Abstract
Background
Fluid therapy (FT) is a critical intervention in managing acute pancreatitis (AP). There is a paucity of evidence to guide FT and virtually no data on current prescribing practice. This survey aims to characterize current practice and opinion with regard to FT in AP throughout New Zealand.
Methods
Information was collected on fluid selection, administration, and goal-directed FT. The survey was distributed online and in print to all doctors employed in General Surgery Departments in New Zealand on 1 May 2012. Monthly email reminders were sent for 6 months.
Results
The overall response rate was 47 % (n = 190/408). Crystalloids were the preferred initial fluid for all categories of severity; however, colloid use increased with severity (p < 0.001). Fluid volume also increased with severity (p = 0.001), with 74 % of respondents prescribing >4 L for AP with organ failure (OF). Clinicians treating 26–50 patients per year with AP were less likely to prescribe colloid for AP with OF (8 vs 43 %) (p = 0.001). Rate of fluid administration in AP with OF varied according to physicians’ seniority (p = 0.004); consultants prescribed >4 L more than other groups (83 vs 68 %). Only 17 % of respondents reported the use of guidelines.
Conclusions
This survey reveals significant variation in prescription of FT for AP, and aggressive FT is commonly prescribed for AP with OF. There is little adherence to published guidelines or best available evidence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intravenous fluid therapy (FT) is regarded as an essential element of the early management of acute pancreatitis (AP). A recent review of the evidence base for FT in AP has revealed relatively few clinical trials and exposed the low quality of available evidence [1]. It is not surprising then that guidelines are of highly variable quality and offer little with regard to specific recommendations for FT [2].
Fundamental questions remain. We do not know the best fluid to use, the optimal rate to prescribe, or the best goal(s) to guide and monitor fluid resuscitation [1]. These questions must be answered by well-designed, adequately powered, prospective clinical studies. In the absence of high quality evidence, we hypothesize that contemporary prescribing practice will be highly variable. The aim of the present study was to perform a national survey to document contemporary prescribing practice and variation of FT for AP in New Zealand and the application of available evidence. This approach will not only enable an evaluation of compliance with current guidelines but will also be a useful baseline of practice when further evidence is introduced, should a change in prescribing practice be required.
Methods
Survey design
The survey was divided into two parts: (1) 8 items collecting demographic information about the participants and (2) 11 stem questions collecting information on current practice of FT in AP patients. Questions to document fluid prescription practice were written as clinical vignettes (supplementary content) to encourage real-world responses and presented patients with AP without systemic inflammatory response syndrome (SIRS), AP with SIRS, and AP with organ failure (OF).
The survey was reviewed by members of the Pancreas Network of New Zealand (PANNZ) prior to final approval for distribution. Ethical approval was not necessary for this anonymous survey.
Survey distribution
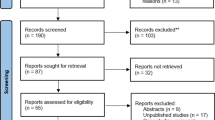
The target population for the survey was all doctors [house officers (n = 106), registrars (n = 130), fellows (n = 12), and consultants (n = 160)] working within the Departments of General Surgery in all the District Health Boards in the public health sector in New Zealand (n = 20). All the departments were contacted by telephone to obtain email addresses for clinical directors and their secretaries as well as the number of medical staff. Because of privacy laws in New Zealand, it was not possible to obtain individual contact details for all potential participants. This made it difficult to determine the response rate accurately as the denominator could not be calculated precisely. An estimated denominator was obtained through human resources units within the departments.
The survey was distributed both electronically (online) as well as in print to the clinical directors of each department. We also approached the registrars and fellows directly in various departments to encourage participation. In addition, reminders were sent at monthly intervals via email to the clinical directors of the surgical departments along with details about the response rates from their department. Final print reminders were mailed at the beginning of the sixth month of the survey.
Data collection and analysis
All responses were collated into a central database. One center had to be excluded from the survey because paper responses were irretrievably lost in transit.
Data were analyzed for variations in practice. Pearson Chi square tests were performed for the following comparisons: (1) type of fluid used for AP without SIRS versus AP with OF, (2) rate of fluid administration for AP without SIRS versus AP with OF, (3) type of fluid used according to physician seniority in AP with OF, (4) type of fluid used according to patient load in AP with OF, (5) rate of fluid administration for AP with OF according to seniority, and (6) rate of fluid administration for AP with OF according to patient load. Statistical significance was set at a p value of 0.05. All analyses were performed with the SPSS statistical package 19.0.0.1 (SPSS Inc., Birmingham, AL).
Results
Demographic
The overall response rate for the survey was 47 % (n = 190/408). The response rate from each level of physician seniority, respondent experience, and patient load is summarized in Table 1.
Fluid selection
FT was considered important by almost all respondents across all levels of pancreatitis severity. Crystalloid solutions were the most commonly used type of fluid for all categories of AP. Colloids were prescribed at higher rates as severity increased (χ² = 244.553 df = 12; p < 0.001), either alone or together with a crystalloid.
Normal saline (0.9 %) was the most common crystalloid used at all levels of severity. There was little variation in the other crystalloid fluids used at all levels of severity. The main colloid used by respondents was Gelofusine (4 % succinylated gelatine with crystalloid component of 154 mmol/L sodium and 120 mmol/L chloride) (B. Braun Melsungen AG, Melsungen, Germany) at all levels of severity. The other colloids prescribed to a lesser extent were albumin, hydroxyethyl starch (e.g., Voluven), pentastarch (e.g., StarQuin), and some respondents indicated they would use any colloid available to them.
Surgical trainees were less likely than consultants to include colloids in the treatment of AP as severity increased (χ² = 97.786 df = 20; p < 0.001). In addition, respondents who treated 26–50 patients with AP with OF in the past 12 months were less likely to prescribe colloids than the rest of respondents (χ² = 41.110 df = 16; p = 0.001).
Rate and volume of administration
Nearly half the respondents (46 %, n = 82/180,) defined aggressive FT to be >4 L in the first 24 h. There was a clear relationship between the severity of AP and the volume of fluid prescribed for the first 24 h (χ² = 27.040, df = 9; p = 0.001) (Fig. 1). The respondents prescribed larger volumes of fluid in the initial 24 h as the severity of distant organ dysfunction increased.
Rate of fluid administration in AP with OF varied according to physician seniority (χ² = 28.688, df = 12; p = 0.004), with consultants more likely to prescribe >4 L in the initial 24 h than other groups. Although it appears that lesser volumes are prescribed in the initial 24 h with increasing patient loads in the past 12 months, this was not statistically significant (χ² = 18.010, df = 12; p = 0.115).
Goals of resuscitation
All respondents indicated that it is important to be able to tell if a patient has responded to FT, with 92 % (n = 163/177) of respondents indicating that they use goals to guide FT. The goals used can be divided into clinical and laboratory goals; their use is summarized in Table 2.
Variation in practice according to employment level showed no substantial changes in the types of goals used between staff. When looking at variation in practice according to patient load, there were no substantial changes in the goals used to guide FT other than base excess being used being used more frequently when laboratory goals were being used by respondents who treated 26–50 patients.
Perception of the literature
Ninety-five percent (n = 179/188) of respondents consider FT to be important in the management of AP. Despite having 30 clinical guidelines to choose from [2], only a minority of respondents (17 %, n = 31/180) indicated that they employ any guidelines, and 90 % (n = 28/31) of these people either consider the evidence to be of poor quality or are unaware of the quality of the evidence. The guidelines used most frequently were those of the United Kingdom working party on AP [3]. Other guidelines used are summarized in Table 3.
Discussion
Here we conducted a national-level survey of current practice of intravenous FT for AP. It documents that in New Zealand, the practice of FT in AP is variable, with the majority of respondents not actively using any of the 30 available guidelines, which are known to be highly variable in quality [2].
Clinical practice should ideally be guided by high-quality, evidence-based guidelines. Within the 30 available guidelines, recommendations for FT in AP are either entirely absent or based predominantly on expert opinion (level 5 evidence) (Table 4). The guidelines that offer a recommendation on fluid selection advise the use of crystalloids, such as Ringer’s lactate and normal saline [5, 6] (Table 4). With regard to the rate of fluid administration, the consensus of the clinical guidelines is that prompt aggressive FT is of importance [3, 5–8]. The guidelines also recommend use of goals to guide FT [3, 6–9]; however there is no consensus with regard to the best goals to use. Given the general poor quality of the guidelines for FT in AP [2], it is not surprising that the practice in New Zealand is in keeping with the prevalent dogma of aggressive resuscitation with a crystalloid. The following discussion examines the practice in New Zealand and the available best evidence regarding the choice of fluid, the rate at which this fluid should be administered, and the goals that can be used to monitor FT.
What fluid to resuscitate with?
When turning to the literature for guidance, clinicians will find only two studies (both of which are recently published RCT) to aid them in their decision [10, 11]. The use of Ringer’s lactate has been shown to reduce systemic inflammation when compared to normal saline [11], and when hydroxyethyl starch was used in combination with Ringer’s lactate, patients showed reduced intra-abdominal pressure and a lower requirement for mechanical ventilation when compared to patients resuscitated with Ringer’s lactate alone [10]. Adding to this evidence, a recent editorial by Lobo [12] highlighted the growing body of evidence mounting against normal saline in favor of crystalloids with compositions closer to that of plasma (i.e., Ringer’s lactate). Two factors may contribute to this recommendation. First, the presence of constituents other than sodium chloride (i.e., Ringer’s lactate contains lactate 28 mmol/L, potassium 4 mmol/L, and calcium 1.5 mmol/L) may offer a resuscitation medium more capable of maintaining physiological norms. The second, and, key factor in the physiological mechanism for this is the reduced ability of the human body to clear the salt load imposed by the use of normal saline, leading to a hyperchloremic acidosis, reduced urine output, increased plasma ADH, and edema [13, 14]. The mechanism behind this factor is considered to be that it is not until recent times that humans have been exposed to salt excess, and thus the suppression of the renin-angiotensin-aldosterone system is slow. It takes 2 days to excrete the salt load imposed by a rapid 2 L normal saline infusion [15]. Further to this, it has been demonstrated that a 2 L infusion of normal saline reduces renal artery blood flow velocity and renal cortical perfusion when compared to an infusion of 2 L of Plasma-Lyte 148 (crystalloid: sodium 140 mmol/L, potassium 5 mmol/L, magnesium 1.5 mmol/L, chloride 98 mmol/L, acetate 27 mmol/L, and gluconate 23 mmol/L) (Baxter Healthcare, Thetford, UK) [16].
In the present survey, 97 % of respondents consider the type of fluid used in resuscitation to be important; however, the majority of participants chose to resuscitate with normal saline. Only 4 % of respondents used Ringer’s lactate solution at all levels of severity, and hydroxyethyl starch solutions made up a minority of colloid use. It is evident that the recent evidence presented by Du, Wu, Lobo, and colleagues [10–12] favoring the use of Ringer’s lactate has not yet become established in clinical practice in New Zealand. It may be that respondents are reluctant to resuscitate with a potassium-containing fluid in patients at risk of renal failure, and that they therefore see normal saline as a preferred option.
What rate to administer fluids?
The prevailing dogma advocates for aggressive FT in AP [1, 3, 5–7, 17–20]. However, the evidence for aggressive FT stems from historically poor quality observational [17–20] while recent evidence from observational [21–23] and randomized [24, 25] studies favor controlled volume expansion during resuscitation in AP. There is an emerging body of evidence demonstrating adverse outcomes for aggressive FT in the management of AP, with increasing rates of mortality, organ dysfunction, acute peripancreatic fluid collections, ICU admissions, abdominal compartment syndrome, sepsis, and APACHE II score at days 1, 2, and 3 [21–25].
In the present survey, the rate of fluid administration has been shown to have a clear tendency to increase as the severity of AP increases. The percentage of respondents who would give >4 L (aggressive FT) in the initial 24 h increased from 6 % in AP without SIRS to 20 % in AP with SIRS to 74 % in AP with OF. Thus, the majority of New Zealand general surgical doctors consider that aggressive FT in AP with OF is appropriate. Again, this indicates that recent evidence is yet to establish itself in clinical practice.
Which goals should guide fluid therapy?
It is acknowledged that the likely solution to providing clinicians with guidance in determining how much fluid to give lies in establishing the optimal method to guide and monitor the response to FT rather than try to set volume targets. Goal-directed FT is not a new concept; it dates back to a landmark study by Shoemaker et al. [26] that demonstrated that using cardiovascular variables to guide FT could reduce mortality in critically ill postoperative patients. Since that study there has been an explosion of physiological parameters promoted as potential goals to guide FT. The sheer number of potential goals available serves as an obstacle to determining which is best in each particular setting. Goals that have been investigated in the setting of AP include blood urea nitrogen, central venous pressure, hematocrit, heart rate, blood pressure, and urine output. It has been shown that blood urea nitrogen offers no advantage with respect to the outcomes of systemic inflammation and C-reactive protein level [11]. Central venous pressure was shown not to be a reliable sole goal for resuscitation, because its use led to inappropriate use of inotropes and vasopressors [27]. Controversy surrounds the usefulness of targeting a particular hematocrit level as a goal; while levels >44 % have been associated with pancreatic necrosis [17], it has also been shown that if a hematocrit goal of <35 % is achieved rapidly there is an increased rate of sepsis and death [24]. The combined use of heart rate, blood pressure, urinary output, and hematocrit together as goals is associated with less severe AP, shorter hospital stays, and reduced requirement for CT imaging and antibiotics [28]. Urine output is a widely used goal for FT in AP; however, a recent review highlights an inconsistent relationship between renal perfusion pressure and diuresis/natriuresis in critical illness [29]. With the obvious benefits to be gained from refining goal-directed FT in AP, determining the optimal goal to guide FT should be considered a high priority for future research due to its potential to refine current practice and reduce the guesswork involved.
Goal-directed FT is widely used by New Zealand doctors working in the specialty of General Surgery in the treatment of AP. Heretofore, there was a tendency to use goals that are easy to apply at the bedside and that are readily available from the patient chart. Urine output, heart rate, systolic blood pressure, jugular venous pressure, and central venous pressure were the most commonly implemented clinical goals and lactate, base excess, hematocrit, and blood urea nitrogen were the most common laboratory goals used. It is worth noting that despite the poor correlation between urine output and the fluid status of patients, urine output was used by 97 % of our respondents. Doctors are trained to recognize the importance of maintaining adequate urine output (generally > 0.5 ml/kg), and it is not surprising that it is in common use in the context of AP. However it is important to draw attention to evidence suggesting that the use of urine output alone has significant limitations, because it is a poor marker of organ perfusion in severe and critical AP.
Only 17 % of respondents in our survey indicated that they use guidelines for FT in AP. Nevertheless, the results of this survey clearly demonstrate that current practice of FT for AP in New Zealand is consistent with current guidelines, such as they are, as well as the prevailing dogma of a crystalloid fluid, infused aggressively. Although this result appears reassuring, it is at odds with recent evidence that favors non-aggressive FT in AP.
Limitations of this work stem from the nature of New Zealand privacy regulations. These regulations prevented us from directly accessing staff lists. This introduces the possibility for inaccuracy in the denominator used in the calculation of response rates and dependence on each department to distribute the survey to its own staff members. Our response rate was 47 % and, based on recent literature, this is acceptable. A recent meta-analysis of 68 online surveys indicates a mean response rate of 35 ± 16 % [30]. Our response rate is similar to other surveys of doctors treating AP around the world [31–36]. Further to this, recent literature suggests that the absolute response rate may not be as strongly associated with survey quality as originally believed [37], and it is the representativeness of the sample that is more important and this does not necessarily increases with response rate [38]. With this in mind, we consider our response rate of 47 % to be very reasonable, particularly considering we have nearly 200 respondents who were diverse with regard to expertise, volume of patients treated, and geographic location.
In conclusion, the use of FT in AP in New Zealand is variable, and the majority of respondents did not refer to current clinical guidelines or best available evidence. Normal saline is the most commonly used fluid; however, this may change as evidence mounts against its use in favor of more physiologically balanced solutions, such as Ringer’s lactate. There was a clear tendency to resuscitate more aggressively as the severity of distant organ dysfunction increased, and while this follows the prevailing dogma of aggressive fluid resuscitation in AP, emerging evidence favors non-aggressive FT. Establishing the optimal goals to guide FT is a logical next step as it will provide a focus that will refine the practice of FT in AP.
With significant unanswered questions about to the type of fluid, the optimal infusion rate, and the best way to guide and monitor resuscitation, and with the current variable practice, there is substantial room for evidence-based standardization of practice.
References
Haydock MD, Mittal A, Wilms HR et al (2012) Fluid therapy in acute pancreatitis: anybody’s guess. Ann Surg 257(2):182–188. doi:10.1097/SLA.1090b1013e31827773ff
Loveday BPT, Srinivasa S, Vather R et al (2010) High quantity and variable quality of guidelines for acute pancreatitis: a systematic review. Am J Gastroenterol 105:1466–1476
Johnson CD (2005) UK guidelines for the management of acute pancreatitis. Gut 54:iii1–iii9
Uhl W, Warshaw A, Imrie C et al (2002) IAP guidelines for the surgical management of acute pancreatitis. Pancreatology 2:565–573
Forsmark CE, Baillie J (2007) AGA institute technical review on acute pancreatitis. Gastroenterology 132:2022–2044
Toouli J, Brooke-Smith M, Bassi C et al (2002) Guidelines for the management of acute pancreatitis. J Gastroenterol Hepatol 17:S15–S39
Banks PA, Freeman ML, Fass R et al (2006) Practice guidelines in acute pancreatitis. Am J Gastroenterol 101:2379–2400
Pezzilli R, Zerbi A, Di Carlo V et al (2010) Practical guidelines for acute pancreatitis. Pancreatology 10:523–535
Hirota M, Takada T, Kitamura N et al (2010) Fundamental and intensive care of acute pancreatitis. J Hepato Biliary Pancreat Sci 17:45–52
Du XJ, Hu WM, Xia Q et al (2011) Hydroxyethyl starch resuscitation reduces the risk of intra-abdominal hypertension in severe acute pancreatitis. Pancreas 40:1220–1225
Wu BU, Hwang JQ, Gardner TH et al (2011) Lactated Ringer’s solution reduces systemic inflammation compared with saline in patients with acute pancreatitis. Clin Gastroenterol Hepatol 9(710–717):e711
Lobo DN (2012) Intravenous 0.9% saline and general surgical patients: a problem, not a solution. Ann Surg 255:830–832
Lobo DN, Stanga Z, Simpson JA et al (2001) Dilution and redistribution effects of rapid 2-litre infusions of 0.9% (w/v) saline and 5% (w/v) dextrose on haematological parameters and serum biochemistry in normal subjects: a double-blind crossover study. Clin Sci 101:173–179
Lobo DN, Stanga Z, Aloysius MM et al (2010) Effect of volume loading with 1 liter intravenous infusions of 0.9% saline, 4% succinylated gelatine (Gelofusine) and 6% hydroxyethyl starch (Voluven) on blood volume and endocrine responses: a randomized, three-way crossover study in healthy volunteers. Crit Care Med 38:464–470
Drummer C, Gerzer R, Heer M et al (1992) Effects of an acute saline infusion on fluid and electrolyte metabolism in humans. Am J Physiol Renal Physiol 262:F744–F754
Chowdhury AH, Cox EF, Francis ST et al (2012) A randomized, controlled, double-blind crossover study on the effects of 2-L infusions of 0.9% saline and Plasma-Lyte® 148 on renal blood flow velocity and renal cortical tissue perfusion in healthy volunteers. Ann Surg 256:18–24
Brown A, Baillargeon JD, Hughes MD et al (2002) Can fluid resuscitation prevent pancreatic necrosis in severe acute pancreatitis? Pancreatology 2:104–107
Gardner TB, Vege SS, Chari ST et al (2009) Faster rate of initial fluid resuscitation in severe acute pancreatitis diminishes in-hospital mortality. Pancreatology 9:770–776
Wall I, Badalov N, Baradarian R et al (2011) Decreased mortality in acute pancreatitis related to early aggressive hydration. Pancreas 40:547–550
Warndorf MG, Kurtzman JT, Bartel MJ et al (2011) Early fluid resuscitation reduces morbidity among patients with acute pancreatitis. Clin Gastroenterol Hepatol 9:705–709
De-Madaria E, Soler-Sala G, Sanchez-Paya J et al (2011) Influence of fluid therapy on the prognosis of acute pancreatitis: a prospective cohort study. Am J Gastroenterol 106:1843–1850
Eckerwall G, Olin H, Andersson B et al (2006) Fluid resuscitation and nutritional support during severe acute pancreatitis in the past: what have we learned and how can we do better? Clin Nutr 25:497–504
Mao EQ, Tang YQ, Li L et al (2007) Strategy of controlling fluid resuscitation for severe acute pancreatitis in acute phase. [Chinese]. Zhonghua wai ke za zhi [Chin J Surg] 45:1331–1334
Mao EQ, Fei J, Peng YB et al (2010) Rapid hemodilution is associated with increased sepsis and mortality among patients with severe acute pancreatitis. Chin Med J (Engl) 123:1639–1644
Mao EQ, Tang YQ, Fei J et al (2009) Fluid therapy for severe acute pancreatitis in acute response stage. Chin Med J (Engl) 122:169–173
Shoemaker WC, Appel P, Bland R (1983) Use of physiologic monitoring to predict outcome and to assist in clinical decisions in critically ill postoperative patients. Am J Surg 146:43–50
Mole DJ, Hall A, McKeown D et al (2011) Detailed fluid resuscitation profiles in patients with severe acute pancreatitis. HPB 13:51–58
Reddy N, Wilcox CM, Tamhane A et al (2008) Protocol-based medical management of post-ERCP pancreatitis. J Gastroenterol Hepatol 23:385–392
Legrand M, Payen D (2011) Understanding urine output in critically ill patients. Ann Intensive Care 11:13
Cook C, Heath F, Thompson RL (2000) A meta-analysis of response rates in Web- or Internet-based surveys. Educ Psychol Meas 60:821–836
Ogawa M, Hirota M, Hayakawa T et al (2002) Development and use of a new staging system for severe acute pancreatitis based on a nationwide survey in Japan. Pancreas 25:325–330
van Geenen E-JM, Mulder CJJ, van der Peet DL et al (2010) Endoscopic treatment of acute biliary pancreatitis: a national survey among Dutch gastroenterologists. Scand J Gastroenterol 45:1116–1120
Loveday BPT, Rossaak JI, Mittal A et al (2011) Survey of trends in minimally invasive intervention for necrotizing pancreatitis. Aust N Z J Surg 81:56–64
Satoh K, Shimosegawa T, Masamune A et al (2011) Nationwide epidemiological survey of acute pancreatitis in Japan. Pancreas 40:503–507
King NKK, Siriwardena AK (2004) European survey of surgical strategies for the management of severe acute pancreatitis. Am J Gastroenterol 99:719–728
Petrov MS, Vege SS, Windsor JA (2012) Global survey of controversies in classifying the severity of acute pancreatitis. Eur J Gastroenterol Hepatol 24:715–721
Johnson TP, Wislar JS (2012) Response rates and nonresponse errors in surveys. JAMA 307:1805–1806
Krosnick JA (1999) Survey research. Annu Rev Psychol 50:537–567
Acknowledgments
The authors are grateful to Tarik Sammour, Benjamin Loveday, and Ursula van den Heever for their voluntary assistance in promoting and distributing the survey in their respective medical centers.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Matthew D. Haydock and Anubhav Mittal contributed equally to this study.
Rights and permissions
About this article
Cite this article
Haydock, M.D., Mittal, A., van den Heever, M. et al. National Survey of Fluid Therapy in Acute Pancreatitis: Current Practice Lacks a Sound Evidence Base. World J Surg 37, 2428–2435 (2013). https://doi.org/10.1007/s00268-013-2105-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-2105-7