Abstract
Background
Trauma is one of the leading prehospital disease profiles in South Africa in general and in KwaZulu-Natal (KZN) in particular. The present study was designed to review the prehospital burden of injury in KZN, identify trauma burden to ambulance ratios, analyze system deficiencies, and propose a prehospital trauma system that is Afrocentric in nature.
Methods
Approval from the relevant ethics authorities was obtained. Using a convenience data set all Emergency Medical Service (EMS) call data for the months of March and September 2010 were reviewed for the three main EMS providers in KZN. Data were extrapolated to annual data and placed in the context of population, ambulance service, and facility. The data were then mapped for area distribution and prehospital workload relative to the entire province. Questionnaire-based assessments of knowledge and deficiencies of the current system were completed by senior officers of the provincial system as part of the analysis of the current system.
Results
The total annual call burden for trauma ranges between 94,840 and 101,420, or around 11.6 trauma calls per thousand of the population per year. Almost 70 % of calls were either for interpersonal intentional violence or vehicular collisions. Only 0.25 % of calls involved aeromedical resources. Some 80 % of patients were considered to be moderately to seriously injured, yet only 41 % of the patients were transported to a suitable level of care immediately, with many going to inappropriate lower level care facilities. Many rural calls are not attended within the time norms accepted nationally. Deficiencies noted by the questionnaire survey are the general lack of a bypass mechanism and the feeling among staff that most EMS bases do not have a bypass option or feel part of a system of care, despite large numbers of staff having been recently trained in triage and major trauma care.
Conclusions
The prehospital trauma burden in KZN is significant and consumes vital resources and gridlocks facilities. A prehospital trauma system that is financially sustainable and meets the needs of the trauma burden is proposed to enable Afrocentric emergency care planning for low and middle income regions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Trauma is the second most frequent cause of mortality in KwaZulu-Natal province (KZN), the largest and most populous province of South Africa [1]. Trauma affects the young and productive population subgroup, and in this respect is similar to HIV/AIDS, the leading killer in the province. KwaZulu-Natal lies on the East coast of South Africa and has a population of almost 11 million [2], with approximately 50 % of the population living in the rural areas outside the two major cities of eThekwini (Durban) and uMsinduzi (Pietermaritzburg). Healthcare provision is divided into eleven health districts (Table 1; Fig. 1—population distribution)
South Africa is one of the few countries in Africa to have a formalized emergency medical service (EMS)[3–5], divided into private and public services, the latter being free-access. There is, at present, no formalized single emergency call center, and each of the services independently dispatches vehicles and personnel to reported incidents (this places South Africa somewhere between World Health Organisation prehospital trauma system grading level 2 and level 3) [6]. In KZN the majority of the emergency service vehicles in the public sector are staffed by basic or intermediate life support paramedics, whereas advanced life support (ALS) paramedics work from rapid response vehicles, mostly situated in the larger towns and the urban areas, many of these being aligned to private services. The majority of the population (87.5 %) is uninsured and relies on public ambulance services. Much has been published in the past about the fatal disease burden of trauma in South Africa[7–9]; however, little is known about either the prehospital or hospital overall burden of trauma in the country.
The purpose of the present study was to determine the trauma prehospital burden to this province suffering from resource constraints and the “devil of distance” for many rural patients living in a province with undulating terrain. From available data, the ratio of trauma to ambulance availability was reviewed. System deficiencies were identified and a proposal for a prehospital trauma system was developed.
Methods
The study received UKZN-BREC (BE011/010) and Provincial Research Office approval, and permission for the use of de-identified call data was granted by the Netcare Ethical Committee and the Medical Director of ER24. The strategy employed a convenience data set of all EMS dispatches for a “trauma call” during the months of March and September 2010. These months were chosen to avoid “holiday bias” in December and the effect of the FIFA2010 Soccer World Cup, played in June–July of 2010.
Using extrapolation, these data were converted to a predicted annual incidence, using two methods to enable range prediction, classified by injury severity (where available) and then mapped per health district within the KZN province to reflect calls per 1,000 population. Finally, the data were placed into “facility” context by assessing trauma burden per staff and vehicle status per district and by access to major hospital (delivery destination). To illustrate the relative severity of the trauma burden, certain of the variables were geographic information system (GIS) mapped with standard mapping software [10]. From the available EMS structural data, a system was proposed for providing more efficient prehospital trauma care from an Afrocentric perspective.
The trauma causes were divided into three groups, namely vehicular related, interpersonal violence (with penetrating trauma as a separate subgroup where available), and other trauma (this includes domestic, industrial, other penetrating or blunt injury). Burn injuries were not included initially; however, these were reported for a number of the regions and the data were extrapolated to establish a regional burn incidence. The various causes of trauma were also evaluated per region to determine the spectrum of injury by region, and to determine whether rural regional variation differs from urban areas.
Results
For the 2 months under review, the total trauma-related call volume for the three EMS services was 16,903 calls from the data provided, which was incomplete for two districts. This would equate to an annual minimum trauma call volume for the KZN province between 94,840 and 101,420 calls, using a predictive system of either monthly averages totalled for one year or the total of the two months multiplied by six, respectively. Using the two systems resulted in a 6.5 % variance between the two possible systems to calculate the annual trauma volume. Put into population context, this equates to 11.6 trauma events requiring emergency ambulance activation per 1,000 population in the province per annum, with certain of these events presenting multiple patients. The distribution of these ambulance calls across the province is GIS-mapped in Fig. 2. In terms of ambulances per district, the distribution is mapped in Figs. 3 and 4.
During the study period, there were 2,042 operational EMS staff across the province; however, most were only basic life support (BLS) qualified, with only around 70 ALS providers for the entire patient cohort. Assuming all worked an equal number of shifts and saw a similar spectrum of disease, then each EMS provider would be exposed to between 46 and 50 trauma calls per operational staff member. There are, however, only between six and ten ambulances per 100,000 population (including private services) operating on a daily basis, thus increasing the risk of delays and increased morbidity. Of these ambulances, 66 % of the public EMS vehicles have over 150,000 km completed service mileage. They are based at 70 public and 12 private EMS bases, with 80 % of the bases having fewer than six ambulances each. There are two rotor wing aeromedical aircraft, one private rotor wing aeromedical aircraft, and one fixed wing aeromedical aircraft, which combined to undertake fewer than 300 flights for trauma during 2010.
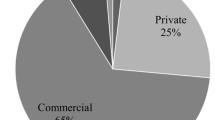
Regarding relative trauma volume by cause, overall violence-related trauma occupies 39.7 % of the workload (Fig. 5), while vehicular collisions are second, with 31.9 % of the trauma burden (Fig. 6). Other trauma, which includes burns, was the third cause overall at 28.4 % (Fig. 7). The predicted number of burn cases for the province is 7,099 per annum. The high rates of assault and gunshot injury relative to the overall trauma burden is of particular significance, along with the vehicle-related trauma, as these are potentially preventable injuries. This is especially concerning in light of the United Nations WHO Decade of Action 2011–2020 [11]. This was true for nine districts; however, two districts showed a different trauma spectrum, with the Amajuba and uThukela districts (both rural) having “other trauma” as the leading cause of injury, while the two private services had a much higher vehicular collision rate and much lower interpersonal violence rates (Table 2). This is expected because most of the private services are based in urban areas with higher ALS staff availability. The private services responded to 3.5 % of the overall number of calls reviewed, mostly in the eThekwini, uMgungundlovu and Ilembe districts.
Three districts had large numbers of “exempt” calls, those where the EMS response was made and the call was either a hoax or the patient had left the scene prior to EMS arrival. All three of those districts were largely rural in nature, and control center records show that less than 35 % of all calls in these rural regions were attended to in under 40 min (the national norm for rural responses) [12]. Overall, 6,609 unnecessary responses were recorded, where no patient was found or transported.
Regarding the severity of injury, the EMS use a four-part triage system with red implying life-threatening injury, yellow a stable stretcher case, and green walking wounded. Code blue indicates that the patient was dead on arrival. Injury classification had been recorded by the control centers for 13,133 cases (77.7 % of all calls received). The spread of injury severity across the province was as follows: 80.3 % of cases were coded “yellow”; 15.6 % were cases of severe trauma and were coded “red,” whereas only 3.7 % of the cases were coded “green” and a minority of 0.4 % were dead on arrival. This implies that 80 % of the patients should be treatable in appropriately equipped and staffed regional hospitals and that the majority of trauma victims should bypass small clinics and district hospitals. Only 15 % of cases will require care in a fully equipped level 1 trauma center, and there is only one such center in the province.
When examining definitive care destination, however, it was noted that almost 57 % of trauma cases were transferred to district hospitals, which have limited imaging and surgical facilities, whereas 40 % were taken to regional hospitals and 1 % to tertiary or quaternary hospitals, whereas only 0.42 % were taken to the private hospital sector facilities. A further 1.6 % of cases were inappropriately taken to community (nurse-run) clinics. Around 2.7 % of transfers required transfer out of the district, thus further reducing the limited numbers of ambulances available for emergency cases in these districts (Fig. 6). All code blue patients were transported to state forensic mortuaries, as SA law require a medico-legal post-mortem in these cases [13].
As part of the process of gauging the need for a trauma system in the prehospital phase of care, qualitative questionnaires were sent to 29 senior ambulance personnel (“Zonal Officers”) across the province, and the following recurring themes were noted: 83 % of respondents had knowledge of the free triage and mass casualty system training in the province and they indicated that over 460 staff had been trained. Despite this, 55 % felt there was no established system to bypass district hospitals effectively when injury severity clinically justifies such bypass. When appropriate, it was often left to the individual advance life support practitioner, incident commander, or hospital medical officer to recommend such bypass maneuvers. In fact, 18 of the officers responded that all patients are initially taken to the closest hospital or clinic, even when this is not the best facility for the patient, as this is what the current referral pathway dictated. A further five officers suggested the district hospital is appropriate only for minor and moderate injuries, and that major cases (code red) should be offered bypass to larger regional hospitals. Three officers said they never offer bypass as an option for their patients.
When asked which patients they would bypass, the responses were varied and included the following: 17 suggested only major cases, while one each stated cases of prolonged transfer distance and mass casualty situations, respectively. Four officers suggested bypass for those needing computed tomography (CT), surgery, or orthopedic intervention, as these specialties are available only at regional facilities. Only two respondents suggested that only helicopter cases qualified for service upgrade and bypass.
Finally, the officers were asked to comment on what they felt was necessary to improve the system once implemented. Seventeen suggested upgrading receiving hospitals at the district level. In particular they mentioned provision of adequate staff, training for the medical and nursing staff in trauma care, improvement of equipment (especially for ventilation), provision of imaging at all hospitals (CT scanner) to reduce transfers, and allowing EMS staff to directly discuss patients with regional center staff if the triage category suggested the need for a higher level of care. They also mentioned predesignation of trauma centers and increased access to aeromedical evacuation as priorities for improving outcome.
Discussion
South Africa is considered by many to be a mixed developed and developing country (Fig. 8 from World Bank data), with parts of the country comparable to well-resourced international cities and other parts comparable to very poorly resourced low to middle income countries. [14] The EMS in South Africa is far more developed and established than in most other parts of Africa, where reliance on passers-by and informally trained first-aiders is the norm and ambulances are few and far between [15, 16].
Trauma, as a relative disease-burden, has been examined both regionally [17] and nationally from various aspects, although the prehospital burden has largely been ignored, with the last large series reported in 1996 [18, 19]. Mostly these studies have focussed on mortality and not the live-patient cohort. Relative to other countries, South Africa has advanced training and fairly modern facilities for prehospital emergency care; however, much of this is located in the urban regions where the effectiveness of ALS has been questioned [20, 21]. Trauma also consumes much more of the health care budget and constitutes relatively more of the emergency workload relative to other developed countries [22]. The additional challenge to the EMS in South Africa is the high level of brain drain among the highest levels of emergency care providers [23, 24].
Despite these advantages and challenges, previous reviews have demonstrated that there is a semi-formal system of care in South Africa, which is split into a private sector and a public sector [12, 25, 26]. There is professional cooperation, with the private sector aiming to capture the insured section of the health care sector comprising <20 % of the population, with some mistrust between the two sectors evident [27]. This is coupled with a referral pathway largely based on a system relevant to primary medical healthcare conditions, such as maternal-child health, infectious or chronic disease. In addition, the system is burdened by numerous mass-casualty events [4, 28–32]. This leads to the inappropriate delivery of severely injured patients to inadequately equipped facilities, which were not designed for trauma care, necessitating subsequent transfer, often with delayed dispatch of ALS prehospital services, which are engaged in treating minor and moderate injury cases [28, 32]. These services are often already overwhelmed, as noted by the fact that only between 30 and 40 % of all emergency patients arrive at hospital in an ambulance [33]. Violence and motor vehicle incidents make up the lion’s share of the work, in a similar spectrum to that recorded previously, with no apparent reduction over time [34–36]. In keeping with this study, the previous Durban study showed that only about 15–20 % of cases comprise major trauma [28].
Previous local studies have shown that care at a major trauma center leads to less morbidity, mortality, and missed injury, especially for the more severely injured [37, 38]. Studies from other parts of Africa have demonstrated reduced morbidity and mortality through community participation and basic prehospital system development [39–41]. Similar studies from other parts of Africa have shown that the lack of EMS services lead to higher complication rates, longer prehospital times, and multiple transfers [41–44]. It is interesting to note from the present study that the EMS providers themselves determined this to be a challenge to optimal care and illustrates the blatant link to poorer outcomes. The need for a more formal all-encompassing trauma system is readily apparent. Most of the steps to achieve this will be fairly simple and cost-efficient, such as bypass to appropriate “first contact” facilities and upgrading the lower levels of hospital facility.
As far back as 1998, the Cape Town Summit, endorsed by the Trauma Society of South Africa, called for Emergency Medical Systems that took account of the world’s economic constraints and proposed that these require change in the delivery of health care in both the developing and developed world. The proposal they offered was a step-wise evolutionary system adaptable to many different practice environments [45, 46]. South Africa is now fairly advanced on the template proposed at the summit; however, the same is not true of many other African countries. The Cape Town model proposes beginning with self-care and prevention, progressing to access and intervention by trained providers, and completion of care in a properly staffed, equipped, and regionally credentialed hospital, such as facilities that meet the recently proposed local South African standards [46, 47].
To place this in perspective, it is interesting to compare the trauma prehospital event rate of 11.6 per 1,000 population to other local or international data. Regionally, the total ambulance call rate is listed in data on hand as 72/1,000 population, implying that trauma is approximately 15 % of the total ambulance workload in KZN. No other local data have been published looking at the prehospital trauma burden, while the reported hospital burden is around 40 per 1,000 [48]. This total includes all ambulance transports in the public sector, except planned outpatient transports. Comparatively, the rates are far in excess of those reported from developed countries, with Wales reporting a rate of 19 per 100,000 and Norway 30 per 100,000, while other developing countries also report much lower rates, with Pakistan varying between 9 and 23 per 100,000, depending on the underlying injury mechanism [49–52]. This begs the question of what prehospital trauma system will work in under-resourced countries. The World Health Organisation document for essential prehospital care suggests that the components of an efficient prehospital care system must include, at a minimum, prompt communication and activation of the system, the prompt response of the system, and the assessment, treatment, and transport of injured people to formal health-care facilities, regardless of whether they are urban or rural. This system may be constituted of one or more tiers of care, but it must have a lead organisation, appropriate cost-effective staffing of at least the basic level of EMS response, and disaster planning. Funding options and the need for political and legislative considerations are highlighted, similar to points highlighted recently in a South African publication. Additionally, the WHO and TSSA documents suggest that there is a need for medical oversight of the EMS service, regular audits, and quality assurance [22, 47, 53].
In the context of the present study, the system must optimize the number of ambulances per geographical region, determine and appropriately equip predetermined receiving facilities, and establish the option of bypassing limited resourced facilities. Putting more advanced emergency care practitioners in the rural areas would potentially reduce prehospital mortality. Additionally, the WHO document highlights the need for bypass to allow prehospital providers to take patients to the appropriate level of care [53].
Can this be done cost effectively in Africa? Recent studies have shown that trauma systems are cost-effective; however, these studies also show that it takes about 10 years to realize the cost benefits [54]. To ensure success in constructing more efficient systems, health departments need to demonstrate courage in putting the structure and processes in place, knowing that the ends must justify the means in Africa. The data presented in this study also show the need to redesign the system in South Africa to make it more inclusive and cost effective, with bypass as a simple initial stage in this process.
A logical system must include a single national number, with universal access from mobile and landline telephony, integration of private and public service providers into a coordinated control structure to ensure efficient resource utilization, using regionalized control centers with rapid access to other emergency services. Using the TSSA guidelines and the WHO Trauma System Evaluation tool will enable South Africa to reach at least a level 3 rating and aspire to level 4 [6, 47]. Predesignation of trauma facilities, both private and public, will ensure that patients reach the closest appropriate care facility rapidly. The funding for all emergency cases, especially trauma, should be from the central government, with universal payment to prevent a dichotomy of service provision, such as the planned National Health Insurance scheme proposed recently by the South African health ministry [22, 47, 48, 55].
The present study has some limitations, including the fact that it was undertaken in a single province in one of the more developed countries in Africa. Thus the generalizability of the results may not be high, although trauma is recognized across the continent as a major challenge. Additional limitations include reliance on recorded data interpreted secondhand from call-center records, which may lead to the possibility of underreporting of the trauma burden. In fact, approximately 5 % of all potential calls were excluded by the researchers due to lack of clarity of the underlying cause. It was known to the researchers that two of the districts provided incomplete data, thus the total trauma burden is at best an estimate of the minimum burden. This may have led to an underestimation of up to 5 % of the true trauma burden. Third, this study only included data from the two large nationally functioning private ambulance services, while there are numerous small private services in the province, probably providing care to as much as an additional 2 % of cases. Thus the true underestimate may be as high as 7 %, meaning that there would most likely be closer to 110,000 trauma calls to EMS per annum. In addition, it has been noted that a significant proportion of trauma cases present to definitive care via their own transport [34, 35, 56].
Conclusions
The burden of prehospital trauma in South Africa is significant and higher than in most developed countries; at about 18 % of the overall emergency burden of disease, however, this consumes vital resources and reduces the availability of ambulances, already at a premium, for other non-trauma emergency cases. The optimal system will deliver the patient with appropriate severity to the correct level of care, but will bypass non-doctor primary care services and inappropriately resourced district services for moderate and major severity cases. A system must be inclusive and incorporate all services from EMS to rehabilitation, rather than focusing on one or two super-specialized major trauma centers, which should be maintained as a regional lead resource.
References
The Epidemiology Unit, KZN Health. KwaZulu-Natal Epidemiology Bulletin no 6, March 2004. Department of Health, KZN, South Africa: 10–11
Department of Health Population estimates. www.kznhealth.gov.za. Accessed 24 March 2012
Hardcastle TC, Balfour C, Wallis LA et al (2006) The training of emergency care personnel in South Africa: from prehospital to emergency department to the operating room. Arch Ibadan Med 7:92–94
Goosen J, Bowley DM, Degiannis E et al (2003) Trauma care systems in South Africa. Injury 34:704–708
Naidoo R (2011) Emergency care in Africa. Afr J Emerg Med 1:51–52
Trauma system maturity tool. World Health Organisation. www.who.int/. Accessed 24 March 2012
Butchart A, Peden M, Matzopoulos R et al (2001) The South African national non-natural mortality surveillance system rationale, pilot results and evaluation. S Afr Med J 91:408–417
Van der Spuy JW, De Wet B (1991) Trauma—today and tomorrow. S Afr Med J 79:61–62
Vella V, Govender T (2006) Burden of mortality in KwaZulu-Natal. KwaZulu-Natal Epidemiol Bull no 14, Department of Health, KZN, December:5–13
Fortesque A (2010) GIS: mapping disasters. Emergency services SA, August:8
World Health Organization (2009) Global status report on road safety: Time for action. Geneva, World Health Organization. www.who.int/violence_injury_prevention/road_safety_status/2009. Accessed 20 September 2010
MacFarlane C, Van Loggerenberg C, Kloek W (2005) International EMS systems: past present and future. Resuscitation 64:145–148
Hardcastle T (2012) Medico-legal aspects of operative nursing—what is new? SATS 37:12–14
Brysiewicz P (2001) Trauma in South Africa. Int J Trauma Nurs 7:29–32
Wachira B, Martin IBK (2011) The state of emergency care in the Republic of Kenya. Afr J Emerg Med 1:160–165
Geduld H, Wallis LA (2011) Taxi driver training in Madagascar: the first step in developing a functional prehospital emergency care system. Emerg Med J 28:794–796
Garrip A, Herbst AJ, Hosegood V et al (2011) Injury mortality in rural South Africa: 2000–2007: rates and associated factors. Trop Med Internat Health 16:439–446
Norman R, Matzopoulos R, Groenewald P et al (2007) The high burden of injuries in South Africa. Bull WHO 85:695–702
Van der Spuy J, Steenkamp M (1996) Ambulance transport of trauma victims: a metropolitan profile. Trauma Emerg Med 13:9–12
Smith WP, Hardcastle TC, Robertson CC (2006) Prehospital emergency medical services in South Africa. Arch Ibadan Med 7:85–87
Eckstein M, Chan L, Schnier A et al (2000) Effect of prehospital advanced life support on outcomes of major trauma patients. J Trauma 48:643–648
Hardcastle TC (2011) The 11P’s of an Afrocentric trauma system for South Africa: a time for action. S Afr Med J 101:160–162
Hackland S, Stein C (2011) Factors influencing the departure of South African advanced life support paramedics from prehospital operational practice. Afr J Emerg Med 1:62–68
Whittaker R (2011) Safety First. Bull HPCSA :36–37
Macfarlane C, Benn CA (2003) Evaluation of emergency medical services systems: a classification to assist in determination of indicators. Emerg Med J 20:188–191
Toubkin M (2010) Emergency medicine—private sector trends. Emergency services SA/occupational risk April:13–14
Bateman C (2005) Saving lives: who picks up the tab? S Afr Med J 95:545–550
Owen R, Dimopoulos GE (1994) An analysis of advanced life support in the greater Durban area. Trauma Emerg Med (SA) May/June:1053–1057
Robertson C (1998) Report on the Nuwekloof train accident near Tulbach in the Western Cape on 23 April 1997. Trauma Emerg Med (SA) Feb/Mar:15–17
Boyd ST, Dimopoulos GE (1998) The Marianhill train accident. Trauma Emerg Med (SA) Feb/Mar:27–29
Brysiewicz P, Bruce J (2008) Emergency nursing in South Africa. Int Emerg Nurs 16:127–131
Slabbert JA, Smith WP (2011) Patient transport from rural to tertiary health centres in the Western Cape: is there room for improvement. Afr J Emerg Med 1:11–16
Van der Spuy J (1995) Prehospital trauma care. Trauma Rev 7:4–5
Strydom M (1998) Ambulance transport of trauma cases in the Cape Metropole. Trauma Rev 3:6–8
Peden M, Abrahams N (1994) From urban to rural trauma. Trauma Rev 2:1–3
Meumann C, Peden M (1997) Trauma in Durban. Trauma Rev 5:3–5
Cheddie S, Muckart DJJ, Hardcastle TC et al (2011) Direct admission versus transfer to a level 1 trauma unit improves survival. S Afr Med J 101:176–178
Steinwall D, Befrits F, Naidoo SR et al (2012) Deaths at a level 1 trauma unit: a clinical finding and post-mortem correlation study. Injury 43:91–95
Mock C (2009) Strengthening prehospital trauma care in the absence of formal emergency medical services. World J Surg 33:2510–2511. doi:10.1007/s00268-009-0239-4
Jayaraman S, Mabweijano JR, Lipnick MS et al (2009) Current patterns of prehospital trauma care in Kampala, Uganda, and the feasibility of a lay-first-responder training program. World J Surg 33:2512–2521. doi:10.1007/s00268-009-0180-6
Olayinka SA, Ayokunle O, Mustapha AF (2012) Prehospital transport of spinal cord injured patients in Nigeria. S Afr J Surg 50:3–5
Forjouh SN, Mock CN, Friedman DI et al (1999) Transport of the injured to hospital in Ghana. Accid Anal Prev 3:66–70
Solagberu BA, Kuranga SA, Adekanye AO et al (2003) Preventable trauma deaths in a country without emergency medical services. Afr J Trauma 1:39–44
Trunkey DD (2008) The medical world is flat too. World J Surg 32:1583–1604. doi:10.1007/s00268-008-9522-z
Turner J, Judge TP, Ward ME et al (2000) A new worldwide systems model for emergency medical services: statement from the Cape Town EMS summit, South Africa, January 1998. Pre-hospital Immediate Care 4:183–188
Ward ME, Judge TP, Johns BM et al (2000) Improving the odds: towards a new understanding of emergency medical care. Pre-hospital Immediate Care 4:189–191
Hardcastle T, Steyn E, Boffard K et al (2011) Guideline for the assessment of trauma centres for South Africa. S Afr Med J 101:189–194
Matzopoulos RG, Prinsloo M, Butchart A et al (2006) Estimating the South African trauma load. Int J Inj Contr Saf Promoton 13:49–51
Gorman DF, Teanby DN, Sinha MP et al (1995) The epidemiology of major injuries in Mersey and North Wales. Injury 26:51–54
Hansen KS, Morild I, Engesaeter LB et al (2004) Epidemiology of severely and fatally injured patients in the Western part of Norway. Scand J Surg 93:198–203
Chotani HA, Razak JA, Luby SP (2002) Patterns of violence in Karachi, Pakistan. Inj Prev 8:57–59
Gaffar A, Hyder AA, Mastor MI et al (1999) Injuries in Pakistan: directions for future health policy. Health Policy Planning 14:11–17
Sasser S, Varghese M, Kellermann A et al (2005) Prehospital trauma care systems. World Health Organization, Geneva
Moore L, Hanley JA, Turgeon AF et al (2010) Evaluation of the long-term trend in mortality from injury in a mature inclusive trauma system. World J Surg 34:2069–2075. doi:10.1007/s00268-010-0588-z
National Department of Health (South Africa) (2011) National Health Insurance, policy paper issued 12 August, Cape Town, Government Printer
Demetriades D, Chan L, Cornwell E et al (1996) Paramedic versus private transportation of trauma patients. Arch Surg 131:133–138
Acknowledgments
The authors are grateful to Mr. Sithole, General Manager of EMRS; Robyn Holgate of ER24; and the Netcare EMS senior management for permission to use their data.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article forms part of a series of studies toward a PhD in Trauma Systems for the lead author.
Rights and permissions
About this article
Cite this article
Hardcastle, T.C., Finlayson, M., van Heerden, M. et al. The Prehospital Burden of Disease due to Trauma in KwaZulu-Natal: The Need for Afrocentric Trauma Systems. World J Surg 37, 1513–1525 (2013). https://doi.org/10.1007/s00268-012-1852-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-012-1852-1