonstrated that MVI was related neither to survival nor to the recurrence rate after LR [16]. In this study, we examined almost twice the number of patients for a longer period of observation. OS was different when MVI was the discriminant factor, but the difference in survival between the two groups of patients so defined is not as sharp as we noted after OLT [11]. An acceptable survival can also be obtained also in MVI+ patients.
When recurrence was the end-point, the distribution in time of the events marks two curves that are opened widely only in the first 2 years after surgery, the slope of the curve being superimposable after this period. This confirms that MVI is related only to early recurrence, which expresses in many cases the metastatic potential of the primary tumor, although the absolute number of recurrences is not higher in these patients.
Recurrence in MVI+ HCC is more frequently extrahepatic, early, and multinodular, meaning an unfavorable clinical presentation. Nevertheless, as a whole, the feasibility of a curative procedure, herein including the chance of a salvage OLT, is not different according to MVI status in the primary HCC. When a radical treatment of recurrence is possible, the results are not different according to MVI status either of the primary tumor and the recurrent HCC. These data reduce the value of MVI from a clinical point of view. A long DFS can be expected in a substantial percentage of patients with MVI+ HCC (>50 % of patients are free of recurrence in the first 5 years after surgery), as recently suggested by Choi et al. [18], so suggesting caution in predicting a poor outcome for patients with MVI+ HCC treated with a radical resection. In contrast, MVI may represent a useful suggestion to a tailored follow-up, indicating a higher risk of early recurrence.
Our experience suggests that the Milan classification in itself could represent a more reliable guide to the therapeutic approach and that the combination with MVI determination is able to further select the outcome of the different patients. This is of particular value in patients classed as Milan+, both for size or number of the nodules. For these patients, 5-year survival was statistically comparable to OLT [1, 3, 4, 19–23] only for MVI− HCC (67.9 %). In Milan− patients, survival after resection was lower (39.7 %) but better than after chemoembolization [16, 24]. In these patients survival is not related to MVI status, which doesn’t allow a clearer definition of the prognosis of the patients. In other words, an unfavorable tumor stage has greater prognostic weight than the biologic data reflected by MVI. Milan classification is not related to the risk of recurrence as a whole but it is more strictly predictive of the feasibility of a cure of the recurrence—including OLT—than MVI. After treatment of the recurrence, the results are strictly related to Milan classification of the primary tumor; thus this datum, more than MVI in the resected specimen, may dictate the right therapeutic solution for the recurrence.
Our results are in contrast with a recent report by Lim et al. [25] of 454 patients submitted to LR in Singapore. In our retrospective study, MVI proved to be a better predictor of OS and DFS than the Milan classification. The difference in the results may be due to the different clinical context. In the Asian report, the patients were younger (61.3 vs 66 years in our study), with a higher incidence of HBV infection (66 vs 23.1 %) and a lower rate of liver cirrhosis (50 vs 63.3 %); all these factors may have influenced the rate and the type of liver recurrence, thereby modifying the relative value of MVI. Furthermore, the patients are differently distributed (the rate of MVI was 31 vs 42.8 %), and in the report by Lim et al. the statistical comparison was difficult among the subgroups of patients defined for the different combination of Milan criteria and MVI status. Finally, the follow-up was short (27 months), so there were not many patients in the group suffering late recurrence.
In conclusion, our study confirms that MVI is a prognostic factor in relation to survival after radical LR for HCC, but the clinical value of this information is limited. The long-term results are acceptable in MVI+ patients, and more than 50 % of MVI+ patients did not have a recurrence. The presence of MVI may allow selection of patients with a higher risk of extrahepatic, multinodular disease and early recurrence, but this demonstration does not reduce either the feasibility of a curative therapy or the chance of a long survival after curative treatment of a recurrence The best information provided by MVI is the opportunity of allowing strict follow-up, particularly for the first two postoperative years. In contrast, the Milan criteria seem to be more useful in the clinical management of HCC patients, provided that they are not used to exclude Milan− patients from liver resection. A long survival can be achieved in 40 % of patients with a large tumor or multinodular cancer. When recurrence appears after resection of a Milan– HCC, the results of radical treatment are not as good. The combination of Milan classification and MVI analysis can allow a more precise prognostic definition for the patients undergoing resection for an early cancer.
References
Fan ST, Poon RTP, Lam CM et al (2011) Outcome after partial hepatectomy for hepatocellular cancer within the Milan criteria. Br J Surg 98:1292–1300
Mazzaferro V, Regalia E, Doci R et al (1996) Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 334:693–699
Yamamoto J, Kosuge T, Sakamoto Y et al (2007) Effectiveness of hepatic resection for early-stage hepatocellular carcinoma in cirrhotic patients: subgroup analysis according to Milan criteria. Jpn J Clin Oncol 37:287–295
Cha CH, Ruo L, Jarnagin WR et al (2003) Resection of hepatocellular carcinoma in patients otherwise eligible for transplantation. Ann Surg 238:315–323
Otto G, Heuschen U, Hofmann WJ et al (1998) Survival and recurrence after liver transplantation versus liver resection for hepatocellular carcinoma. A retrospective analysis. Ann Surg 227:424–432
Poon RT, Fan ST, Lo CM et al (2007) Difference in tumour invasiveness in cirrhotic patients with hepatocellular carcinoma fulfilling the Milan criteria treated by resection and transplantation. Impact on long term survival. Ann Surg 245:51–58
Sumie S, Kuromatsu R, Okuda K et al (2008) Microvascular invasion in patients with hepatocellular carcinoma and its predictable clinicopathological factors. Ann Surg Oncol 15:1375–1382
Esnaola NF, Lauwers GH, Mirza NQ et al (2002) Predictors of microvascular invasion in patients with hepatocellular carcinoma who are candidates for orthotopic liver transplantation. J Gastrointest Surg 6:224–232
Mitsunobu M, Toyosaka A, Oriyama T et al (1996) Intrahepatic metastases in hepatocellular carcinoma: the role of the portal vein as an efferent vessel. Clin Exp Metastasis 14:520–529
Pawlik TM, Delman KA, Vauthey JN et al (2005) Tumor size predicts vascular invasion and histologic grade: implication for selection of surgical treatment for hepatocellular carcinoma. Liver Transpl 11:1086–1092
Piardi T, Gheza F, Ellero B et al (2012) Number and tumor size are not sufficient criteria to select patients for liver transplantation for hepatocellular carcinoma. Ann Surg Oncol 19:2020–2026
Cherqui D, Laurent A, Mocellin N et al (2009) Liver resection for transplantable hepatocellular carcinoma. Long term survival and role of secondary liver transplantation. Ann Surg 250:738–746
Jonas SJ, Bechstein WO, Steinmuller T et al (2001) Vascular invasion and histopathologic grading determine outcome after liver transplantation for hepatocellular carcinoma in cirrhosis. Hepatology 33:1080–1086
Roayaie S, Blume IN, Thing SN et al (2009) A system of classifying microvascular invasion to predict outcome after resection in patients with hepatocellular carcinoma. Gastroenterology 137:850–855
Edmondson HA, Steiner PE (1954) Primary carcinoma of the liver: a study of 100 cases among 48900 necropsies. Cancer 7:462–503
Portolani N, Coniglio A, Ghidoni S et al (2006) Early and late recurrence after liver resection for hepatocellular carcinoma: prognostic and therapeutic implications. Ann Surg 243:229–235
Kim BW, Kim YB, Wang HJ et al (2006) Risk factors for immediate post-operative fatal recurrence after curative resection of hepatocellular carcinoma. World J Gastroenterol 12:99–104
Choi KK, Kim SH, Choi SB et al (2011) Portal venous invasion: the single most independent risk factor for immediate postoperative recurrence of hepatocellular carcinoma. J Gastroenterol Hepatol 26:1646–1651
Eguchi S, Takatsuki M, Hidaka M et al (2010) Predictor for histological microvascular invasion of hepatocellular carcinoma: a lesson from 229 consecutive cases of curative liver resection. World J Surg 34:1034–1038. doi:10.1007/s00268-010-0424-5
Bilimoria M, Lauwers GY, Doherty DA et al (2001) Underlying liver disease, not tumor factors, predicts long-term survival after resection of hepatocellular carcinoma. Arch Surg 136:528–535
Kamiyama T, Nakanishi K, Yokno H et al (2009) Recurrence patterns after hepatectomy of hepatocellular carcinoma: implication of Milan criteria utilization. Ann Surg Oncol 16:1560–1571
Konarias LG, Levi DM, Pedroso TE et al (2011) Is surgical resection superior to transplantation in the treatment of hepatocellular carcinoma? Ann Surg 254:527–538
Tanaka S, Noguchi N, Ochiai T et al (2007) Outcomes and recurrence of initially resectable hepatocellular carcinoma meeting Milan criteria: rationale for partial hepatectomy as first strategy. J Am Coll Surg 204:1–6
Torzilli G, Donadon M, Marconi M et al (2008) Hepatectomy for stage B and stage C hepatocellular carcinoma in the Barcelona Clinic Cancer Classification. Results of a prospective analysis. Arch Surg 143:1082–1090
Lim KC, Chow PKH, Allen JC et al (2011) Microvascular invasion is a better predictor of tumor recurrence and overall survival following surgical resection for hepatocellular carcinoma compared to the Milan criteria. Ann Surg 254:108–113
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Portolani, N., Baiocchi, G.L., Molfino, S. et al. Microvascular Infiltration has Limited Clinical Value for Treatment and Prognosis in Hepatocellular Carcinoma. World J Surg 38, 1769–1776 (2014). https://doi.org/10.1007/s00268-013-2426-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-2426-6