Abstract
Background
Randomized studies have indicated that acute appendicitis may be treated by antibiotics without the need of surgery. However, concerns have been raised about selection bias of patients in such studies. Therefore, the present study was aimed to validate previous findings in randomized studies by a full-scale population-based application.
Methods
All patients with acute appendicitis at Sahlgrenska University Hospital (May 2009 and February 2010) were offered intravenous piperacillin plus tazobactam according to our previous experience, followed by 9 days out-hospital oral ciprofloxacin plus metronidazole. Endpoints were treatment efficacy and complications. Efficient antibiotic treatment was defined as recovery without the need of surgery beyond 1 year of follow-up.
Results
A total of 558 consecutive patients were hospitalized and treated due to acute appendicitis. Seventy-nine percent (n = 442) received antibiotics as first-line therapy and 20 % (n = 111) had primary surgery as the second-line therapy. Seventy-seven percent of patients on primary antibiotics recovered while 23 % (n = 100) had subsequent appendectomy due to failed initial treatment on antibiotics. Thirty-eight patients (11 %) of the 342 had experienced recurrent appendicitis at 1-year follow-up. Primary antibiotic treatment had fewer complications compared to primary surgery.
Conclusions
This population-based study confirms previous results of randomized studies. Antibiotic treatment can be offered as the first-line therapy to a majority of unselected patients with acute appendicitis without medical drawbacks other than the unknown risk for long-term relapse, which must be weighed against the unpredicted but well-known risk for serious major complications following surgical intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute appendicitis is a most common surgical disorder and is still a clinical challenge [1, 2]. Appendectomy as treatment was introduced around 1880 and became standard therapy during the 20th century. However, interest in antibiotic therapy as a possible primary treatment increased during the last decade [3–6], although this is not a novel thought [7]. Four randomized controlled trials comparing antibiotics with appendectomy in adults with acute appendicitis have been published [8–11]. Three of these studies show similar results, with initial recovery for 88–95 % of patients treated with antibiotics [8–10]. The recurrence rate in our previous study on unselected adult patients appeared to be 10–15 % after 1 year in patients treated by antibiotics, with fewer major complications such as abscess formations, reoperations, and small bowel obstructions.
However, promising results from randomized trials do not automatically predict reproducible outcome in everyday clinical praxis. The first randomized study invited only men between 18 and 50 years old, with only around 20 % of eligible patients included [8]. This indicates low external validity and low generalizability. Other studies, included both sexes but did not report the number of excluded patients [10, 11]. In our own study, based on unselected men and women, the randomization procedure allowed surgeons on charge to violate the intention-to-treat allocation, which may create bias, although all eligible patients were included in the final analyses [9]. Thus, cited randomized studies and several retrospective reports indicate that antibiotic therapy is safe and may represent an effective first-line treatment of acute appendicitis, although with unknown long-term risk of recurrence or other complications [12–15]. The aim of the present study was therefore to investigate the extent to which results from randomized trials are valid in everyday clinical practice, i.e., to offer antibiotic therapy for acute appendicitis as the first-line therapy option to all patients with presumed acute appendicitis based on clinical evidence.
Materials and methods
This prospective nonrandomized population-based study was performed in the surgical clinics of Sahlgrenska University Hospital/Sahlgrenska and Sahlgrenska University Hospital/Östra, the two main hospitals in Gothenburg, Sweden. The study population consisted of all consecutive adult patients (>16 years old) with acute appendicitis according to our established clinical practice, where radiological CT examinations and ultrasound are used only when the diagnosis appears uncertain [16, 17]. Thus, acute appendicitis was based on several variables, including anamnesis, abdominal status, laboratory tests, and radiological examinations, only in doubtful cases to reduce hospital costs and unnecessary radiation as recommended [18]. The size of the population served by Sahlgrenska University Hospital is around 575,000–600,000 individuals with an estimated incidence of appendicitis around 0.10–0.12 %, which is in line with various figures for Sweden during 2009 according to database information provided by a Swedish medical authority (Socialstyrelsen) as well as compared to estimates of our population before our previous and present studies. Also, our prestudy values indicated that around 18 % of patients with acute appendicitis in the Gothenburg area displayed perforation and around 82 %had nonperforated appendicitis at operation (see Table 6 in [9]). No patients from our population area were treated outside the present protocol as confirmed by follow-up investigations in all our available databases.
Interventions
Our recommendation was to offer antibiotic therapy as the first choice for treatment to all patients judged to have acute appendicitis. However, the surgeon in charge could decide to operate when deemed necessary based on objective and subjective clinical reasons or when the patient insisted on primary surgery according to our ethical permission. Failing antibiotic treatment, judged clinically as progression of abdominal status, increasing body temperature, and lack of overall improvement within 12–24 h, allowed subsequent appendectomy. Those who were pregnant or who had recurrent appendicitis following previous randomized treatment with antibiotics [9] were offered primary surgery. All patients on first-line antibiotics received intravenous antibiotics (piperacillin plus tazobactam 4 g every 8 h) for at least three doses usually within 24 h according to our previous experience [9]. During this time the patients were not allowed oral intake but received intravenous fluids. Patients with improved clinical status the next day (12–24 h) were discharged from the hospital with oral antibiotics (ciprofloxacin 500 mg and metronidazole 400 mg twice a day) for an additional 9 days [9]. Seventy surgeons performed all operations according to the emergency staff organization in our hospital.
Data collection and follow-up
Pre-, peri-, and post-treatment data were recorded according to protocol. The surgeons were always obliged to grade abdominal status at diagnosis and also state the reason for surgery when deemed necessary [9]. Questionnaires, including questions on remaining symptoms and abdominal pain, experienced additional hospitalization, and any kind of operation or relevant medical treatment, were sent to all patients after 6 and 12 months. Medical hospital data files for each patient were searched at a minimum of 1 year after treatment and complications, recurrences, and reoperations were registered.
Outcome measures
Primary endpoints were treatment efficacy and major complications. Efficient antibiotic treatment was defined as recovery without the need for surgery for the primary hospital stay and the 1-year follow-up should be without recurrence. Surgical treatment was regarded as efficient based on positive findings at exploration (appendicitis or other surgical diagnosis). Negative findings at exploration were regarded as surgical failure by protocol. Secondary endpoints were minor complications, duration of hospital stay and patient experience of abdominal pain or discomfort at follow-up.
Statistical analysis
The χ2 test was used to check for differences between proportions. Student’s t test was used for comparisons of continuous variables between groups in order to apply high statistical power, although some variables may not be normally distributed without any bearing difference in this kind of large material as specifically confirmed by nonparametric statistics. p < 0.05 was considered significant in two-tailed tests. SPSS ver. 17.0 (SPSS, Inc., Chicago, IL, USA) was used for the statistical calculations.
The study was approved by the regional Committee of Ethics in Gothenburg, Sweden (367-08).
Results
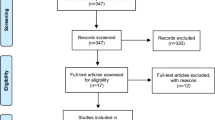
Between May 2009 and February 2010 a total of 558 consecutive patients were hospitalized due to acute appendicitis and were all offered antibiotics as their first-line therapy according to our hospital clinical guidelines during this study period. Accordingly, 442 patients (79 %) received antibiotics as the first-line therapy and 111 patients (20 %) had surgery as their primary treatment (Fig. 1). The most common reasons for primary surgery were patient preference (56 patients, 50 %) and a surgeon’s decision for indication of acute operation (35 patients, 32 %). Five patients improved without any treatment but were still diagnosed as having acute appendicitis. Nine patients were either pregnant or assumed to have recurrence of appendicitis (Fig. 1).
Patient characteristics
Clinical, laboratory, and diagnostic variables at diagnosis of acute appendicitis before the start of any treatment are given in Table 1. Patients who received primary surgery had significantly higher white blood cell counts (WCC) and more local or general peritonitis. Patients who successfully recovered on antibiotics alone had significantly lower WCC, neutrophils, and temperature than patients who failed to improve with primary antibiotics. Radiological imaging was performed to a greater extent in patients with primary surgery (Table 1); CT investigations showed clear-cut or assumed appendicitis in 71 % of patients on primary antibiotics and in 85 % of patients on primary or rescue surgery as expected [19].
Treatment efficacy
Of the 442 patients who received antibiotics as the first-line therapy, 342 (77 %) experienced successful recovery and 100 patients (23 %) had subsequent rescue appendectomy (Table 2). The main reason for surgery subsequent to primary treatment with antibiotics was lack of improvement within 12–24 h (Table 3). Diagnoses in patients who experienced rescue surgery are given in Table 4. Among the 111 patients who had primary surgery, 98 (88 %) had appendicitis or other surgically curable diagnoses. Thus, 12 % were negative explorations. Ninety-two percent of extirpated appendices were sent for histopathology (PAD) (Table 4).
The proportions of phlegmonous, gangrenous, and perforated appendicitis did not differ between patients who had primary surgery and those who had rescue surgery (Table 4), and they agreed with frequencies reported for patient cohorts in Sweden. Thus, treatment efficacy of acute appendicitis appeared to be 77 % for antibiotics as the first-line therapy (Table 2).
Recurrences
Of the 342 patients who initially recovered on antibiotics without surgery, 38 (11 %) had experienced recurrent appendicitis at the 1-year follow-up (Table 2). Time to recurrence varied from 2 weeks up to the end of follow-up (12 months), with a mean time of 5 months. Relapsing patients were men and women between 17 and 89 years old; 33 of these patients were treated with appendectomy. The diagnoses at operation are given in Table 4. Six of these 38 patients had a second round of antibiotics treatment according to their own wishes; one of them did not recover and had appendectomy. The same diagnostic criteria were used for patients with recurrent abdominal pain as for patients at first admission for abdominal pain.
Major complications
Major complications within the 1-year follow-up did not differ significantly between patients who received primary antibiotics treatment and those who had primary surgery (Table 5). There was no difference in major complications between patients who recovered successfully on primary antibiotics and those who had subsequent rescue surgery following failed treatment with primary antibiotics. The five patients who recovered without treatment did not have any major complications and are therefore not included in Table 5. Appendicitis was confirmed by CT in two of these patients, while three patients did not have CT investigations.
Abscess formation was the most common complication following either primary antibiotics or primary surgery. In the antibiotics group, six patients were later operated on because of suspected appendicitis (diagnostic laparoscopy or open appendectomy) without any positive findings, i.e., it was an unnecessary operation by protocol. One patient was treated successfully with antibiotics but had recurrent problems with abdominal pain, abscess, and fistula and was finally diagnosed with Crohn’s disease and later had a ileocecal resection. One patient, treated with primary antibiotics, developed an abscess that required operative drainage. One patient operated on due to recurrence suffered wound rupture and therefore had reoperation. Likewise, one patient operated on after failure with antibiotics developed a wound hernia and underwent reoperation with hernia mesh repair. Another patient operated on after failure with antibiotics came back a few days after discharge with acalculous cholecystitis, which was treated conservatively.
Reoperations were performed on two patients who had primary surgery: one for paralytic ileus and one for abscess formation. One patient with primary surgery had small bowel obstruction that resolved without surgery.
Minor complications
Minor complications were twice as common among patients with primary surgery compared to patients treated with primary antibiotics (Table 6). Also, minor complications were three times higher in patients with antibiotics failure compared to those who successfully recovered on primary antibiotics. The most common complications among operated patients were prolonged postoperative course (vomiting, intestinal paralysis) and wound infection, and among antibiotics-treated patients, the most common complication was some side effect of the antibiotics (mainly diarrhea). The five patients who recovered without treatment did not experience complications.
Patient experience
The proportions of patients who experienced some kind of abdominal discomfort after 6 and 12 months did not differ between the antibiotics and the surgery group; after 12 months 27 % had some kind of abdominal symptom. The figures are based on questionnaire answers from 411 (74 %) patients at 6 months and from 382 (69 %) patients at 12 months. The proportion that answered the questionnaire was similar in both groups.
Duration of antibiotic therapy
Patients treated with first-line antibiotics had the same number of days of intravenous antibiotic therapy as patients who had primary surgery with subsequent perioperative antibiotics (1.6 ± 0.2 days). Patients who were operated on after primary antibiotics failure experienced prolonged antibiotic therapy (2.3 ± 0.1 days) compared to those who recovered on primary antibiotics alone, as expected (p < 0.001). (The total number of days on antibiotics was not specifically measured in the present study, but it was 10 ± 0.3 vs. 4.6 ± 0.4 days in our previous randomized study [9]) Time from appearance in the emergency ward until start of intravenous antibiotic therapy was prolonged for patients who recovered on primary antibiotics (9.8 ± 0.4 h) compared to those who failed on primary antibiotics and had subsequent rescue surgery (6.0 ± 0.4 h; p < 0.001).
Hospital stay
Duration of the primary hospital stay was significantly shorter in patients who received primary antibiotics (2.3 ± 0.1 days) compared to the stay of those who had primary surgery (2.9 ± 0.3; p < 0.025). Patients who were operated on due to primary antibiotics failure had a significantly longer hospital stay (3.6 ± 0.2 days) compared to those who recovered on primary antibiotics alone (1.9 ± 0.1 days; p < 0.001).
Discussion
The results of the present study show that the modern treatment of acute appendicitis may be changing. Previous randomized controlled studies have indicated that a majority of patients with acute appendicitis will heal with antibiotic treatment without the need for surgery, although such studies have displayed various kinds of scientific limitations due to unavoidable ethical considerations in protocol design [8–10]. The most recent randomized controlled study was based on short-term surrogate markers for clinical outcome within 30 days of primary treatment. Its relevance for clinical outcome is therefore difficult to evaluate [11]. Besides, those patients were treated with a combination of amoxicillin and clavulanic acid, which are usually regarded less than ideal for gastrointestinal infections. Our previous study included unselected patients between 18 and 85 years of age to be treated by either antibiotics or conventional appendectomy following randomization [9]. The results agreed with those of other selected patient groups, where more than 75 % of all patients with acute appendicitis recovered on antibiotics without the need of surgical exploration before discharge from the hospital [8, 10]. However, criticism has been raised against our previous study design, since surgeons in charge or on call could decide to operate against the allocation by chance when randomized, despite final analyses by intention to treat [9]. A potential bias of our previous patient selection was, however, not possible to circumvent because of ethical considerations and permission [9]. Therefore, it could not be determined to what extent any selection bias in allocation of patients contributed to our otherwise clear results; which were highly debated among surgeons. This hesitance for a paradigm shift in treatment of acute appendicitis was characterized in a recent review and in a Cochrane Database Systems Review [3, 20].
In the light of previous uncertainties on biased patient selection, we decided to test the present research protocol. This means that a clinical decision was made to offer all consecutive patients hospitalized for acute appendicitis treatment with antibiotics as the first-line therapy in our university hospital. Again, ethical and medical considerations made it necessary to allow patients to accept or reject our offer. Also, it was necessary to allow the surgeons to make independent medical judgments in their offer for best treatment choice. This algorithm or principle should represent what may be a future application of optimized treatment of acute appendicitis. Therefore, our study represents the first full-scale practical test of the validity of previous randomized studies with daily practical limitations involved, i.e., many surgeons involved and no formally applied diagnostic procedure and criteria for all patients.
It may be regarded as a disadvantage that not all our patients had a CT or US examination, although imaging procedures are neither completely inclusive nor exclusive for diagnosis of early appendicitis, which should be the most preferred status to treat by antibiotics in a first-line algorithm. Therefore, acute appendicitis remains a diagnosis dependent on several criteria due to the lack of strict and highly specific criteria, even when systematic imaging is included. However, assumed appendicitis in the present study represents best available knowledge among university trainee surgeons. Accordingly, our observation that patients who recovered on primary antibiotics showed a higher degree of inconclusive CT findings (~29 vs. ~15 %) should be expected in a protocol where antibiotics is offered before a definite choice for surgical exploration. The alternative, to compare the efficiency of antibiotics only in patients with clear-cut signs of appendicitis on CT, relates to a different clinical question than our present protocol with treatment of unselected patients with clinically assumed appendicitis, including comparatively early appendix inflammation. Of course, this approach may imply some unnecessary antibiotics treatment due to bias inclusion of patients with nonspecific abdominal pain. However, this drawback should not be important when patients with increased CRP are treated, indicating a very high probability of any kind of abdominal bacterial infection or tissue damage where bacterial complications may be subsequent. In our present and previous studies, greater than 97 % of all patients with acute appendicitis had elevated serum CRP [9], always indicating some kind of cellular infection/inflammation and usually not of viral origin.
Our present results agree with those of most randomized studies, i.e., a majority of patients will recover on antibiotics as the first-line therapy [8–10]. Thus, in the present study 77 % of all patients with presumed acute appendicitis, based on overall clinical criteria, recovered initially, and 69 % of all these patients remained without relapse after at least 1 year of follow-up. It is likely that the same success should be observed for those patients who chose primary appendectomy. It remains to be confirmed what the relapse will be after 5, 10, and 30 years of follow-up.
It is important to emphasize that major complications did not differ significantly between patients who received primary antibiotics and those who were recommended for or chose primary surgery. Also, there was no difference in major complications between patients who recovered successfully on primary antibiotics treatment and those who experienced subsequent rescue appendectomy. Interestingly, minor complications were twice as common among patients who had primary surgery compared to patients treated with primary antibiotics, and the proportion of patients who experienced some kind of abdominal discomfort between 6 and 12 months did not differ between the antibiotic and surgical groups. Surprisingly, almost 30 % of all patients had some kind of abdominal symptom at the 12-month follow-up irrespective of their treatment schedule, which agrees with observations by others [10, 21]. Also, it is important to emphasize that patients treated with antibiotics as first-line therapy were not exposed to more intravenous antibiotics than patients who had appendectomy. This may be due to observations that clinicians do not always strictly adhere to intended prophylactic regimens following appendectomy. This fact attenuates arguments against different in-hospital initiation of antibiotic resistance among individuals treated with either antibiotics or appendectomy. Surgeons may be reluctant to accept this fact since it is usually proposed that postoperative treatment of appendectomized patients should have minimal or no perioperative antibiotics, although the significant role of antibiotics in the treatment of both operated on and conservatively treated patients appears quite clear [9, 12]. Anyway, it remains uncertain to what extent a 4–5-day difference in taking oral antibiotics is a real risk factor for increased development of antibiotic resistance in patients on successful primary antibiotics treatment outside of the hospital compared to patients who had surgery plus several days of perioperative in-hospital antibiotics [9].
Based on the results of the present study, we find it clear that physicians can offer evidence-based treatment with antibiotics as first-line therapy for acute appendicitis as long as our confirmed treatment protocol is offered and applied [9]. This means that all or at least most adult patients can be initially treated with antibiotics during a 12–36-h course when particular medical reasons do not argue for acute operation [22]. Such conditions may be generalized peritonitis, systemic sepsis, or any other sign of vital dysfunction [13]. Practically, this means that an emergency operation during at nighttime should not be necessary in the majority of patients with acute appendicitis [23]. Such a change in practice may also attenuate serious surgical complications, which are not negligible [9, 13, 24]. It is also clear that several important questions remain to be determined, such as the proportion of long-term relapse following primary antibiotic treatment, definite economical costs for treatment of acute appendicitis by antibiotics versus conventional surgery, which may be large as indicated in our previous report [9]; and to what extent relapse can be efficiently treated by second and third rounds of antibiotic regimens as suggested from observational data in the present study. It is also not clear how the combinations of antibiotics should be applied for optimal long-term results, since it has not been possible to predict antibiotic regimens based on bacterial cultures on inflamed and necrotic appendices [25, 26]. The clear discrepancy between our experience with antibiotics treatment of acute appendicitis and that of others [11] indicates that the choice of antibiotics makes a difference [9, 11]. Additionally, it will be very interesting to know how systematic oral provision of antibiotics compared to the present regimen of initial intravenous provision and subsequent oral treatment for 9 days.
In conclusion, the present prospective population-based study confirms results in previous randomized studies, that antibiotic treatment can be offered as the first-line therapy to a majority of patients with acute appendicitis without medical drawbacks other than the unknown risk for long-term relapse, which must be weighed against the unpredicted but well-known risk for both early and late serious complications following surgical interventions.
References
Hennelly KE, Bachur R (2011) Appendicitis update. Curr Opin Pediatr 23(3):281–285
D’Souza N (2011) Appendicitis. Clin Evid 7 Jan 2011 http://clinicalevidence.bmj.com
Fitzmaurice GJ, McWilliams B, Hurreiz H, Epanomeritakis E (2011) Antibiotics versus appendectomy in the management of acute appendicitis: a review of the current evidence. Can J Surg 54(3):6610
Mason RJ (2008) Surgery for appendicitis: is it necessary? Surg Infect (Larchmt) 9(4):481–488
Vons C (2009) Can acute appendicitis be treated by antibiotics and in what conditions? J Chir (Paris) 146(Spec No 1):17–21
Andersson RE, Petzold MG (2007) Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg 246(5):741–748
Coldrey E (1959) Five years of conservative treatment of acute appendicitis. J Inter Coll Surg 32:255–259
Styrud J, Eriksson S, Nilsson I et al (2006) Appendectomy versus antibiotic treatment in acute appendicitis: a prospective multicenter randomized controlled trial. World J Surg 30(6):1033–1037. doi:10.1007/s00268-005-0304-6
Hansson J, Korner U, Khorram-Manesh A et al (2009) Randomized clinical trial of antibiotic therapy versus appendicectomy as primary treatment of acute appendicitis in unselected patients. Br J Surg 96(5):473–481
Malik AA, Bari SU (2009) Conservative management of acute appendicitis. J Gastrointest Surg 13(5):966–970
Vons C, Barry C, Maitre S et al (2011) Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet 377(9777):1573–1579
Andersen BR, Kallehave FL, Andersen HK (2005) Antibiotics versus placebo for prevention of postoperative infection after appendicectomy. Cochrane Database Syst Rev (3):CD001439
Andersson MN, Andersson RE (2011) Causes of short-term mortality after appendectomy: a population-based case-controlled study. Ann Surg 254(1):103–107
Fike FB, Mortellaro VE, Juang D et al (2011) The impact of postoperative abscess formation in perforated appendicitis. J Surg Res 170(1):24–26
Ansaloni L, Catena F, Coccolini F et al (2011) Surgery versus conservative antibiotic treatment in acute appendicitis: a systematic review and meta-analysis of randomized controlled trials. Dig Surg 28(3):210–221
Suh SW, Choi YS, Park JM et al (2011) Clinical factors for distinguishing perforated from nonperforated appendicitis: a comparison using multidetector computed tomography in 528 laparoscopic appendectomies. Surg Laparosc Endosc Percutan Tech 21(2):72–75
Andersson RE (2004) Meta-analysis of the clinical and laboratory diagnosis of appendicitis. Br J Surg 91(1):28–37
Wijetunga R, Doust B, Bigg-Wither G (2003) The CT diagnosis of acute appendicitis. Semin Ultrasound CT MR 24(2):101–106
Lai V, Chan WC, Lau HY et al (2012) Diagnostic power of various computed tomography signs in diagnosing acute appendicitis. Clin Imaging 36(1):29–34
Wilms IM, de Hoog DE, de Visser DC, Janzing HM (2011) Appendectomy versus antibiotic treatment for acute appendicitis. Cochrane Database Syst Rev (11):CD008359
Tingstedt B, Johansson J, Nehez L, Andersson R (2004) Late abdominal complaints after appendectomy—readmissions during long-term follow-up. Dig Surg 21(1):23–27
Augustin T, Cagir B, Vandermeer TJ (2011) Characteristics of perforated appendicitis: effect of delay is confounded by age and gender. J Gastrointest Surg 15(7):1223–1231
Hall AB, Freeman T, Banks S (2011) Is it safe? Appendectomies at night at a low-volume center. J Surg Educ 68(3):199–201
Andersson RE (2001) Small bowel obstruction after appendicectomy. Br J Surg 88(10):1387–1391
Lamps LW (2004) Appendicitis and infections of the appendix. Semin Diagn Pathol 21(2):86–97
Bennion RS, Baron EJ, Thompson JE Jr et al (1990) The bacteriology of gangrenous and perforated appendicitis—revisited. Ann Surg 211(2):165–171
Acknowledgments
This work was supported by grants from Region Västra Götaland, Gothenburg Medical Society, the Swedish government (LUA-ALF).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hansson, J., Körner, U., Ludwigs, K. et al. Antibiotics as First-line Therapy for Acute Appendicitis: Evidence for a Change in Clinical Practice. World J Surg 36, 2028–2036 (2012). https://doi.org/10.1007/s00268-012-1641-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-012-1641-x