Abstract
Background
A Billroth I reconstruction with a mechanically sutured anastomosis is commonly performed in gastric cancer patients. Some surgeons prefer to use large circular staplers during suturing to minimize risks for anastomotic stricture and gastric stasis after surgery. The effect of stapler size on anastomotic complications has not been validated.
Methods
This study was conducted with 1,031 patients who underwent gastrectomy and Billroth I reconstruction at Samsung Medical Center in Seoul, Korea, between January 2007 and October 2008. Patients were assigned to group A (384 patients) or group B (647 patients) depending on the size of the circular stapler that the surgeon selected for mechanical anastomosis. A 25 mm circular stapler was used for patients in group A, and a 28 or 29 mm circular stapler was used for patients in group B. Postoperative complications were analyzed retrospectively.
Results
The incidence of complications (e.g., gastric stasis, anastomotic stricture, and bleeding) did not differ significantly between groups. Age greater than 60 years was the only significant risk factor for anastomotic complications identified in univariate and multivariate analyses.
Conclusions
Stapler size was unrelated to complications, such as stricture and gastric stasis. Age was the only significant risk factor for anastomotic complications after gastroduodenostomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since Nance [1] introduced the end-to-end anastomosis using a circular stapler in 1979, this method for gastroduodenostomy has been shown to reduce the time in surgery compared to hand-sewing, with no difference in rates of complication, such as leakage and stricture. In gastric cancer, a mechanical circular stapler is commonly used to perform anastomosis during gastroduodenostomy procedures [2–4]. Although no consensus exists on the ideal size of the stapler for anastomosis, some surgeons prefer to use relatively large circular staplers based on the perception that smaller staplers cause gastric stasis or anastomotic strictures. However, no studies have directly compared outcomes and complication rates in relation to stapler size. The aim of the present study was to compare rates of complications and to investigate the risk factor of anastomotic complications after gastroduodenostomy performed with staplers of different sizes. The complications of interest included bleeding, leakage, stricture, gastric stasis, gastritis, bile reflux gastritis, and esophagitis.
Methods
This study was conducted with 1,245 patients who had undergone Billroth I reconstruction after subtotal gastrectomy. These patients were selected from among 2,369 patients diagnosed with gastric cancer who had undergone gastrectomy at Samsung Medical Center between January 2007 and October 2007. Of the 1,245 patients, we enrolled 1,031 who underwent curative subtotal gastrectomy with the Billroth I reconstruction and who were followed up for at least one year. We retrospectively analyzed the relationships between the size of the mechanical circular stapler and anastomotic complications.
Five surgeons participated in this study. Two of the surgeons used a 25 mm circular stapler (Autosuture, Covidien, Norwalk, CT), and the other three surgeons used either a 28 mm circular stapler (Autosuture, Covidien) or a CDH circular stapler that was 29 mm in size (Ethicon Endo-Surgery; Johnson & Johnson, Cincinnati, OH). Group A was composed of patients for whom a 25 mm circular stapler was used, and group B was composed of patients for whom a 28 mm or 29 mm circular stapler was used.
Laparotomy was performed with an upper-middle incision, and a subtotal gastrectomy and D2 lymphadenectomy with truncal vagotomy were also performed. Mechanical Billroth I reconstruction was then performed with a circular stapler. Postoperative complications were analyzed retrospectively.
Stricture was identified by gastrointestinal symptoms such as dysphagia, early satiety, or eating restriction, or when balloon dilatation was needed for passage of a 9 mm endoscope. Leakage was identified based on patients’ symptoms of leakage or on the drain and radiologic findings. Anastomotic bleeding was defined as the need for transfusion for bleeding after surgery, and delayed gastric emptying was defined as the need for a Levine tube for at least four days after surgery in the absence of any mechanical obstruction [5]. Gastric stasis was defined as gastric residue greater than grade 1 according to the Residue, Gastritis, and Bile (RGB) classification system described by Kubo et al. [6]. The RGB grade was evaluated 12 months after operation based on the endoscopic findings. Marginal ulcers, bile reflux gastritis, and esophagitis were assessed based on endoscopic findings 12 months after operation.
PSPW 17.0 for Windows (SPSS, Chicago, IL) was used to analyze the data. The clinicopathologic findings were confirmed with the chi-square test and Fisher’s exact test, and means were compared with the Mann–Whitney U test. A p value <0.05 was considered statistically significant.
Results
Of the 1,031 patients enrolled in the study, 384 were assigned to group A and 647 to group B. These groups did not differ in age, gender, body mass index (BMI), or disease stage, but they did differ in the number of retrieved lymph nodes (Table 1). No leakage was observed in either group, and the two groups did not differ in the incidence of strictures, bleeding, gastric stasis, marginal ulcers, bile reflux gastritis, or esophagitis (Table 2). There were two cases of stricture in group A, and one case of stricture in group B. In group A, stricture occurred in an 80 year-old man with hypertension and diabetes mellitus, and a 49 year-old woman with no underlying disease. In group B, stricture occurred in a 70 year-old man with a history of cerebrovascular disease that was diagnosed four years before surgery.
Univariate analysis revealed that age greater than 60 years was a significant risk factor for anastomotic complications; sex, stapler size, BMI, retrieved lymph nodes (LN), and disease stage were not significant risk factors (Table 3). Multivariate analysis showed that age greater than 60 years was an independent risk factor for anastomotic complications (Hazard Ratio [HR] = 1.590, p = 0.021; Table 4).
Discussion
Gastric cancer is one of the most common cancers in Korea, and it occurs most frequently in the lower third of the stomach. Distal subtotal gastrectomy with the Billroth I reconstruction is the most commonly used treatment for this type of cancer in Korea [7]. Studies show that anastomosis performed with a stapler is either equivalent or superior to hand-sewn anastomosis for gastroduodenostomy in terms of outcomes and complications [2–4]. Hori et al. [2] suggest that the two techniques differ in terms of time requirements but not in the risks of morbidity and mortality. Although many surgeons perform mechanical anastomosis with a circular stapler because it is convenient and reduces operative time, the effect of stapler size on the risk of complications after gastroduodenostomy is unknown.
The risk for stricture after esophagogastrostomy may be increased by leakage [8] or an inadequate blood supply at the anastomosis site [9]. The size of the stapler may be inversely related to the occurrence of strictures after esophagogastrostomy or esophagojejunostomy [10–12]. Johansson et al. [13] reported that the frequency of anastomotic strictures after total gastrectomy is inversely related to stapler size, but these authors found no relationship between the frequency of strictures and stapler size during esophagogastrostomy after esophagectomy. These studies indicate that decreased blood supply is an important risk factor for stricture formation, so surgery must be performed carefully in the case of eophagojejunostomy after total gastrectomy, in which the blood supply must be sufficient to reach the distant anastomosis.
Previously, we showed that the size of the stapler does not affect the risk for stricture in esophagojejunostomy after total gastrectomy [14]. The frequency of stricture in mechanical gastroduodenostomy ranges from 1.1 to 8.0 % [2–4, 15]. Many surgeons prefer to use relatively large circular staplers because these are presumed to prevent anastomotic stenosis. However, this preference is not based on systematic study.
We observed a total of three cases of stricture. In group A, an 80 year-old man with hypertension and diabetes mellitus experienced a stricture four months after operation; and a 49 year-old woman with no underlying disease developed a stricture four months after operation. In group B, a 70 year-old man with a history of cerebrovascular disease developed a stricture three months after operation. All patients recovered from the stricture after a single balloon dilatation. The presence of vascular disease in two of the three patients suggests that reduced blood supply at the site of the anastomosis induced the stricture. Thus, maintenance of an adequate blood supply may be more important than the size of the stapler for stricture prevention. Anastomic bleeding occurred in two patients in group B and no patients in group A, but this difference was not significant.
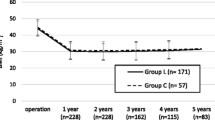
Takahashi et al. [4] reported a higher frequency of gastric stasis after mechanical anastomosis than after hand-sewn anastomosis. These authors noted that a higher risk for gastric stasis in mechanical anastomosis may result from a perturbation of gastric motility after surgery or the location of the anastomosis site. In our study, gastric stasis occurred in 20 patients in group A (5.2 %) and 31 patients in group B (4.8 %) 12 months after surgery. We observed no difference in gastric stasis in relation to stapler size. One patient from group B developed gastric stasis immediately after surgery, but the patient recovered after conservative treatment involving the insertion of a Levine tube. The two groups did not differ in the incidence of gastritis, marginal ulcers, bile reflux gastritis, or esophagitis.
Few studies have assessed complications of anastomosis related to Billroth I reconstruction after surgery for gastric cancer, perhaps because these complications tend to occur at very low frequencies. Park et al. [15] identified three independent risk factors for morbidity after gastrectomy, including age greater than 50 years, combined resection, and Billroth II reconstruction. These authors observed no leakage in the Billroth I reconstruction, and stenosis occurred in 1.1 % of patients. Jeong et al. [16] identified three independent risk factors for morbidity after curative gastrectomy, including male sex, BMI ≥25, and distal pancreatectomy. In their study, luminal bleeding and anastomosis leakage occurred in 2.6 and 0.3 % of patients, respectively.
Although we performed this study retrospectively with a one-year follow-up, our results indicate that age greater than 60 years is an independent risk factor for anastomotic complications. Thus, when older patients undergo these procedures, they should be observed closely during and after surgery. In the future, our findings should be confirmed in a prospective study with a long-term follow-up.
Conclusions
Some surgeons prefer to use a relatively large circular stapler to reduce the risk of anastomotic stricture or gastric stasis during gastroduodenostomy. However, we observed no relationship between rates of anastomotic complications and stapler size. For ease of manipulation and to minimize tissue manipulation, we recommend using one of the smaller staplers for anastomosis during gastroduodenostomy. In addition, age greater than 60 years was associated with anastomotic complications, suggesting that older patients should be observed closely during and after this surgery.
References
Nance FC (1979) New techniques of gastrointestinal anastomoses with the EEA stapler. Ann Surg 189:587–600
Hori S, Ochiai T, Gunji Y et al (2004) A prospective randomized trial of hand-sutured versus mechanically stapled anastomoses for gastroduodenostomy after distal gastrectomy. Gastric Cancer 7:24–30
Mimatsu K, Oida T, Kawasaki A et al (2009) Anastomotic stricture of Billroth-I gastroduodenostomy using a hemi-double stapling technique. Hepatogastroenterology 56:381–384
Takahashi T, Saikawa Y, Yoshida M et al (2007) Mechanical-stapled versus hand-sutured anastomoses in Billroth-I reconstruction with distal gastrectomy. Surg Today 37:122–126
Wente MN, Bassi C, Dervenis C et al (2007) Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 142:761–768
Kubo M, Sasako M, Gotoda T et al (2002) Endoscopic evaluation of the remnant stomach after gastrectomy: proposal for a new classification. Gastric Cancer 5:83–89
Information Committee of the Korean Gastric Cancer Association (2007) 2004 nation wide gastric cancer report in Korea. J Korean Gastric Cancer Assoc 7:47
Dewar L, Gelfand G, Finley RJ et al (1992) Factors affecting cervical anastomotic leak and stricture formation following esophagogastrectomy and gastric tube interposition. Am J Surg 163:484–489
Pierie JP, de Graaf PW, Poen H et al (1993) Incidence and management of benign anastomotic stricture after cervical oesophagogastrostomy. Br J Surg 80:471–474
Berrisford RG, Page RD, Donnelly RJ (1996) Stapler design and strictures at the esophagogastric anastomosis. J Thorac Cardiovasc Surg 111:142–146
Muehrcke DD, Kaplan DK, Donnelly RJ (1989) Anastomotic narrowing after esophagogastrectomy with the EEA stapling device. J Thorac Cardiovasc Surg 97:434–438
Zilling TL, Walther BS, Johnsson F et al (1995) Anastomotic diameter of circular stapled oesophagojejunal anastomoses and its implication for weight development. A clinical and experimental study. Eur J Surg 161:193–198
Johansson J, Zilling T, von Holstein CS et al (2000) Anastomotic diameters and strictures following esophagectomy and total gastrectomy in 256 patients. World J Surg 24:78–84 discussion 84–75
Oh SJ, Baik YH, Hong SK et al (2005) Benign stricture of esophagojejunstomy after radical total gastrectomy. J Korean Gastric Cancer Assoc 5:246–250
Park DJ, Lee HJ, Kim HH et al (2005) Predictors of operative morbidity and mortality in gastric cancer surgery. Br J Surg 92:1099–1102
Jeong O, Park YK, Ryu SY et al (2010) Effect of age on surgical outcomes of extended gastrectomy with D2 lymph node dissection in gastric carcinoma: prospective cohort study. Ann Surg Oncol 17:1589–1596
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, D.H., Oh, C.A., Oh, S.J. et al. Circular Stapler Size and Risk of Anastomotic Complications in Gastroduodenostomy for Gastric Cancer. World J Surg 36, 1796–1799 (2012). https://doi.org/10.1007/s00268-012-1584-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-012-1584-2