Abstract
Background
Although differentiated thyroid carcinoma (DTC) rarely develops distant metastases, the present study was performed to evaluate factors that affect the survival of patients with DTC who present with distant metastasis.
Methods
Among 4,989 patients who underwent thyroid surgery for DTC, 82 presenting with distant metastasis were analyzed. Based on radioiodine (131I) avidity and the thyroid-stimulating hormone-stimulated serum thyroglobulin (sTg) level at the time of metastasis, patients were divided into three groups: group 1 (131I uptake + sTg ≤ 215 ng/mL, n = 46), group 2 (131I uptake + sTg > 215 ng/mL, n = 24), group 3 (no 131I uptake, n = 12). Disease-specific survival (DSS) was estimated using the Kaplan–Meier method. Factors predicting the outcome were evaluated using Cox proportional hazard regression analysis.
Results
The age of patients (p = 0.04), frequency of follicular thyroid carcinoma (p = 0.002), tumor size (p < 0.001), and number of multiple metastatic sites (p = 0.004) differed significantly among the groups. With a median follow-up after surgery of 72 months, the 5- and 10-year DSSs for all patients were 84 and 69 %, respectively. The predictors of survival were age (p = 0.004), symptoms at the time of presentation (p = 0.045), histology (p = 0.01), sites of metastasis (p = 0.03), and 131I avidity and sTg level at the time of metastasis (p = 0.002). In the multivariate analysis, age, histology, and 131I avidity and sTg level at the time of metastasis remained significant factors for survival.
Conclusions
Certain DTC patients with distant metastasis demonstrate favorable outcomes dependent on age, histology, and 131I avidity and sTg level at the time of metastasis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The vast majority of patients with differentiated thyroid carcinoma (DTC) present with disease confined to the thyroid gland, with or without invasion of regional lymph nodes. These patients have a favorable prognosis. Distant metastasis occurs in 3–21 % of patients [1–6] and represents the most frequent cause of thyroid cancer-related deaths [7]. The approach to treating DTC patients with distant metastasis is individualized according to disease progression. Total thyroidectomy, which facilitates subsequent radioiodine (131I) treatment [8, 9], is preferred, although other therapeutic modalities (e.g., resection of metastatic lesions, external beam radiotherapy, selective embolization) are considered. Few studies have evaluated the influence of prognostic variables on survival in DTC patients with distant metastasis.
We conducted this study to elucidate the factors affecting outcome in DTC patients with distant metastasis and to compare the clinicopathologic characteristics of patients according to 131I avidity and thyroid-stimulating hormone (TSH)-stimulated serum thyroglobulin (sTg) level at the time of metastasis.
Subjects and methods
Study population
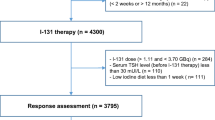
We retrospectively reviewed the medical records of 4,989 consecutive patients who underwent total thyroidectomy for DTC at Samsung Medical Center between 1994 and 2008. There were 4,874 cases of papillary thyroid carcinoma (PTC) and 115 cases of follicular thyroid carcinoma (FTC). Among the 4,989 patients, 82 patients (1.6 %) had distant metastasis. These 82 patients were chosen for evaluation in this study. We obtained approval for this study from the institutional review board.
Methods
Medical records were reviewed, and the following data were collected: demographic information such as sex and age at diagnosis; extent of surgery; various histologic parameters including primary tumor size, local invasion, and cervical lymph node involvement; distant metastasis; 131I therapy and accumulated 131I doses; clinical outcomes at the last follow-up.
Tumor-node-metastasis (TNM) staging was based on the Union Internationale Contre le Cancer/American Joint Committee on Cancer (UICC/AJCC), 7th edition [10]. Patients who exhibited tumor invasion of adjacent organs (e.g., larynx, trachea, esophagus, recurrent laryngeal nerve) were defined as having local invasion rather than distant metastasis. Distant metastasis was evaluated based on clinical, surgical, and imaging evidence. Radiologic evaluation included chest radiography, ultrasonography (US), computed tomography (CT), magnetic resonance imaging, positron emission tomography, and 131I whole-body scan (WBS). Patients were listed as having distant metastasis at diagnosis if the metastasis was identified during the preoperative period or within 6 months after thyroid surgery, including at the first postoperative 131I ablation. 131I avidity was determined by visual uptake at the known site of metastatic disease on WBS after 131I therapy. Absence of visual uptake on WBS was classified as no 131I uptake. The criteria for remission were no clinical or imaging evidence of tumors and sTg levels <2 ng/ml in the absence of interfering antibodies. Persistent disease was defined as a state that did not meet the criteria for remission throughout the observation period.
Treatment of thyroid tumor and metastatic disease
All patients in this study had undergone total thyroidectomy. Prophylactic central neck dissection (ipsilateral or bilateral) was performed in patients with advanced PTC. Therapeutic lateral neck dissection was performed in patients with biopsy-proven lateral cervical lymph node invasion. If any suspicious cervical lymph node was detected by preoperative thyroid US/CT or by surgeons during an operation, central or lateral neck dissection was performed, even in patients with less advanced DTC. All patients with metastatic disease were treated with 131I following levothyroxine withdrawal or recombinant human TSH (rhTSH) stimulation. An initial dose of 30–200 mCi of 131I was used for remnant ablation or treatment of remaining or metastatic disease. A posttherapy scan was performed 2–7 days after 131I administration, and additional 131I was given 6–12 months later in patients with any 131I uptake in residual disease. External beam irradiation was administered to unresectable cancers in the neck or metastatic bone lesions in 11 patients. The typical radiation doses were 30 Gy in 10 days or 60 Gy in 20 days. Distant metastases were surgically removed in 4 patients (2 patients for solitary bone metastasis, 1 for a brain lesion, and 1 for a lung metastasis).
Follow-up
All patients were followed by clinical examination, assessment of serum Tg levels and Tg antibodies (TgAb), and US of the neck. To detect persistent, recurrent, or metastatic lesions, various imaging modalities and histologic proofs were obtained if necessary. TSH suppression therapy by levothyroxine was maintained to achieve a serum TSH level <0.10 mU/L.
Assays for serum Tg and TgAb measurement
Serum Tg levels were measured using a commercialized kit (BRAHMS, Hennigsdorf, Germany). The interassay coefficients of variation were 6.1, 4.2, and 2.2 % at low, median, and high concentrations, respectively. The detection limit was 0.1 ng/ml. Serum TgAb was measured using a commercialized kit (BRAHMS). Titers <100 U/ml were considered negative.
Statistical analysis
Age at diagnosis, primary tumor size, cumulative 131I dose, sTg level at the time of metastasis, and follow-up period are expressed as means (SD) or medians (25th, 75th percentiles). Differences between groups were compared using a one-way analysis of variance or Kruskal–Wallis test. Group comparisons of categoric variables were performed using the χ2 test or, for small cell values, Fisher’s exact test. Results of categoric data are summarized using frequencies and percents. We evaluated the sensitivity and specificity of sTg level at the time of metastasis for survival using receiver operating characteristics (ROC) curve analysis, estimating the area under the curve (AUC) with 95 % confidence intervals (CIs). Disease-specific survival (DSS) curves were estimated using a Kaplan–Meier test and were compared using the log-rank test. Cox proportional hazards models with person-months as the underlying time metric were used to calculate a hazard ratio and 95 % CI for survival. We evaluated effect modification by other thyroid cancer prognostic factors for survival, including sex, age at diagnosis, symptoms at the time of presentation, histology, primary tumor size, multifocality, local invasion, cervical lymph node metastasis, site of metastasis, timing of metastasis, and 131I avidity and sTg level at the time of metastasis. All statistical tests were two-sided, and analyses were executed using SPSS Statistics 19.0 software package (SPSS, Chicago, IL, USA). A value of p < 0.05 was considered statistically significant.
Results
Baseline clinicopathologic characteristics of DTC patients with distant metastasis
The clinicopathologic characteristics of 82 patients who were found to have a distant metastasis are summarized in Table 1. There was a predominance of females (F:M ratio 3:1). The mean age was 48 ± 16 years (range 17–74 years), and 57 % of the patients were >45 years of age at diagnosis. In all, 62 patients (76 %) presented with clinical symptoms at diagnosis: palpable thyroid mass in 47 (76 %), bone pain in 6 (10 %), dyspnea in 4 (6 %), hoarseness in 3 (5 %), palpable metastatic bone lesion in 1 (2 %), and headache in 1 (2 %).
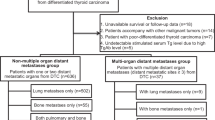
Altogether, 60 patients (73 %) had PTC and 22 (27 %) had FTC. The median (25th, 75th percentile) tumor size was 2.8 (1.6, 4.5) cm (range 0.3–10.0 cm). The most frequent sites of metastatic disease were lung and bone. Lung metastases only, detected in 40 patients, were characterized by diffuse lesions in all but 1 patient. Bone metastases only were solitary in 18 patients, appeared as two or three lesions in 6 patients, and comprised multiple lesions in 2 patients. Of the 16 patients with multiple metastatic sites, 15 had a combination of lung and bone involvement, and 1 patient had involvement of both lung and brain.
All patients were managed with postoperative 131I therapy, receiving a median (25th, 75th percentile) cumulative dose of 465 (200, 808) mCi. In all, 70 patients (85 %) were observed to have 131I uptake in sites of distant metastasis, whereas the remaining patients did not.
The median (25th, 75th percentile) sTg level at the time of metastasis was 106.9 (11.4, 1119.0) ng/ml. The ROC analysis based on the sTg level at the time of distant metastasis for survival is presented in Fig. 1. A stimulated serum Tg level of 215 ng/ml was the optimal cutoff value, giving a sensitivity of 65 % and a specificity of 71 %. The AUC in the ROC analysis was 0.696 (95 % CI 0.537–0.854); p = 0.01).
Grouping DTC patients with distant metastasis according to 131I avidity and sTg level at the time of metastasis
Based on 131I avidity and using an sTg cutoff value of 215 ng/ml, the study population was divided into three groups: group 1 (131I uptake + sTg ≤ 215 ng/ml, n = 46); group 2 (131I uptake + sTg > 215 ng/ml, n = 24); group 3 (no 131I uptake, n = 12). Clinicopathologic characteristics according to group are summarized in Table 1. The mean ages were significantly different between the three groups: 45 years in group 1, 49 years in group 2, and 57 years in group 3 (p = 0.04). The frequency of FTC was significantly higher in group 2 (54 %) than in either group 1 (15 %) or group 3 (17 %) (p = 0.002). Median tumor size was largest in group 2 (4.5 cm), followed by group 3 (3.4 cm) and group 1 (2.0 cm) (p < 0.001). The number of metastatic sites was significantly different between the three groups, as shown in Table 1 (p = 0.004). The frequency of multiple metastatic sites was higher in group 2 than in either group 1 or group 3. Patients in group 2 had significantly higher cumulative 131I doses than those in group 1 or group 3 (p < 0.001). There were no significant differences found between the groups with respect to sex, presentation of disease, multifocality, local invasion, cervical lymph node metastasis, or timing of metastasis.
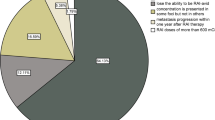
Among the 46 patients in group 1, 22 patients (48 %) achieved remission, 18 patients (39 %) had persistent disease, 4 patients (9 %) died of thyroid cancer, and 2 patients (4 %) died of other causes. In comparison, no patients in group 2 or group 3 achieved remission. In all, 14 patients (58 %) in group 2 had disease persistence, and 8 patients (33 %) died of thyroid cancer. Half of the patients (6/12) in group 3 had persistent disease, and the other half died.
Prognostic factors for DSS
The median follow-up was 72 months (range 45–105 months). During this time, 17 patients (21 %) died of thyroid cancer. The 5- and 10-year DSSs for all patients were 84 and 69 %, respectively (Fig. 2).
Probability of DSS for patients with DTC with distant metastasis. (A) Disease status 5 years after the initial surgery included the following data: remission (n = 20), persistence (n = 32), died of thyroid cancer (n = 11), died of other causes (n = 2), follow-up period <5 years (n = 17). (B) Disease status 10 years after initial surgery included the following data: remission (n = 4), persistence (n = 7), died of thyroid cancer (n = 17), died of other causes (n = 5), follow-up period <10 years (n = 49)
Prognostic factors for survival were analyzed based on the following comparisons: sex (female or male), age (<45 or ≥45 years), presentation of disease (detected on thyroid US or clinically symptomatic), histology (papillary or follicular), primary tumor size (≤ 4 cm or > 4 cm), cervical lymph node metastasis (N0, N1a, N1b, Nx), site of metastasis (lung only, bone only, multiple sites), timing of metastasis (at diagnosis or during follow-up), and 131I avidity + sTg at the time of metastasis (131I uptake + sTg ≤ 215 ng/ml, 131I uptake + sTg > 215 ng/ml, no 131I uptake) (Table 2). Univariate analysis showed that clinical risk factors such as age (p = 0.004), symptoms (p = 0.045), histology (p = 0.01), site of metastasis (p = 0.03), and 131I avidity and sTg level at the time of metastasis (p = 0.002) were associated with DSS (Fig. 3). Among these, age, histology, and 131I avidity and sTg level at the time of metastasis remained significant for survival in multivariate analysis.
Kaplan–Meier estimate of DSS in patients with DTC with distant metastasis according to the significant prognostic variables. a Age (<45 vs. ≥45 years). b Presentation of disease: detected on thyroid US vs. clinically symptomatic. c Histology (papillary vs. follicular). d Site of metastasis (lung only vs. bone only vs. multiple sites). e 131I avidity and sTg at the time of metastasis (131I uptake + sTg ≤ 215 ng/ml vs. 131I uptake + sTg > 215 ng/ml vs. no 131I uptake)
Discussion
In the present study of 82 DTC patients with distant metastasis, we observed 5- and 10-year DSS rates of 84 and 69 %, respectively. The predictors of survival were age, symptoms at diagnosis, histology, site of metastasis, and 131I avidity and sTg level at the time of metastasis. In the multivariate analysis after adjusting for prognostic variables, age, histology, and 131I avidity and sTg level at the time of metastasis remained significant for survival.
Distant metastasis was observed in 1.6 % of DTC patients in our series, which is lower than the previously reported incidence of 2.9–21.2 % in patients with DTC [2, 3, 5, 6, 11, 12]. The 5- and 10-year survival rates in our series were 84 and 69 %, respectively, which are higher than the previously reported rates of 50–68 and 26.0–48.3 %, respectively [1, 2, 5, 11–13]. Our higher survival rates could be attributed to several factors, including the fact that 73 % of our patients had PTC, 131I therapy was administered to all patients, and 85 % had 131I avidity at metastatic foci.
Few studies on prognostic factors and long-term outcomes in DTC patients with distant metastasis have been published. Similar to previous reports [1, 2, 5, 6, 11–15], our univariate analyses demonstrated that age ≥45 years, follicular histology, and a metastatic site other than lung only or bone only were associated with a risk of poor outcome in patients presenting with distant metastasis. Interestingly, clinical symptoms such as palpable primary or metastatic mass, bone pain, hoarseness, or dyspnea were predictive of lower DSS. Shoup et al. [13] reported that patients with disease that was detected based on clinical symptoms had a higher tumor-related mortality rate that that for patients with tumors that were detected incidentally. We speculated that this may represent the burden of primary tumor or metastatic lesions. This observation may be important clinically in regard to predicting prognosis and planning follow-up.
In our study, a multivariate Cox’s proportional hazards model of DSS including all prognostic factors showed that an independent predictor of survival was 131I avidity and sTg level at the time of metastasis. 131I avidity in metastatic lesions has been found to have a significant impact on survival in DTC patients with distant metastasis [2, 5, 12]. Lee and Soh reported that 131I avidity was associated with DSS in patients presenting with distant metastasis at diagnosis and in those who developed distant metastasis during follow-up [2]. Mihailovic et al. [12] found that 131I avidity had a significant influence on DSS and identified an association between the absence of 131I uptake in distant metastasis and low survival rates in patients <45 years of age. Sampson et al. [5] reported that 131I avidity was a significant prognostic factor for survival, with a hazard ratio for tumors with no 131I uptake of 3.4 (95 % CI 1.2–9.2). On the other hand, Huang et al. [6] recently showed that a high sTg level at the discovery of metastasis was a significant predictor of poor outcome. We analyzed specific subgroups according to 131I avidity and sTg level in DTC patients with distant metastasis that were not analyzed in previous studies [2, 5, 6, 16]. We used ROC curves to determine cutoff values for survival that gave the maximum sum of sensitivity and specificity and found that a sTg level of 215 ng/ml gave an optimal sensitivity of 65 % and specificity of 71 %. When we compared clinicopathologic features and clinical outcomes among specific subgroups according to 131I avidity and an sTg level of 215 ng/ml, there were significant differences in age, histology, tumor size, and site of metastases. Patients with no 131I uptake in metastatic lesions were more often >45 years of age compared with those with 131I uptake. This was consistent with the findings of a previous study that showed that higher rates of 131I uptake were seen in the metastatic lesions of younger patients [1]. As age is related to tumor differentiation, 131I avidity is related to age. The frequency of FTC was significantly higher in group 2 (131I uptake + sTg > 215 ng/ml) compared with either group 1 (131I uptake + sTg ≤ 215 ng/ml) or group 3 (no 131I uptake). Our results are in agreement with those of Robbins et al. [17] and Dralle et al. [18], who noted that the Tg levels were significantly higher in patients with FTCs than in those with PTCs. The primary tumor size was larger and the frequency of multiple sites of metastasis was higher in group 2 than in other groups. This result is in agreement with the suggestion of relation between serum Tg level and tumor burden in terms of tumor size and number of metastatic sites. Robbins et al. [17] and Bachelot et al. [19] reported that sTg levels were correlated with volume of disease. Shah et al. [20] and Robbins et al. [17] demonstrated that metastatic involvement of bone was associated with much higher serum Tg levels than lung involvement. Considering that a combination of lung and bone involvement is seen in most patients with multiple metastatic sites, the frequency of bone metastasis was highest in group 2, which is supported by previous data [17, 20]. The 10-year survival rates were 78, 60, and 28 % for groups 1, 2, and 3, respectively. About half of the patients in group 1 achieved remission, whereas no patients achieved remission in groups 2 or 3. In addition, 131I avidity and sTg level at the time of metastasis remained significant for survival in the multivariate analysis after adjusting for prognostic factors. Our results demonstrated the prognostic importance and clinical relevance of 131I avidity and sTg level at the time of metastasis.
Although 131I therapy has been recognized as effective in most DTC patients with distant metastasis, surgery should be considered for isolated distant metastasis. Surgical treatment was carried out in four patients with solitary bone, brain, or pulmonary lesions. Two deaths occurred secondary to disease (mean survival 52 months), and two patients remained alive and disease-free (mean survival 58 months). Surgical resection of isolated symptomatic bone metastasis was associated with improved survival [21, 22]. Surgical resection of brain metastasis is also recommended [23, 24]. Given the rarity of distant metastasis and because of the heterogeneity of the management approaches, we were unable to examine the impact of surgical excision of a solitary metastasis.
Conclusions
The DTC patients with distant metastasis showed relatively favorable outcomes in this study. The major factors determining prognosis, such as age, symptoms at diagnosis, histology, and site of metastasis, were confirmed to be important in DTC patients with metastatic disease. In addition, 131I avidity and sTg level at the time of metastasis were the main predictors of outcome in these patients.
References
Nixon IJ, Whitcher M, Palmer FL et al (2012) The impact of distant metastases at presentation on prognosis in patients with differentiated carcinoma of the thyroid gland. Thyroid 22:884–889
Lee J, Soh EY (2010) Differentiated thyroid carcinoma presenting with distant metastasis at initial diagnosis clinical outcomes and prognostic factors. Ann Surg 251:114–119
Benbassat CA, Mechlis-Frish S, Hirsch D (2006) Clinicopathological characteristics and long-term outcome in patients with distant metastases from differentiated thyroid cancer. World J Surg 30:1088–1095. doi:10.1007/s00268-005-0472-4
Ruegemer JJ, Hay ID, Bergstralh EJ et al (1988) Distant metastases in differentiated thyroid carcinoma: a multivariate analysis of prognostic variables. J Clin Endocrinol Metab 67:501–508
Sampson E, Brierley JD, Le LW et al (2007) Clinical management and outcome of papillary and follicular (differentiated) thyroid cancer presenting with distant metastasis at diagnosis. Cancer 110:1451–1456
Huang IC, Chou FF, Liu RT et al (2012) Long-term outcomes of distant metastasis from differentiated thyroid carcinoma. Clin Endocrinol (Oxf) 76:439–447
Mazzaferri EL, Kloos RT (2001) Clinical review 128: current approaches to primary therapy for papillary and follicular thyroid cancer. J Clin Endocrinol Metab 86:1447–1463
Cooper DS, Doherty GM, Haugen BR et al (2009) Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19:1167–1214
Pacini F, Schlumberger M, Dralle H et al (2006) European consensus for the management of patients with differentiated thyroid carcinoma of the follicular epithelium. Eur J Endocrinol 154:787–803
AJCC (American Joint Committee on Cancer) (2010) Thyroid. In: Edge SB, Byrd DR, Compton CC et al (eds) Cancer staging manual, 7th edn. Springer, New York, pp 87–96
Haq M, Harmer C (2005) Differentiated thyroid carcinoma with distant metastases at presentation: prognostic factors and outcome. Clin Endocrinol (Oxf) 63:87–93
Mihailovic J, Stefanovic L, Malesevic M et al (2009) The importance of age over radioiodine avidity as a prognostic factor in differentiated thyroid carcinoma with distant metastases. Thyroid 19:227–232
Shoup M, Stojadinovic A, Nissan A et al (2003) Prognostic indicators of outcomes in patients with distant metastases from differentiated thyroid carcinoma. J Am Coll Surg 197:191–197
Durante C, Haddy N, Baudin E et al (2006) Long-term outcome of 444 patients with distant metastases from papillary and follicular thyroid carcinoma: benefits and limits of radioiodine therapy. J Clin Endocrinol Metab 91:2892–2899
Ito Y, Masuoka H, Fukushima M et al (2010) Prognosis and prognostic factors of patients with papillary carcinoma showing distant metastasis at surgery (M1 patients) in Japan. Endocr J 57:523–531
Mihailovic JM, Stefanovic LJ, Malesevic MD et al (2009) Metastatic differentiated thyroid carcinoma: clinical management and outcome of disease in patients with initial and late distant metastases. Nucl Med Commun 30:558–564
Robbins RJ, Srivastava S, Shaha A et al (2004) Factors influencing the basal and recombinant human thyrotropin-stimulated serum thyroglobulin in patients with metastatic thyroid carcinoma. J Clin Endocrinol Metab 89:6010–6016
Dralle H, Schwarzrock R, Lang W et al (1985) Comparison of histology and immunohistochemistry with thyroglobulin serum levels and radioiodine uptake in recurrences and metastases of differentiated thyroid carcinomas. Acta Endocrinol (Copenh) 108:504–510
Bachelot A, Cailleux AF, Klain M et al (2002) Relationship between tumor burden and serum thyroglobulin level in patients with papillary and follicular thyroid carcinoma. Thyroid 12:707–711
Shah DH, Dandekar SR, Jeevanram RK et al (1981) Serum thyroglobulin differentiated thyroid carcinoma: histological and metastatic classification. Acta Endocrinol (Copenh) 98:222–226
Zettinig G, Fueger BJ, Passler C et al (2002) Long-term follow-up of patients with bone metastases from differentiated thyroid carcinoma: surgery or conventional therapy? Clin Endocrinol (Oxf) 56:377–382
Bernier MO, Leenhardt L, Hoang C et al (2001) Survival and therapeutic modalities in patients with bone metastases of differentiated thyroid carcinomas. J Clin Endocrinol Metab 86:1568–1573
McWilliams RR, Giannini C, Hay ID et al (2003) Management of brain metastases from thyroid carcinoma: a study of 16 pathologically confirmed cases over 25 years. Cancer 98:356–362
Chiu AC, Delpassand ES, Sherman SI (1997) Prognosis and treatment of brain metastases in thyroid carcinoma. J Clin Endocrinol Metab 82:3637–3642
Acknowledgments
This study was supported by 2012 SMC Clinical Research grant (CR0112101), the Korean Foundation for Cancer Research (CB-2011-03-02), and the Samsung Biomedical Research Institute grant (SBRI C-B0-233-3).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, H.J., Lee, J.I., Kim, N.K. et al. Prognostic Implications of Radioiodine Avidity and Serum Thyroglobulin in Differentiated Thyroid Carcinoma with Distant Metastasis. World J Surg 37, 2845–2852 (2013). https://doi.org/10.1007/s00268-013-2213-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-2213-4