Abstract
Background
Papillary thyroid carcinoma (PTC) is associated with an excellent prognosis but frequently spreads to regional lymph nodes. The extent of neck dissection, particularly routine level II or V lymphadenectomy, is still controversial as it may lead to spinal accessory nerve injury and associated postoperative morbidities. We assessed the diagnostic value of preoperative ultrasonography (US) plus computed tomography (CT) for detecting metastatic lymph nodes and for identifying predictors of level II or V metastasis in patients with PTC.
Methods
The results of US and CT were compared with histopathologic findings at various neck levels in 209 previously untreated PTC patients with lateral cervical nodal metastases who underwent total thyroidectomy with central and lateral neck dissection. Clinicopathologic predictors for level II or V metastases were identified.
Results
Pathologic metastases to level II and V were observed in 53.6 and 25.4 % of patients, respectively. Occult metastases were found in 34.5 and 16.8 %, respectively. The sensitivities of US plus CT for levels II and V were 64.6 and 50.9 %, respectively. Image-based, isolated lateral level IV involvement and macroscopic extranodal extension were independently associated with level II metastasis or either level II or V metastasis (p < 0.01). Macroscopic extranodal extension was also independently associated with level V metastasis (p = 0.001).
Conclusions
Patients with image-based, isolated lateral level IV involvement and no macroscopic extranodal extension are potential candidates for limited level III–IV dissection or prophylactic level II lymphadenectomy omission. Level V lymphadenectomy may be omitted in patients without macroscopic extranodal extension.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Papillary thyroid carcinoma (PTC) frequently spreads to cervical lymph nodes. Cervical lymph node metastases develop in approximately 30–80 % of PTC patients [1–3]. The pattern of neck metastasis from PTC is generally sequential, progressing first to the lymphatic basin of the central neck compartment and subsequently to that of the lateral neck, including the jugular chain and supraclavicular fossa [1, 4, 5]. Cervical lymph node metastasis has no major impact on survival in low-risk patients but is an important factor for locoregional recurrence [6, 7]. Historically, surgical treatment for cervical lymph node metastasis has varied from “berry picking” to modified radical neck dissection [8]. Most surgeons recommend therapeutic en bloc neck dissection for patients with positive lateral lymph nodes, including neck levels II–V with preservation of the spinal accessory nerve, internal jugular vein, and sternocleidomastoid muscle [9, 10]. This strategy is based on the patterns and metastasis of PTC showing that levels II–IV (jugular nodes) and VI (central compartment lymph nodes) are often involved [1–5]. However, the optimal extent of lateral neck dissection (LND) is still controversial. Some surgeons advocate a limited lateral neck dissection approach, wherein only the neck levels containing metastatic nodes diagnosed by ultrasonography (US) are dissected [1, 11].
Neck dissection of the jugulodigastric lymph node pads (level II) or posterior triangle (level V) involves the spinal accessory nerve. Dissection, traction, or transection of the nerve may cause shoulder dysfunction and sensory changes, which impairs the quality of life [12, 13]. Because most PTC patients have a normal life-span, surgical morbidity is important to both patients and clinicians. To prevent potential neck and shoulder dysfunction, clinically nonmetastatic neck levels II or V may not be included in routine therapeutic neck dissection for patients with metastatic PTC. In this regard, predictive factors for occult metastasis in levels II or V have recently been elucidated [14, 15]. In addition, the optimal extent of LND may depend on the diagnostic value of preoperative imaging for detecting lymph node metastasis at different cervical levels. Further criteria are needed to select appropriate candidates for limited LND.
We previously analyzed predictive factors for metastases to level V in PTC patients [16] and found that level V lymphadenectomy may be omitted in patients who have lymph node metastasis in the ipsilateral lateral neck but no macroscopic extranodal extension. Following the enrollment of more patients, this original study has been extended to seek independent variables predictive of level II as well as level V involvement in patients with metastatic PTC. We also evaluated the diagnostic performance of US and computed tomography (CT) scanning. The aim of the present study was to assess the diagnostic value of preoperative US plus CT for detecting metastatic lymph nodes at different neck levels and to find variables predictive of metastases to level II or V in patients with one or more clinically positive lymph nodes in the lateral neck. Histopathology of neck dissection samples served as a reference to compare the presence of metastasis with results of preoperative imaging at different levels.
Materials and methods
Study population
Clinical and pathologic data were reviewed from the medical records of consecutive patients who underwent therapeutic LND for clinically metastatic PTC to the lateral neck nodes at the Department of Otolaryngology of Asan Medical Center between January 2006 and December 2011. All patients underwent US and fine-needle aspiration (FNA) cytology for diagnoses on primary thyroid nodules and lateral neck nodes. All patients were diagnosed with PTC in the primary thyroid and one or more lymph nodes in the lateral neck by preoperative FNA. Patients with nonpapillary or poorly differentiated cancer, those undergoing repeat surgery for recurrent PTC, and those with distant metastases at initial presentation were excluded. A total of 209 consecutive patients were finally included: 65 male and 144 female patients, with a mean age at initial treatment of 45 years (range 11–81 years). Tumors were staged according to the American Joint Committee on Cancer staging system [17]. This institutional review board of Asan Medical Center approved the study.
Lymph node dissection
All patients underwent total thyroidectomy with central and lateral compartment neck dissection. Node clearance of the bilateral central compartments was performed cranially to the superior thyroid arteries and the pyramidal lobe, caudally to the innominate vein, laterally to the carotid sheaths, and dorsally to the prevertebral fascia [2]. Particular attention was paid to ensure identification of the parathyroid glands. The thymus was routinely preserved by separation from the central lymph nodes. LND encompassing levels II–V was performed en bloc, sparing the spinal accessory nerve, sternocleidomastoid muscle, and internal jugular vein [14]. LND was delimited superiorly to the hypoglossal nerve, inferiorly to the subclavian vein, and laterally to the trapezius muscle. The central and lateral compartment lymph node dissection involved neck levels II (upper jugular), III (mid-jugular), IV (lower jugular), V (posterior neck), and VI (central neck), according to the level system categorized by the American Head and Neck Society [18]. Bilateral neck dissections were performed in 39 (18.7 %) patients with clinically diagnosed bilateral nodal involvement in the lateral neck. The neck levels were marked during surgery, and the neck dissection specimens were separated according to the different neck levels and then sent for analysis as permanent sections.
Preoperative imaging and histopathology
High-resolution preoperative US examinations were performed in all patients using an HDI 5000 scanner (Philips Medical Systems, Best, The Netherlands) with a 12- to 15-MHz linear phased-array transducer. Lymph nodes were characterized according to neck levels. Metastasis to lymph nodes was deemed present by US when at least one of the five US criteria was met: a round shape (long/transverse diameter ratio <1.5), microcalcification or macrocalcification, cystic change, focal or diffuse hyperechogenicity, or abnormal vascular pattern [19, 20]. Contrast-enhanced CT evaluation of the head and neck was performed in 175 patients (83.7 %) using multidetector CT scanners, either the LightSpeed QX/i scanner (GE Medical Systems, Milwaukee, WI, USA) or the Somatom Sensation 16 system (Siemens Medical Solutions, Forchheim, Germany), with a reconstructed slice thickness of 2.5–3.0 mm. After unenhanced CT was performed to detect calcifications in thyroid nodules and cervical lymph nodes, contrast enhancement was performed by intravenous injection of 90 ml iodinated contrast agent (Ultravist 370, Schering, Berlin, Germany) at 3 ml/s with an automated injector using a scan delay time of 45 s. The lymph nodes on CT images were characterized according to neck levels by using the designated criteria for lymph node metastases: calcification, cystic or necrotic change, heterogeneous enhancement, strong enhancement without hilar vessel enhancement, and nodal size [21, 22]. Two board-certified radiologists who had more than 10 years of clinical experience in head and neck imaging and were blinded to the results of surgical pathology interpreted the US and CT results.
The thyroid was examined for tumor size, multifocal cancer, extracapsular invasion, and lymphovascular invasion. Lymph nodes were harvested from the neck dissection specimens by neck level. Each lymph node was examined at 200-μm intervals. Positive nodes were defined as those containing metastatic tumors of any size. Extranodal extension was defined as tumor extension beyond the lymph node with a desmoplastic stromal response. The total number and size of the excised and metastatic lymph nodes, extranodal extension, and the neck level of positive lymph nodes were reported. Lymph node metastases at different neck levels were compared with the results of preoperative US examination. In addition, the pathologic findings of metastatic levels were compared with the results of combined US plus CT. Independent comparisons between CT and pathologic results were not performed.
Statistical analysis
Continuous variables were expressed as the median and range and categoric variables as numbers and percents. The results of US or US plus CT were compared to those of the final pathology by neck level-by-level analyses. The diagnostic value of the imaging modalities for predicting metastatic lymph nodes at different neck levels was characterized by sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV), respectively. The sensitivity and specificity of US versus US plus CT were compared with the McNemar test. Clinical, imaging, and pathologic variables were analyzed to identify risk factors associated with level II or level V lymph node metastasis. Univariate analysis of patients with and without level II or V metastasis was performed using the two-sided Pearson χ 2 test or Fisher’s exact test. Significant variables with p < 0.1 in the univariate analysis were included in a multivariate logistic regression analysis. The results are reported as the odds ratio (OR) with 95 % confidence interval (CI). Two-sided p values of <0.05 were considered statistically significant. All statistical analyses were performed using IBM SPSS software version 21.0 (IBM, Armonk, NY, USA).
Results
Pathology examination
The median size of the primary thyroid tumor was 2.1 cm (range 0.1–9.8 cm). Microcarcinoma was found in 54 (25.8 %) of 209 study patients (Table 1). Multifocality, extracapsular invasion, and lymphovascular invasion of primary tumors were found in 102 (48.8 %), 171 (81.8 %), and 29 (13.9 %), respectively. Altogether 120 patients had tumors involving the upper lobe of the thyroid gland. Invasions of the recurrent laryngeal nerve, trachea, and esophagus were found in 39 (18.7 %), 14 (6.7 %), and 5 (2.4 %) patients, respectively. Most patients (82.3 %) had advanced stage III or IV tumor pathology.
As determined from the neck dissection specimens, the median total numbers of excised lymph nodes and metastatic nodes were 50 (17–154) and 9 (1–50), respectively. The median size of the largest positive lymph nodes was 1.3 cm (range 0.5–6.0 cm). Metastatic lymph nodes were found in level VI in 177 (84.7 %) patients. Levels II, III, IV, and V were involved in 112 (53.6 %), 164 (78.5 %), 156 (74.6 %), and 53 (25.4 %) patients, respectively. Contralateral metastasis in the lateral compartment was found in 27 (12.9 %) patients. Extranodal extension was observed in 129 (61.7 %) patients.
Diagnostic value of preoperative imaging for identifying metastatic neck levels
The comparison between US or US plus CT and histopathologic findings is summarized in Table 2. The sensitivity of US for identifying metastatic lymph nodes was high in levels III (73.2 %) and IV (79.5 %) and low in levels II (54.5 %), V (43.4 %), and VI (52.5 %). When the US and CT were combined, the sensitivity increased to 64.6 % in level II, 81.7 % in level III, 87.8 % in level VI, 50.9 % in level V, and 70.1 % in level VI. The specificity of US for diagnosing metastatic levels was high in levels II (85.6 %) and V (84.0 %) and low in levels III (62.2 %), IV (47.2 %), and VI (65.6 %). By combining US and CT, the specificity decreased to 76.3 % in level II, 57.8 % in level III, 35.8 % in level IV, 82.7 % in level V, and 53.1 % in level VI. The PPV was lowest at level V and the NPV at level VI. The rate of occult metastasis to level II and IV in PTC patients with one or more clinically positive lymph nodes in the lateral neck was low: 34.5 % (35/113) and 16.8 % (26/155), respectively.
Variables predictive of level II or V metastases
Clinicopathologic variables and image-based involvement by level involvement were assessed for prediction of level II or V metastases (Table 3). Univariate analysis showed that tumor multifocality, image-based level II involvement, image-based independent lateral level IV involvement, simultaneous metastasis to level III, a largest metastatic nodal size >2 cm, the number of metastatic lymph nodes in the lateral compartment, and pathologic or macroscopic extranodal extension (assessed by the surgeon) were significantly associated with level II metastasis. Univariate analysis showed that male sex, image-based level V metastasis, image-based independent lateral level IV involvement, simultaneous metastasis to level III, the largest lymph node size, the number of metastatic lymph nodes, and extranodal extension were significantly associated with level V metastasis. Univariate analysis showed that tumor appearing in the upper thyroid lobe, tumor multifocality, image-based level II or V involvement, image-based independent lateral level IV involvement, simultaneous metastasis to level III, the largest metastatic nodal size >2 cm, the number of metastatic lymph nodes, and extranodal extension were significantly associated with level II or V metastases.
On multivariate analyses, image-based independent lateral level IV involvement was an independent variable predictive of level II metastasis (OR 0.056, 95 % CI 0.011–0.28; p < 0.001) or either level II or V metastasis (OR 0.12, 95 % CI 0.035–0.42; p = 0.001) (Table 4). Macroscopic extranodal extension was an independent variable predictive of level II metastasis (OR 5.31, 95 % CI 2.39–11.82; p < 0.001), level V metastasis (OR 4.37, 95 % CI 2.01–9.49; p < 0.001), and either level II or V metastasis (OR 4.34, 95 % CI 1.86–10.12; p = 0.001). Tumor multifocality was also an independent variable predictive of either level II or V metastasis (OR 2.12, 95 % CI 1.03–4.38; p = 0.043).
In all, 37 patients presented with image-based, independent lateral level IV involvement. Among them, two (5.4 %) had pathologic level II metastases: one with macroscopic extranodal extension and the other with multifocal tumors. Pathologic level V metastases were found in three (8.1 %) patients, of whom one had macroscopic extranodal extension and one had multifocal tumors. Therefore, either pathologic level II or V metastases were found in five (13.5 %) patients, of whom two had macroscopic extranodal extension and two had multifocal tumors. Only one patient had no macroscopic extranodal extension or multifocal tumors but did have level V metastasis. Therefore, an ideal candidate for limited level III–IV dissection would have image-based, independent lateral level IV involvement but no tumor multifocality or macroscopic nodal extension; only one (3 %) of 35 patients had pathologically confirmed simultaneous positive nodes in levels IV and V.
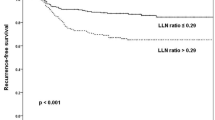
Follow-up and recurrence
All patients underwent postoperative radioactive iodine ablation therapy with 150–200 mCi 131I and thyroid-stimulating hormone suppression thyroxine therapy. The median follow-up period was 54 months (range 12–86 months). The 5-year overall, disease-specific, and disease-free survivals were 91.8, 98.5, and 67.7 %, respectively. Locoregional control was 78.9 %. In all, 37 patients had recurrences or distant metastasis: 5 had developed local or central compartment recurrences, 23 had lateral neck recurrences, and 14 had distant metastases. Five patients had multiple recurrences or metastases of local, regional, and distant sites. Most patients with recurrence or distant metastasis had multilevel lateral neck disease at initial presentation. No patient had recurrence in level V. Eight patients died of distant metastases, and four died of other causes: lung cancer, uterine cervix cancer, interstitial disease, cardiovascular disease. All other patients were still alive at the last follow-up.
Discussion
This study examined the pattern of cervical metastasis of 209 patients with biopsy-proven single or multiple lymph node metastases in the lateral compartment of the neck. The central compartment was most frequently involved in these patients. Skip metastasis to the lateral neck, with no progression through the central neck, was seen in 15.3 % of patients, similar to that found in other reports [2–5, 23, 24]. Therefore, routine clearance of lymph nodes in the central neck compartment for patients with metastatic PTC is warranted, regardless of clinical suspicion of level VI involvement [4, 5]. Levels III and IV were the second sites most frequently involved in our patients (78.5 and 74.6 %, respectively). This suggests that levels III and IV, as well as level VI, should be routinely included in neck dissection procedures for metastatic PTC. The metastatic rates of levels II and V (53.6 and 25.4 %) were low compared with those of levels III, IV, and VI. The relatively limited involvement of these levels combined with the potential postoperative morbidity from dissecting at these levels suggests that limited LND is justified for patients with metastatic PTC.
Preoperative US has previously been shown to have high sensitivity and specificity for detecting cervical nodal metastasis in the lateral neck [25, 26]. US is also effective in detecting nonpalpable metastasis of PTC [26]. The sensitivity of US or CT in per-patient analyses has been high (up to 95) in the lateral neck but relatively low (23–59 %) in the central neck [22, 27]. However, these studies did not clearly analyze lymph node metastasis at the different cervical levels, which may have assisted in determining the necessity and extent of LND in PTC patients. We found that the sensitivity of US alone or US plus CT for detecting lymph node metastasis was high in levels III and IV but relatively low in levels II, V, and VI. This may be because many metastatic lymph nodes are too small to be identified by US or CT in these levels, and the presence of the thyroid gland makes examination of the central lymph nodes difficult [27]. Although CT is not routinely recommended for all PTC patients because of cost, radiation exposure, and delay in administrating radioactive iodine ablation [9], it may be useful for evaluating metastatic lymph nodes. CT is not operator-dependent and provides compete assessments of whole neck levels. CT may evaluate lymph nodes in the anatomic subsites, such as high level II, low level VI, and the retropharyngeal/mediastinal space, which are sometimes difficult to assess by US alone. In addition, CT may improve diagnostic confidence for diagnosis of lymph nodes with nonspecific US features (e.g., large size, absent hilum, round shape) [22]. Our data and data from previous studies have shown that CT can complement US in identifying metastatic lymph nodes, and the combination of imaging modalities is better than either alone [22]. However, 34.5 % (39/113) and 16.8 % (26/155) of patients had occult metastasis at levels II and V, respectively. In addition to preoperative US or CT evaluation, level II or V metastasis may also be predicted by clinical variables and pathology [14–16].
A prior study showed that occult lymph node metastasis in level II was greater in patients with simultaneous metastases to levels III and IV or those with more than four metastatic lymph nodes [14]. We found that these factors were significantly associated with level II metastasis by univariate, but not multivariate, analysis. In addition, a recent report suggested that because simultaneous involvement of lymphatic metastases to levels II–V was independently associated with level V metastasis, level V lymphadenectomy may be omitted in patients without level IV positivity [15]. In our previous report, macroscopic extranodal extension was the only independent variable for level V metastasis in these patients [16]. The same result was found in the present study, which had a larger cohort and also considered level II metastasis. Multivariate analysis showed that tumor multifocality, image-based independent lateral level IV involvement, and macroscopic extranodal extension were independently associated with level II or V metastasis. Of 35 patients without any of these independent variables, only one patient had pathologically confirmed simultaneous positive nodes in levels IV and V. Only 16.7 % (35/209) of patients in the present study with PTC metastasizing to the lateral compartment may have been candidates for limited level III–IV dissection, whereby the remaining patients would be candidates for levels II–V LND. However, given that a large proportion of these patients would still undergo unnecessary dissection of the posterior neck and spinal accessory nerve with this approach, refinement of the criteria for limited LND is warranted. Because pathologic level V involvement is relatively low, the indication for level V lymphadenectomy may be separately selected, as has been previously proposed [16]. The small occult metastatic volume in level V may be treated by postoperative radioactive iodine ablation, with possible consideration of posterior neck dissection as a follow-up procedure.
There is a risk of shoulder dysfunction and pain following surgery to level II or V, regardless of whether the spinal accessory nerve has been damaged during dissection [13, 28]. The average survival rate for PTC patients is good, estimated at 99 % by the MACIS score (distant metastasis, age, completeness of resection, local invasion, tumor size). Thus, minimizing the risks of co-morbidities is of great importance in PTC patients who have excellent prognoses [29]. More aggressive surgery may lead to more complications without additional benefit. Extension of the surgical field and tissue peeling using a more aggressive neck dissection may increase the potential for postoperative pain, neck and shoulder movement limitation, and sensory abnormalities [12, 13, 28]. The impact of dysfunction and pain on quality of life may be significant, especially in young PTC patients with a predominantly normal life expectancy. It is important to balance oncologic safety and quality of life, particularly when the survival benefit of wide neck dissection remains uncertain. Our study may help to determine whether level II or V dissection should be included in PTC patients with lateral neck lymph node metastases.
Conclusions
Our study showed a relatively low rate of occult metastasis to level II (34.5 %) and V (16.8 %) in PTC patients with one or more clinically positive lymph nodes in the lateral neck. Patients with image-based, independent lateral involvement of level IV and no macroscopic extranodal extension are candidates for limited level III–IV dissection or prophylactic level II lymphadenectomy omission (Fig. 1). Level V lymphadenectomy may be omitted in patients with metastatic PTC but no image-based level V involvement or macroscopic extranodal extension. Because our patients underwent dissection of all levels II–VI combined with total thyroidectomy, further prospective studies focusing on the role of limited LND based on our findings are required to reveal their impact on recurrence and quality of life.
References
Shaha AR, Shah JP, Loree TR (1996) Patterns of nodal and distant metastasis based on histologic varieties in differentiated carcinoma of the thyroid. Am J Surg 172:692–694
Wada N, Duh QY, Sugino K et al (2003) Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg 237:399–407
Roh JL, Park JY, Park CI (2007) Total thyroidectomy plus neck dissection in differentiated papillary thyroid carcinoma patients: pattern of nodal metastasis, morbidity, recurrence, and postoperative levels of serum parathyroid hormone. Ann Surg 245:604–610
Sivanandan R, Soo KC (2001) Pattern of cervical lymph node metastases from papillary carcinoma of the thyroid. Br J Surg 88:1241–1244
Roh JL, Kim JM, Park CI (2008) Lateral cervical lymph node metastases from papillary thyroid carcinoma: pattern of nodal metastases and optimal strategy for neck dissection. Ann Surg Oncol 15:1177–1182
Lundgren CI, Hall P, Dickman PW et al (2006) Clinically significant prognostic factors for differentiated thyroid carcinoma: a population-based, nested case-control study. Cancer 106:524–531
Baek SK, Jung KY, Kang SM et al (2010) Clinical risk factors associated with cervical lymph node recurrence in papillary thyroid carcinoma. Thyroid 20:147–152
Shaha AR (1998) Management of the neck in thyroid cancer. Otolaryngol Clin North Am 31:823–831
American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer, Cooper DS, Doherty GM, Haugen BR et al (2009) Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19:1167–1214
Anonymous (2012) National Comprehensive Cancer Network. Thyroid carcinoma. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines™), version 3. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp/. Accessed 1 Apr 2013
Caron NR, Tan YY, Ogilvie JB et al (2006) Selective modified radical neck dissection for papillary thyroid cancer: Is level I, II, and V dissection always necessary? World J Surg 30:833–840. doi:10.1007/s00268-005-0358-5
Laverick S, Lowe D, Brown JS et al (2004) The impact of neck dissection on health-related quality of life. Arch Otolaryngol Head Neck Surg 130:149–154
Cappiello J, Piazza C, Giudice M et al (2005) Shoulder disability after different selective neck dissections (levels II–IV versus levels II–V): a comparative study. Laryngoscope 115:259–263
Koo BS, Seo ST, Lee GH et al (2010) Prophylactic lymphadenectomy of neck level II in clinically node-positive papillary thyroid carcinoma. Ann Surg Oncol 17:1637–1641
Lim YC, Choi EC, Yoon YH et al (2010) Occult lymph node metastases in neck level V in papillary thyroid carcinoma. Surgery 147:241–245
Shim MJ, Roh JL, Gong G et al (2013) Preoperative detection and predictors of level V lymph node metastasis in patients with papillary thyroid carcinoma. Br J Surg 100:497–503
Greene FL, Page DL, Fleming ID et al (2002) AJCC cancer staging manual, 6th edn. Springer, New York, pp 77–87
Robbins KT, Shaha AR, Medina JE et al (2008) Consensus statement on the classification and terminology of neck dissection. Arch Otolaryngol Head Neck Surg 134:536–538
Leboulleux S, Girard E, Rose M et al (2007) Ultrasound criteria of malignancy for cervical lymph nodes in patients followed up for differentiated thyroid cancer. J Clin Endocrinol Metab 92:3590–3594
Rosario PW, de Faria S, Bicalho L et al (2005) Ultrasonographic differentiation between metastatic and benign lymph nodes in patients with papillary thyroid carcinoma. J Ultrasound Med 24:1385–1389
Som PM, Brandwein M, Lidov M et al (1994) The varied presentations of papillary thyroid carcinoma cervical nodal disease: CT and MR findings. AJNR Am J Neuroradiol 15:1123–1128
Kim E, Park JS, Son KR et al (2008) Preoperative diagnosis of cervical metastatic lymph nodes in papillary thyroid carcinoma: comparison of ultrasound, computed tomography, and combined ultrasound with computed tomography. Thyroid 18:411–418
Koo BS, Choi EC, Park YH et al (2010) Occult contralateral central lymph node metastases in papillary thyroid carcinoma with unilateral lymph node metastasis in the lateral neck. J Am Coll Surg 210:895–900
Machens A, Holzhausen HJ, Dralle H (2004) Skip metastases in thyroid cancer leaping the central lymph node compartment. Arch Surg 139:43–45
Hwang HS, Orloff LA (2011) Efficacy of preoperative neck ultrasound in the detection of cervical lymph node metastasis from thyroid cancer. Laryngoscope 121:487–491
González HE, Cruz F, O’Brien A et al (2007) Impact of preoperative ultrasonographic staging of the neck in papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg 133:1258–1262
Solorzano CC, Carneiro DM, Ramirez M et al (2004) Surgeon-performed ultrasound in the management of thyroid malignancy. Am Surg 70:576–580
Terrell JE, Welsh DE, Bradford CR et al (2000) Pain, quality of life and spinal accessory nerve status after neck dissection. Laryngoscope 110:620–626
Hay ID, Bergstralh EJ, Goellner JR et al (1993) Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1779 patients surgically treated at one institution during 1940 through 1989. Surgery 114:1050–1057
Conflict of interest
All authors have declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kang, B.C., Roh, JL., Lee, J.H. et al. Candidates for Limited Lateral Neck Dissection among Patients with Metastatic Papillary Thyroid Carcinoma. World J Surg 38, 863–871 (2014). https://doi.org/10.1007/s00268-013-2361-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-2361-6