Abstract
Background
Distinguishing between unilateral and bilateral adrenal lesions is mandatory for surgical treatment of primary aldosteronism (PA). Adrenal venous sampling (AVS) is considered the gold standard for identification and localization of the lesion or lesions causing PA. The objective of the present study was to determine the usefulness of AVS in PA patients.
Patients and methods
From January 2001 to October 2011, 86 patients with the biochemical diagnosis of PA were retrospectively analyzed. The study group included 45 males and 41 females with a mean age of 50.7 ± 12.6 years, and all patients underwent adrenal computed tomography (CT) and AVS.
Results
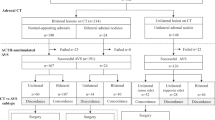
The catheterization success rate of AVS was 82.69 % (86/104). In addition, AVS revealed bilateral lesions in 15/75 patients with unilateral abnormalities diagnosed by CT. These patients underwent medical treatment instead of surgery. One patient had an adrenal mass on the right side, but AVS localized the lesion on the left side. This patient underwent left adrenalectomy. Furthermore, AVS revealed a unilateral lesion in 2/5 patients with bilateral abnormalities demonstrated by CT. These patients underwent unilateral adrenalectomy. Finally, AVS demonstrated localization in 1/6 of patients with no CT abnormalities who were subjected to surgery. Fifty-three patients with unilateral lesion and one patient with bilateral hypersecretion underwent surgical removal of the affected gland(s). All patients had resolution of hypokalemia and clinical improvement of hypertension.
Conclusions
Many patients (19/86, or 22.09 %) would have been inappropriately managed if decision making had been based solely on CT findings. Therefore, AVS is recommended before determining definitive PA management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Primary aldosteronism (PA) is a rare endocrine disease with a prevalence of 0.5–2.0 % in hypertensive patients [1]. In recent years, regardless of clinical symptoms stemming from hypertension or hypokalemia, patients are generally diagnosed with PA by biochemical screening, and PA is even discovered incidentally in normokalemic patients [2]. Because PA is a common cause of correctable secondary hypertension, diagnosis of the disease is extremely important, especially in patients with uncontrollable hypertension resulting from PA.
Proper diagnosis of PA is crucial for the appropriate management of patients and for improvement of their survival outcomes, lowering the cardiovascular risk and preventing fetal complications [3–6]. Treatment options, including surgery and mineralocorticoid receptor antagonist-based pharmaceutical therapy, are selected based on the location of the lesion. Therefore, imaging and biochemical laboratory techniques [e.g., computed tomography (CT), magnetic resonance imaging (MRI), and adrenal venous sampling (AVS)] are currently in wide use as standard examinations for patients with suspected or confirmed PA [7, 8].
Especially AVS has been reported as the gold standard for the localization of the lesion(s) responsible for PA [9–11]. Young et al. reported that unilateral abnormality on CT revealed the isolated contralateral lesion on AVS, and AVS revealed the localization of the lesion in the patient(s) who had bilateral adrenal nodules [12]. The aim of the present study was to investigate the value of AVS as a diagnostic option for patients with PA.
Patients and methods
Study design and patients
From January 2001 to October 2011, 104 patients with PA that was identified by screening with the PAC to PRA ratio were found retrospectively. Computed tomography and AVS were performed simultaneously in these patients to localize the lesions. All diagnostic tests were performed at a single institution, the Seoul National University Hospital. Institutional Review Board approval was obtained for this retrospective study, and informed consent was obtained for all studies and procedures.
Among the 104 patients, one was excluded due to technical failure in the cannulation of the right adrenal vein resulting from the acute angle of entry of the catheter. Seventeen additional patients were excluded as a result of biochemical failure, i.e., dilution of the samples. Therefore, the catheterization success rate of AVS was 82.69 % (86 of 104 patients). The clinical data from these 86 patients (45 males and 41 females with a mean age of 50.7 ± 12.6 years) were retrospectively analyzed from the patients’ electronic medical records.
At the initial diagnosis of PA, 97.7 % of the patients (84 of 86) presented with hypertension, and 74.4 % of the patients (64 of 86) had hypokalemia. Hypertension was defined when a patient’s systolic blood pressure was more than 140 mmHg or when the diastolic blood pressure was more than 90 mmHg, according to the Seventh Report of the Joint National Committee. The mean serum potassium level for the 86 patients was 3.1 mmol/L [range: 1.9–4.4 mmol/L; standard deviation (SD): 0.5].
Both PRA and PAC were measured in 85 of 86 patients. If the PAC/PRA ratio was greater than 30, PA was suspected, and further investigations were performed to localize the lesion [13, 14]. The mean PAC was 349.5 ng/dL (range: 11.9–1,880 ng/dL; SD: 305.2), and the PAC/PRA ratio ranged from 81 to 18,800. Sixty-six percent of the patients (57 of 86) underwent saline loading tests. After infusion of 2 L of saline for 4 h, all patients had an unsuppressed PAC above 10 ng/mL [15]. The mean PAC after the saline loading test was 297.6 ng/dL (range: 7.2–1,640 ng/dL, SD: 316.5) (Table 1). A total of 54 patients underwent surgical treatments; clinical characteristics, a description of the surgical treatment, and the type of pathology are shown in Table 2.
CT imaging
Computed tomography images with a slice thickness of 5 mm were obtained using 4-channel (MX 8000, Philips Medical Systems, Cleveland, OH), 16-channel (Sensation 16, Siemens, Erlangen, Germany), or 64-channel (Brilliance 64, Philips Medical Systems) CT scanners. Forty-five seconds after infusion of the contrast medium, arterial phase images were obtained. Delayed phase images were obtained at 3–15 min after acquisition of the arterial phase images. An adrenal mass was diagnosed when washout of contrast medium was observed in the delayed phase at 15 min after the arterial phase.
Adrenal venous sampling
Computed tomography as a method to assess lesion localization can lead to selection of an inappropriate treatment option due to its high frequency of false positive and false negative results [16]. Therefore, in the present study, all patients underwent AVS and CT simultaneously. Infusion of cosyntropin (Synacthen, 50 μg/h), a synthetic derivative of adrenocorticotropic hormone, was initiated 30 min prior to the procedure. Blood samples were obtained from the bilateral adrenal veins and the inferior vena cava (IVC) for cortisol and aldosterone measurements. Successful AVS (i.e., correct identification of unilateral versus bilateral lesions) was determined by at least a threefold elevation in adrenal vein cortisol levels compared with IVC cortisol levels [9, 17–19].
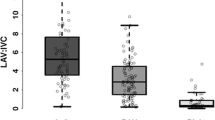
Localization criteria were defined as follows: (1) the aldosterone/cortisol (A/C) ratio of the dominant adrenal vein (i.e., on the side of the lesion) was more than four times the A/C ratio of the non-dominant adrenal vein, and (2) the A/C ratio of the non-dominant adrenal vein was less than that of the IVC.
Statistical analysis
All values are given as the mean ± SD. The results were subjected to statistical analyses performed with SPSS Statistics (version 19, SPSS Inc., Chicago, IL) to ascertain means.
Results
Eighty-seven percent of the patients (75 of 86) presented with unilateral adrenal abnormalities on CT scans, and 5.8 % of the patients (5 of 86) presented with bilateral CT abnormalities. The remaining six patients had no abnormal CT findings in either adrenal gland.
Among the 75 patients who presented with unilateral CT abnormalities, 60 individuals (80 %) also presented with unilateral AVS lesions, and 50 of these patients underwent unilateral adrenalectomy. However, adrenalectomy was not performed in 10 patients with unilateral CT abnormalities and concordant AVS results. Three of these patients refused the operation, and the follow-up of one patient was lost due to the patient’s noncompliance. Three patients were still waiting for the operation at the time of study write-up. Among the remaining three patients, one underwent AVS while taking an aldosterone receptor blocker and a β-blocker. Pharmaceutical therapy with these oral anti-hypertensive medications could not be terminated because the patient was afflicted with severe heart failure; therefore, the endocrinologist decided to continue a mineralocorticoid receptor antagonist in the patient’s drug arsenal, and to follow-up with the patient after a short-term interval. An additional patient previously underwent a left nephrectomy and adrenalectomy due to advanced renal cell carcinoma, and the adrenal lesion was located in the right adrenal gland. In this case, the endocrinologist decided to maintain medical therapy in order to avoid adrenal insufficiency. The final patient presented with a discordant result in regard to the side of the lesion. The CT results indicated that the lesion was located on the right side, whereas AVS localization indicated that the lesion was located on the left side. The endocrinologist again decided to maintain medical therapy, and to follow up with the patient after a short-term interval.
Fifteen patients with CT results of unilateral abnormalities had AVS results of bilateral lesions. Medical therapy was applied for these patients instead of surgical intervention.
In 5 of 86 patients (5.81 %), CT scans revealed bilateral abnormalities, and AVS results indicated bilateral lesions in three of these patients, corresponding to the CT findings. Among these three patients, one underwent bilateral subtotal adrenalectomy, because bilateral hypersecretion was strongly suspected. Histology revealed that this patient had bilateral adrenal cortical adenoma postoperatively. The AVS revealed unilateral lesions for the remaining two patients, and unilateral adrenalectomy was performed.
The AVS study demonstrated that one of the six patients with no CT abnormalities in fact had a unilateral lesion, and that the remaining five patients had bilateral hyperplasia. The one patient with a unilateral lesion revealed by AVS underwent unilateral adrenalectomy.
Therefore, the results of the present retrospective analysis show that 22.09 % of the patients (19 of 86) would have been inappropriately managed based on CT findings alone (Fig. 1).
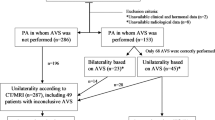
In the 75 patients who presented with a unilateral adrenal mass and a normal contralateral adrenal gland on CT scans, further analysis was performed according to the size of the lesion, the patient’s age, and the AVS results. Fifty-nine patients had adrenal masses larger than 1 cm in diameter, and the others (16 of 75) had adrenal masses smaller than 1 cm in diameter.
Six of the 16 patients with adrenal masses smaller than 1 cm were younger than 40 years of age at the time of diagnosis and had concordant CT and AVS results. The other 10 patients were older than 40 years of age. The CT scans and AVS showed concordant results for 6 of these 10 patients and discordant results for the remaining 4 patients.
In the 59 patients with adrenal masses larger than 1 cm, 9 patients were younger than 40 years of age at the time of diagnosis, and 50 patients were older than 40 years old of age. The AVS results showed bilateral lesions for 9 of the 50 patients who were older than 40 years of age. These results were discordant with the CT results, and the patients did not require surgical therapy. The AVS and CT results were congruent for the remaining 41 patients older than 40 years. In addition, AVS indicated bilateral lesions for 2 of the 9 patients who were younger than 40 years of age, whereas the AVS and CT results were in agreement for the other 7 patients in this age group.
A total of 53 patients underwent unilateral adrenalectomy according to the results of lesion localization revealed by AVS. An additional patient underwent bilateral adrenalectomy according to the AVS result of bilateral hypersecretion. Among these 54 patients, hypertension was cured in 88.9 % of the patients (48 of 54) and improved in 11.1 % of the patients (6 of 54) during postoperative clinical follow-up. Additionally, 98.1 % of the patients (53 of 54) showed postoperative normalization of hypokalemia. One patient could not be evaluated for postoperative potassium levels because of loss to follow-up in the outpatient department. The mean postoperative potassium level among the other 53 patients was 4.03 mmol/L (range: 2.8–5.7 mmol/L, SD: 0.5 mmol/L), and the median follow-up period was 523 days (range: 11–2,586 days).
Discussion
The aim of the present study was to determine the value of AVS as a diagnostic tool to aid in choosing an appropriate treatment option for patients with PA. The treatment option is determined according to the localization of the lesion, and thus diagnostic tests for localization are of utmost importance. The present retrospective analysis of 86 PA patients contributes to our understanding of CT inaccuracy in the assessment of lesion localization, which can consequently have a negative impact on PA management. Adrenalectomy of the affected gland should be offered to patients with unilateral PA, whereas patients with a bilateral source of excess aldosterone secretion should undergo pharmaceutical therapy, including treatment with mineralocorticoid receptor antagonists [20].
In contrast to CT, several studies report the reliability of AVS as a test for localization in patients with PA. Zarnegar et al. report that AVS should be used whenever CT findings are equivocal, or when both adrenal glands are abnormal [21]. Schwab et al. further report that, in their clinical experience, AVS is the superior test when compared with CT for subtype identification of PA, as well as for determination of occult hypersecretion from the adrenal gland [19]. Moreover, recent studies indicate that AVS should be performed routinely rather than selectively in patients with PA. Mathur et al. [22] stated that 50 % of PA patients would have been inappropriately managed based on CT findings alone, and therefore, patients with biochemical evidence of PA who are considering adrenalectomy should first undergo AVS. Additionally, Ishidoya et al. report that because nearly one-fourth of patients with unilateral PA had a negative CT finding, routine AVS should be performed in patients with unilateral adrenal aldosterone hypersecretion [23]. In light of these previous studies, the present study retrospectively analyzed PA patients who underwent simultaneous AVS and CT so as to evaluate the concordance and discordance between the AVS and CT results.
It must be emphasized that AVS is a difficult procedure to perform in the clinical setting, and that considerable expertise is required in the interpretation of AVS results. In fact, Kline et al. declared that AVS may not always be the so-called gold standard for diagnosing PA due to different systems for the interpretation of results [24]. Moreover, the invasiveness and technical complexity of the procedure have created a situation in which many clinicians will only implement AVS in certain PA patients, and if anatomical variations in the adrenal vein are present, such as the unusual variant of left adrenal venous drainage directly into the IVC, the AVS procedure becomes even more arduous [25, 26].
The known major complications of AVS include adrenal vein rupture and subsequent intraglandular and widespread periadrenal hemorrhage, adrenal infarction, and adrenal vein thrombosis [27]. Based on their considerable multicenter clinical experience, Vonend et al. [28] recommend that (1) AVS interpretation should be limited to a few select radiologists so as to increase their expertise; (2) written standard operating AVS procedures should be in place; (3) a rapid cortisol assay should be performed immediately following initiation of the AVS procedure; and (4) prompt feedback should be offered to technical personnel in order to accelerate the learning curve and to overcome the invasiveness of the procedure. In the present study, there were three cases of adrenal vein injury and subsequent small hematoma. Although all three patients recovered without any additional treatment, careful monitoring of vital signs was applied in all cases.
The present study documented that 22.09 % (19/86) of the patients would have been inappropriately managed if the treatment decision had been based solely on CT findings. Two patients who had bilateral abnormalities on CT scans were shown to have unilateral lesion localization following AVS; these patients came close to medical treatment instead of surgery. Additionally, 15 patients who had unilateral abnormalities on CT scans but bilateral abnormalities following AVS, almost underwent surgery instead of medical treatment. One patient who had no abnormality on CT were shown to have a unilateral lesion revealed by AVS: this patient also came close to medical treatment instead of surgery. Finally, one patient with a right side abnormality on CT revealed localization to the left side following AVS. This patient underwent left adrenalectomy. Not only is adrenalectomy an irreversible event, but it is also inappropriate with respect to the patient’s clinical outcome in the case of bilateral disease.
According to the exacting approach for lesion lateralization adopted by the current analysis, adrenalectomy was performed on 53 patients with unilateral PA and one patient with bilateral adrenal adenoma revealed by AVS. All of the patients who underwent surgical treatment were either cured or demonstrated improvement in their hypertensive status. Furthermore, abnormal potassium levels were normalized during the postoperative period.
Some clinicians recommend that AVS should be reserved for a subset of patients for whom CT findings are equivocal, both adrenal veins are abnormal, or preoperative imaging studies cannot definitively lateralize the lesion [21, 25]. In addition, some clinicians recommend that when the patient is younger than 40 years old, has a normal contralateral adrenal gland, and presents with an adrenal adenoma larger than 1 cm in diameter, no further imaging or evaluation is needed, and the patient should be referred for surgical treatment [16]. However, according to our analysis, AVS showed evidence of bilateral abnormalities in two patients younger than 40 years who had an adrenal mass larger than 1 cm. These AVS results were discordant with the CT results, which showed a unilateral adrenal mass. This suggests that AVS should be performed in all patients with PA planning to undergo adrenalectomy, regardless of the CT results.
Of course, this study is not without limitations. First, these results were deduced from a retrospective analysis of clinical data, and therefore, this study was not a double-blinded, prospective study. Second, selection bias existed in the current analysis, and this non-randomized study also included a relatively small number of patients. A future analysis involving a large number of subjects is required to secure the justification for performing AVS in all PA patients considering adrenalectomy. Third, the success rate of AVS in this series was relatively low (82.69 %). However, before September 2006, the success rate was only 54.54 % (12 of 22 patients analyzed). An interim analysis of AVS data was next performed at our institution (Seoul National University Hospital), and an active discussion for improving the success rate of AVS was initiated among endocrinologists, radiologists, and endocrine surgeons. As a result of these discussions and the use of a relatively strict definition of AVS localization criteria, the success rate climbed to 90.24 % (74 of 82 patients) between October 2006 and October 2011. Thus, we found that the success rate of AVS could be improved by using a multidisciplinary approach.
In conclusion, the results of the current analysis suggest that patients with PA who are considering adrenalectomy would benefit from undergoing AVS preoperatively. The present data indicate that AVS will allow the medical team to obtain the correct localization of the lesion, preventing inappropriate treatment. However, to establish AVS as a standard preoperative protocol, additional multicenter clinical experience should be collected and analyzed.
References
Quinkler M, Lepenies J, Diederich S et al (2002) Primary hyperaldosteronism. Exp Clin Endocrinol Diabetes 110:263–271
Bernini G, Moretti A, Argenio G et al (2002) Primary aldosteronism in normokalemic patients with adrenal incidentalomas. Eur J Endocrinol 146:523–529
Acelajado MC, Calhoun DA (2011) Aldosteronism and resistant hypertension. Int J Hypertens 20: article 837817
Milliez P, Girerd X, Plouin PF et al (2005) Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol 45:1243–1248
Delgado Y, Quesada E, Perez Arzola M et al (2006) Ventricular fibrillation as the first manifestation of primary hyperaldosteronism. Bol Asoc Med P R 98:258–262
Bryer A, Miller JL (1982) Conn’s syndrome presenting as a subarachnoid haemorrhage. A case report. S Afr Med J 62:249–250
Failor RA, Capell PT (2003) Hyperaldosteronism and pheochromocytoma: new tricks and tests. Prim Care 30:801–820, viii
Kempers MJ, Lenders JW, van Outheusden L et al (2009) Systematic review: diagnostic procedures to differentiate unilateral from bilateral adrenal abnormality in primary aldosteronism. Ann Intern Med 151:329–337
Nwariaku FE, Miller BS, Auchus R et al (2006) Primary hyperaldosteronism: effect of adrenal vein sampling on surgical outcome. Arch Surg 141:497–502 discussion 502–493
Funder JW, Carey RM, Fardella C et al (2008) Case detection, diagnosis, and treatment of patients with primary aldosteronism: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 93:3266–3281
Harper R, Ferrett CG, McKnight JA et al (1999) Accuracy of CT scanning and adrenal vein sampling in the pre-operative localization of aldosterone-secreting adrenal adenomas. QJM 92:643–650
Young WF, Stanson AW, Thompson GB et al (2004) Role for adrenal venous sampling in primary aldosteronism. Surgery 136:1227–1235
Blumenfeld JD, Sealey JE, Schlussel Y et al (1994) Diagnosis and treatment of primary hyperaldosteronism. Ann Intern Med 121:877–885
Mattsson C, Young WF Jr (2006) Primary aldosteronism: diagnostic and treatment strategies. Nat Clin Pract Nephrol 2:198–208 (quiz, 191 p following 230)
Rossi GP, Belfiore A, Bernini G et al (2007) Prospective evaluation of the saline infusion test for excluding primary aldosteronism due to aldosterone-producing adenoma. J Hypertens 25:1433–1442
Zeiger MA, Thompson GB, Duh QY et al (2009) The American Association of Clinical Endocrinologists and American Association of Endocrine Surgeons medical guidelines for the management of adrenal incidentalomas. Endocr Pract 15(Suppl 1):1–20
Magill SB, Raff H, Shaker JL et al (2001) Comparison of adrenal vein sampling and computed tomography in the differentiation of primary aldosteronism. J Clin Endocrinol Metab 86:1066–1071
White ML, Gauger PG, Doherty GM et al (2008) The role of radiologic studies in the evaluation and management of primary hyperaldosteronism. Surgery 144:926–933 (discussion 933)
Schwab CW 2nd, Vingan H, Fabrizio MD (2008) Usefulness of adrenal vein sampling in the evaluation of aldosteronism. J Endourol 22:1247–1250
Aloia JF, Beutow G (1974) Malignant hypertension with aldosteronoma producing adenoma. Am J Med Sci 268:241–245
Zarnegar R, Bloom AI, Lee J et al (2008) Is adrenal venous sampling necessary in all patients with hyperaldosteronism before adrenalectomy? J Vasc Interv Radiol 19:66–71
Mathur A, Kemp CD, Dutta U et al (2010) Consequences of adrenal venous sampling in primary hyperaldosteronism and predictors of unilateral adrenal disease. J Am Coll Surg 211:384–390
Ishidoya S, Kaiho Y, Ito A et al (2011) Single-center outcome of laparoscopic unilateral adrenalectomy for patients with primary aldosteronism: lateralizing disease using results of adrenal venous sampling. Urology 78:68–73
Kline GA, Harvey A, Jones C et al (2008) Adrenal vein sampling may not be a gold-standard diagnostic test in primary aldosteronism: final diagnosis depends upon which interpretation rule is used. Variable interpretation of adrenal vein sampling. Int Urol Nephrol 40:1035–1043
Tan YY, Ogilvie JB, Triponez F et al (2006) Selective use of adrenal venous sampling in the lateralization of aldosterone-producing adenomas. World J Surg 30:879–885. doi:10.1007/s00268-005-0622-8 (discussion 886–877)
Stack SP, Rosch J, Cook DM et al (2001) Anomalous left adrenal venous drainage directly into the inferior vena cava. J Vasc Interv Radiol 12:385–387
Daunt N (2005) Adrenal vein sampling: how to make it quick, easy, and successful. Radiographics 25(Suppl 1):S143–S158
Vonend O, Ockenfels N, Gao X et al (2011) Adrenal venous sampling: evaluation of the German Conn’s Registry. Hypertension 57:990–995
Conflict of interest
The authors have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oh, E.M., Lee, K.E., Yoon, K. et al. Value of Adrenal Venous Sampling for Lesion Localization in Primary Aldosteronism. World J Surg 36, 2522–2527 (2012). https://doi.org/10.1007/s00268-012-1695-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-012-1695-9