Abstract
Background
There is growing evidence that training on virtual reality simulators leads to improved performance in the animate and human operating room. However, they are expensive, have a limited availability, and involve complex systems. Portable simulators are significantly cheaper, more user-friendly, and are flexible systems that are more suited to a surgical trainee’s busy schedule. The use of portable surgical simulators to train skills and reduce errors has never been evaluated in prospective, randomized clinical settings. The objective of this study was to determine if training on the portable Integrated Laparoscopic Simulator leads to improved performance of core laparoscopic skills.
Methods
Core laparoscopic skills were identified by five experienced laparoscopic surgeons and modeled into two exercises and three basic tasks. Twenty surgically naive medical students had baseline laparoscopic skills assessed on a fixed simulator. Participants were randomized to either 14 h training on a portable laparoscopic simulator over a 3 week period, or control with no training. At 3 weeks two expert laparoscopic surgeons blinded to the allocation of participants assessed their pre- and post-intervention performances recorded on a CD-ROM. The outcome measures included time to complete and global rating scores of clipping and dissection tasks.
Results
No differences were observed in baseline skills level between the two groups. The intervention group had better quality of scissors dissection (p = 0.0038) and improved clipping skills (p = 0.0051), and they took less time to accomplish the tasks (p = 0.0099) in comparison to control.
Conclusions
Training on the portable Integrated Laparoscopic Simulator significantly improved core laparoscopic skills in medical students with no prior experience.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Minimally invasive surgery, in particular laparoscopy, has become the standard of care in many areas of surgical practice [1–4]. Significant patient benefits attributed to laparoscopy have led to increasing indications for this approach, even for complex surgical procedures [2]. The learning curve for laparoscopic skills is steep because of the complex psychomotor skills involved, the two-dimensional views, and mechanical constraints of the instruments, which are vastly different from those employed in traditional open surgery [3]. Recognizing these specialized requirements highlights the importance of incorporating laparoscopic skills training in the surgical curriculum for the surgeon’s training and the patients’ safety. Surgical trainees commit twice as many errors as an experienced surgeon, and introduction of surgical simulation in training programs may shorten the learning curve [4, 5].
Simulation-based training has long provided the framework for training in many other complex, high-risk professions (i.e., nuclear power, aviation, and the military), with the goal of minimizing risk and maximizing safety [6]. In surgical training, the situation seems even more complicated because of multiple external factors: the European Working Time Directive, increasing costs of operating room time, ethics of learning basic skills on patients, and patient safety. This has stimulated interest in learning laparoscopy skills in a laboratory setting (skill centers) and subsequently transferring them into actual surgical procedures carried out on patients [3, 7, 8]. This requires a significant investment in surgical simulators. There has already been a considerable amount of research into virtual reality simulators (Lapmentor, MIST VR Promis, SIMENDO, or LapSim) that have led to improved performance in both the animate [9–13] and human operating rooms [6–8, 10–14]. However, virtual simulation training has limitations that have slowed its clinical implementation. There are resource-derived constraints, such as trainees’ busy schedules, over-sophisticated systems, limited availability, and the considerable cost implications [15].
Portable laparoscopic simulators could enhance the adoption of simulation-based training as they are less expensive, moveable, user-friendly, and flexible systems. Their role and introduction into surgical curricula has not yet been defined, and there are few validated study programs to date. The present study aimed to evaluate the role of a portable laparoscopic simulator (iSIM) in enhancing laparoscopic skills acquisition.
Methods
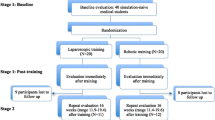
Twenty medical students with no previous laparoscopic experience were recruited into the study following informed consent between 1 August and 31 October 2010. The participants were invited to take part in the study by email addressed to their medical school email inboxes. A first-come, first-recruitment offer policy was adopted. The sample size was calculated based on previous studies on virtual reality surgical simulation [16–18]. The structure and flow of the participants through the trial is illustrated in Fig. 1a.
Identification of core laparoscopic skills and modeling of tasks
Five expert laparoscopic surgeons well recognized and reputed in their field (had experience of more than 200 laparoscopic procedures, teach and train on a minimum of one urology speciality specific laparoscopic courses) identified 10 basic laparoscopic skills necessary for education, training, and procedure-based learning purpose (Table 1). The skills were identified after watching videos of a range of simple and complex laparoscopic procedures. A Delphi process was used to achieve agreement between the experts in scoring tasks and skills required for laparoscopic execution of a procedure (Fig. 1b). The experts remained unaware of each other’s decisions. The following definitions of consensus were established before data analysis:
-
Consensus that task should be retained: >80 of experts scored the task >8
-
Consensus that task should be excluded: >80 % experts scored the task <5
-
No consensus: task failed to meet either of the above criteria
These skills were modeled into two exercises, a scissors dissection task and a clipping task (Fig. 2).
Scissors dissection task (Fig. 2, black circle)
In the scissors dissection exercise, a double-layered latex membrane is attached with tension to a plastic cylinder using an elastic band. The participant is required to carefully dissect between the black lines and separate the triangular shape from its attachments. Any deviation over the lines or damage to the underlying layer of latex was considered an error. This task requires precision and the use of the non-dominant hand to provide traction and position the latex so that the dominant hand can dissect accurately. This task contains nine of the core laparoscopic skills listed in Table 1, except clipping. This task was recorded from start to finish, and the recording was submitted for subsequent analysis.
Clipping task (Fig. 2, white circle)
The participants were asked to select one of the vessels of a synthetic vascular bed and apply two clips, leaving a safe distance between them. To accomplish this, the participant must supinate or pronate both wrists to ensure that both jaws of each clip could be seen prior to applying the clip transversely. This procedure required the subject to use at least nine core laparoscopic skills, except cutting. The procedure was recorded and subsequent analysis of the task performance was carried out.
The Integrated Laparoscopic Simulator (iSIM)
The Integrated Laparoscopic Simulator (iSIM) is a cost-effective portable laparoscopic simulator (£3,000) with a single chip camera system, inbuilt high-definition screen, and recording facility. It displays multiport and single port access, as well as an adaptable skills station (Fig. 3). The simulator takes only a few minutes to set up, is the size of an average laptop computer, and is suitable to practice a wide range of core laparoscopic skills (http://www.isurgicals.com).
Baseline assessment of laparoscopic skills
A 10 min introductory presentation (T.J. and B.J.), which included a brief video of the tasks in simulators and in real patients, was given prior to baseline skills assessment on a fixed laparoscopic simulator in the Cuschieri Skills Centre. Standard Storz laparoscopic instruments and a video endoscopic system (KARL STORZ Endovision DCI Endoscopic System, DCI HOPKINS II Laparoscopes. Enlarged view, diameter 10 mm) with a 2-dimensional monitor were used to perform the task. Instruments were introduced into the trainer box with a 60° manipulation angle, an elevation angle of 45°–60°, and equal azimuth angles. Performances for each task was recorded on a computer disk (CD-ROM) and subsequently measured by two expert laparoscopic surgeons (B.T. and G.N.), who used the validated and reliable Objective Structured Assessment of Technical Skills (OSATS) tool [19] (Table 2). Participants were then randomized into intervention and control group using third party (statistician) computer-generated random numbers. To ensure concealment of allocation, none of the investigators were involved in this process. The investigators involved in the analysis of data and scoring of the tasks were blinded to the details of the participants and performed the evaluation independently.
Progress of intervention and control groups
The intervention group was provided with an instruction sheet and a CD-ROM showing a video of the dissection and clipping tasks being performed by an expert surgeon. They all completed 14 h of practice on the iSIM over a 3 week period. A log book was maintained by an independent person (T.J.) to ensure compliance with the practice. The control group had no access to the portable simulator during this time. At the end of the training period both groups repeated the same tasks on the fixed simulator, and their performances were recorded on CD-ROM. The recorded exercises were again scored with the OSATS tool by independent members of the team (B.T. and G.N.) not associated with the recording process, unaware of group allocation, and each with significant experience using OSATS.
Statistical analysis
Differences between the two groups were assessed with the 2-sample t test and the Mann–Whitney U-test at 1 and 3 weeks to compare the difference in skill levels. Intra-group comparisons were assessed with the paired t test and Wilcoxon matched pairs test at pre- and post-intervention stages to determine the within-group levels of improvement. GraphPad InsTat software (http://www.graphpad.com/quickcalcs/ttest2.cfm) was used for the statistical analysis.
Results
All twenty of the recruited participants completed the study. There was no significant age, gender, or handedness difference between the two groups (Table 3). Consensus following the Delphi process among the experts was achieved in 60, 70, and 80 % in first, second, and third rounds, respectively. On a few tasks there was 100 % consensus. This reflects a high construct and content validity of the process.
Baseline laparoscopic skills
Baseline scores of laparoscopic skills on the fixed simulator did not demonstrate any significant difference between the control group and intervention group for the dissection (p value 0. 0731; 95 % confidence interval 3.17–0.17) or clipping task (p value 0.507; 95 % confidence interval −2.93 to 1.53) on the 2-sample t test (Table 4). In addition, there was no significant difference in the time taken to complete each task (p value 0.659; 95 % confidence interval −59.12 to 38.52) 2-sample t test and Mann–Whitney U-test.
Postintervention assessment of laparoscopic skills (Table 5)
The intervention group had better quality of scissors dissection (p value 0.0038; 95 % confidence interval 3.43–14.56), improved clipping skills (p value 0.0051; 95 % confidence interval 14.90 to −3.29), and took less time to accomplish the task (p value 0.0099; 95 % confidence interval −63.68 to −12.32) in comparison to control on 2-sample t test and Mann–Whitney U-test. Interestingly, intra-group analysis showed some skills improvement trend in the control group as well (Table 6)
Discussion
Principal findings
This is the first randomized controlled trial aimed at assessing the role of a portable laparoscopic simulator in improving laparoscopic skills in subjects (novice medical students) with no previous laparoscopic or surgical experience. The results show a significant improvement in the laparoscopic skills defined tasks. The quality of tasks and the time taken to perform them were significantly better in the group with access to the portable simulators and dedicated training. Availability of portable simulators can contribute to laparoscopic skills development, and their use in surgical education can play a significant role, in particular ny providing reinforcement of learning. Our study showed that access to a portable simulator allows repeated practice of standardized laparoscopic surgical steps and reduces the time taken to perform steps with improvement in quality. Participants who had portable simulation-based training before final assessment with validated tools performed better than their counterparts who had no contact with the portable simulator.
There is already evidence that virtual reality (VR) simulation training can lead to an improvement in laparoscopic skills in both the animate [6, 10–13] and human operating room [14, 20–22]. However, surgical trainees’ access to VR simulators is restricted by the limited availability of such equipment on current training programs, the considerable cost implications of attending a course, and the time constraints of the trainees’ schedule. Portable laparoscopic simulators are less expensive, user-friendly, and flexible. They may provide a more feasible method to improve the acquisition of laparoscopic skills in surgical trainees and have the potential to be easily incorporated into future surgical training programs. This study has demonstrated that the performance of novices was increased significantly after training on the iSIM, which was in line with what has been shown in many VR training studies. Thus, the iSIM could play a significant role in laparoscopic skills acquisition, both for the advantages described above and because it is realistic and cost effective to implement such a device in a surgical department. It could also provide benefit to surgeons with basic and intermediate levels of laparoscopic skills in warming up their skills before they perform an operation on a patient in the operating room, a use suggested previously in a VR simulator study [23]. However, further research needs to be constructed to investigate the impact of such methods.
Generalizability (external validity) of the study
The study was conducted following the CONSORT guidelines [24, 25]. The robust mechanism of task identification by expert and validated tools were used. The tasks were identified by five expert laparoscopic surgeons taking into consideration instrument handling, depth perception, and fine motor control (Table 1). A Delphi process was used with good validity for consensus on the type of tasks. We used OSATS because it is well recognized for its good validity, reliability, and inter-rater reliability when assessing performance using bench models in skills laboratories [19, 26, 27]. Whether basic laparoscopic skills gained by training on a portable laparoscopic simulator can actually improve performance in the human operating room remains to be seen. However, practice on portable simulators could still enhance and re-enforce the skills during laparoscopic surgical training. There is a need for shortening the learning curve of technical skill during training, as this will be a form of quality assurance for the public. An objective assessment is vital because deficiencies in training and performance are hard to rectify without objective feedback [15].
Future research
This study assessed the impact of training on a portable laparoscopic simulator in surgically naive medical students. Therefore the next important step should be to use a large cohort in which to assess the benefits of access to portable laparoscopic simulators to surgical trainees with different levels of training. This would help define the place of a portable simulator in the surgical training curriculum. This could be used as an adjunct to selection of surgical trainees in assessing their spatial perception of tasks during the interview process, as is done in other specialities such as radiology [28] and pathology [29]. In addition, transferability of skills to the operating room and improved patient outcomes (due to training on portable laparoscopic simulators) needs to be determined.
The observation that there was improvement in performance of the controls even after a single use of the stimulator is an interesting one (Table 6). Such findings have potential implications for duration of simulator training required in future research. There is now strong evidence from studies of behaviour in the operating room that failures in non-technical skills are frequently implicated in adverse surgical events and errors [30]. Therefore proficiency in technical skills alone is insufficient to ensure patient safety, and it is imperative that training and assessment in non-technical skills are also incorporated into trainee surgical curricula.
Conclusions
This study demonstrates that training on the portable Integrated Laparoscopic Simulator leads to significant improvement in core laparoscopic skills in medical students with no prior experience.
References
Ghezzi F, Cromi A, Uccella S et al (2009) Incorporating laparoscopy in the practice of a gynecologic oncology service: actual impact beyond clinical trials data. Ann Surg Oncol 16:2305–2314
McNeill AS, Nabi G, McLornan L et al (2010) Endoscopic extraperitoneal radical prostatectomy: critical analysis of outcomes and learning curve. BJU Int 106:1537–1543
Laguna MP, de Reijke TM, de la Rosette JJ (2009) How far will simulators be involved into training? Curr Urol Rep 10:97–105
Tang B, Hanna GB, Cuschieri A (2005) Analysis of errors enacted by surgical trainees during skills training courses. Surgery 138:14–20
Tang B, Hanna GB, Joice P et al (2004) Identification and categorization of technical errors by Observational Clinical Human Reliability Assessment (OCHRA) during laparoscopic cholecystectomy. Arch Surg 139:1215–1220
Andreatta PB, Woodrum DT, Birkmeyer JD et al (2006) Laparoscopic skills are improved with LapMentor training: results of a randomized, double-blinded study. Ann Surg 243:854–860 discussion 860–863
Champion HR, Meglan DA, Shair EK (2008) Minimizing surgical error by incorporating objective assessment into surgical education. J Am Coll Surg 207:284–291
Ziv A, Wolpe PR, Small SD et al (2006) Simulation-based medical education: an ethical imperative. Simul Healthc 1:252–256
Andreatta PB, Woodrum DT, Gauger PG et al (2008) LapMentor metrics possess limited construct validity. Simul Healthc 3:16–25
Youngblood PL, Srivastava S, Curet M et al (2005) Comparison of training on two laparoscopic simulators and assessment of skills transfer to surgical performance. J Am Coll Surg 200:546–551
Jordan JA, Gallagher AG, McGuigan J (2001) Virtual reality training leads to faster adaptation to the novel psychomotor restrictions encountered by laparoscopic surgeons. Surg Endosc 15:1080–1084
Ahlberg G, Heikkinen T, Iselius L et al (2002) Does training in a virtual reality simulator improve surgical performance? Surg Endosc 16:126–129
Hyltander A, Liljegren E, Rhodin PH et al (2002) The transfer of basic skills learned in a laparoscopic simulator to the operating room. Surg Endosc 16:1324–1328
Cosman PH, Hugh TJ, Shearer CJ et al (2007) Skills acquired on virtual reality laparoscopic simulators transfer into the operating room in a blinded, randomised, controlled trial. Stud Health Technol Inform 125:76–81
Windsor JA (2009) Role of simulation in surgical education and training. A N Z J Surg 79:127–132
Miskovic D, Rosenthal R, Zingg U (2008) Randomized controlled trial investigating the effect of music on the virtual reality laparoscopic learning performance of novice surgeons. Surg Endosc 22:2416–2420
Grantcharov TP, Bardram L, Funch-Jensen P et al (2003) Learning curves and impact of previous operative experience on performance on a virtual reality simulator to test laparoscopic surgical skills. Am J Surg 185:146–149
Aggarwal R, Ward J, Balasundaram I et al (2007) Proving the effectiveness of virtual reality simulation for training in laparoscopic surgery. Ann Surg 246:771–779
Martin JA, Regehr G, Reznick R et al (1997) Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg 84:273–278
Gallagher AG, Ritter EM, Champion H et al (2005) Virtual reality simulation for the operating room: proficiency-based training as a paradigm shift in surgical skills training. Ann Surg 241:364–372
Seymour NE, Gallagher AG, Roman SA et al (2002) Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 236:458–463 discussion 463–464
Ahlberg G, Enochsson L, Gallagher AG et al (2007) Proficiency-based virtual reality training significantly reduces the error rate for residents during their first 10 laparoscopic cholecystectomies. Am J Surg 193:797–804
Calatayud D, Arora S, Aggarwal R et al (2010) Warm-up in a virtual reality environment improves performance in the operating room. Ann Surg 251:1181–1185
Moher D, Schulz KF, Altman DG (2001) The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet 357:1191–1194
Marberger M, Schatzl G, Cranston D (2005) Extracorporeal ablation of renal tumours with high-intensity focused ultrasound. BJU Int 95(Suppl 2):52–55
Balasundaram I, Aggarwal R, Darzi LA (2010) Development of a training curriculum for microsurgery. Br J Oral Maxillofac Surg 48:598–606
Beard JD, Marriott J, Purdie H (2011) Assessing the surgical skills of trainees in the operating theatre: a prospective observational study of the methodology. Health Technol Assess 15:i–xxi; 1–162
Smoker WR, Berbaum KS, Luebke NH et al (1984) Spatial perception testing in diagnostic radiology. AJR Am J Roentgenol 143:1105–1109
Berbaum KS, Platz C (1988) Perception testing in surgical pathology. Hum Pathol 19:1127–1131
Christian CK, Gustafson ML, Roth EM et al (2006) A prospective study of patient safety in the operating room. Surgery 139:159–173
Acknowledgments
This work was supported by the Clinical Skills Management Education Network, Scotland, United Kingdom. The authors are grateful to the Surgical Simulation Group (Cushieri Skills Centre) at the University of Dundee for providing intellectual input at different phases of the study. This study was presented at the Clinical Skills Managed Education Network, University of Sterling, March 2011. The abstract has been published in the Journal of Endourology (vol. 25[Suppl 1]:A28, 2011) and in the Journal of Urology (vol. 187[Suppl 4]:E613, 2012).
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Johnston, T.J., Tang, B., Alijani, A. et al. Laparoscopic Surgical Skills are Significantly Improved by the Use of a Portable Laparoscopic Simulator: Results of a Randomized Controlled Trial. World J Surg 37, 957–964 (2013). https://doi.org/10.1007/s00268-013-1945-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-1945-5