Abstract
Background
The purpose of this study was to assess the effect of body position on lower esophageal sphincter (LES) structure and function.
Methods
Symptomatic patients underwent high-resolution manometry in the supine and upright positions followed by pH testing. Regardless of whether there was a positive DeMeester score, isolated upright reflux patterns were considered present when the supine fraction of time pH <4 = 0%. Predominant-upright and predominant-supine bipositional reflux (SBR) patterns were considered present when the supine fraction of time was <upright fraction of time pH <4 and the supine fraction was >upright fraction of time pH <4, respectively.
Results
Of 128 patients, 35 isolated upright, 55 predominant-upright bipositional, and 27 SBR patients were identified. When supine, LES pressure/length was higher in upright compared to bipositional reflux patients. When upright, there was no difference in LES pressure/length between groups. The LES in isolated upright reflux patients became defective when moved from supine to upright position compared to bipositional patients, where the LES was defective regardless of position. Although the incidence of laryngopharyngeal reflux (LPR) events was comparable between groups, isolated upright patients commonly had a normal DeMeester score.
Conclusion
Position impacts LES competency in those with upright reflux and would not be detected with supine manometry. Upright reflux can be associated with GERD and LPR despite negative pH testing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastroesophageal reflux disease (GERD) is the most common esophageal disorder and can result in a wide variety of clinical presentations, including typical symptoms such as heartburn and regurgitation and atypical symptoms such as cough, hoarseness, and globus sensation. Based on distal esophageal pH testing, three distinct patterns of position-related reflux have been described: upright, supine, and bipositional reflux [1]. Isolated upright reflux may represent the earliest manifestation of GERD, with progression to bipositional reflux signifying a worsening disease state with complete loss of the antireflux barrier. The exact mechanism of upright reflux is poorly understood, although several hypotheses have been suggested [2, 3]. In most patients with upright reflux and laryngopharyngeal reflux (LPR) symptoms, the endoscopic appearance of the gastroesophageal valve appears normal in the supine position but then becomes patulous in the upright position [4]. Using multichannel intraluminal impedance (MII) testing, we have previously demonstrated that proximal reflux events (proximal esophagus or hypopharynx) in patients with LPR symptoms occur almost exclusively in the upright position, and many of the patients in this series had a complete symptomatic response with antireflux surgery despite a normal preoperative DeMeester score [5]. Based on these observations, we hypothesize that the upright body position has a shortening effect on the intragastric lower esophageal sphincter (LES) in select patients with symptoms of LPR that leads to the rapid egress of air and gastric contents. The resultant reflux events are few in number, delivered proximally, of small volume, and rapidly cleared and therefore elude consistent detection with conventional pH testing [6]. We theorize that even if reflux events are detected, it is likely that these patients will not fall within the abnormal range established for patients with typical GERD symptoms.
The purpose of this study was to assess the effect of body position on the LES structure and function and to determine whether the characteristics of reflux events (proximity, content, clearance times) correlate with a particular position-related reflux group.
Materials and methods
Patient population and study design
This retrospective review was performed under the approval of the institutional review board of the University of Pittsburgh. Eligible subjects included patients with typical and/or atypical symptoms of GERD and underwent esophageal objective testing, including barium esophagram, upper endoscopy, supine and upright high-resolution manometry, and 48-h wireless pH monitoring or 24-h MII-pH from December 2009 to November 2010. All antisecretory medication such as proton pump inhibitors (PPI) and H2 blockade was discontinued 10 days prior to pH testing with or without MII testing. Based on the position-related acid exposure time, subjects were categorized into three distinct groups regardless of whether there was a positive DeMeester score: (1) isolated upright reflux, (2) predominant-upright bipositional reflux (UBR), and (3) predominant-supine bipositional reflux (SBR) groups. Detailed demographic data (sex, age, and BMI), GERD symptoms (typical and/or atypical), radiographic and endoscopic findings, and manometric and impedance measurements were reviewed. Typical GERD symptoms included heartburn and/or regurgitation. Atypical symptoms included cough, hoarseness, and globus sensation. Clinical symptoms were categorized into three groups: isolated atypical symptoms, isolated typical symptoms, and combined typical and atypical symptoms. Patterns of antisecretory medication use (type, duration, and effectiveness) were recorded.
Esophageal objective testing
Esophagram and upper endoscopy
All patients underwent radiographic and endoscopic evaluation of the upper gastrointestinal tract. Any observed mucosal changes such as esophagitis or suspected Barrett’s esophagus were recorded. Prior to gastric insufflation, the location of the anatomic gastroesophageal junction (GEJ) and the squamocolumnar junction (SCJ) were measured. Barrett’s esophagus and subsequent biopsy was suspected when the SCJ was variegated and located proximal to the anatomic GEJ. The diagnosis of Barrett’s esophagus required evidence of columnar epithelium with goblet cells on histologic examination. The presence of esophagitis was documented using the Los Angeles Classification [7]. The presence of hiatal hernia was evaluated radiographically, and the appearance of the gastroesophageal flap valve was described based on Hill classification (grade I–IV) [8]. Esophagrams were not consistently performed in both the upright and supine positions.
High-resolution manometry (HRM)
HRM was performed using a solid-state assembly with 36 circumferential sensors spaced at 1-cm intervals (ManoScan, Sierra Scientific Instruments, Inc., Los Angeles, CA) to evaluate the function of the LES and the upper esophageal sphincter (UES) and the esophageal body in both the upright and supine positions. Ten wet swallows (5 cc of water per swallow) were obtained in the supine position followed by five wet swallows in the upright position. Manometric measurements, including resting LES and UES pressures, LES residual pressure, total and intra-abdominal LES lengths, mean peristaltic wave pressure, and size of hiatal hernia, were obtained for the comparison of patients with isolated upright reflux and bipositional reflux. A defective LES was defined as either a LES pressure of <5.0 mmHg, total LES length of <2.4 cm, or intra-abdominal length of <0.9 cm [9]. Abnormal esophageal body peristalsis was defined as failed contractions of >20%, simultaneous contractions of >20%, or low mean wave pressure amplitudes of <30 mmHg. An aperistaltic esophagus was considered present when no contractions were propagated with deglutition. Patients with achalasia were excluded.
Forty-eight-hour wireless pH monitoring
48-h wireless pH monitoring was performed using the Bravo pH Monitoring System (Given® Imaging, Duluth, MN). A wireless pH capsule probe was placed within the distal esophagus 6 cm proximal to the termination of the gastric folds which were used to designate the anatomic GEJ. Symptoms and pH data were collected for 48 h in all patients, and DeMeester score was calculated for each testing day. An abnormal 48-h pH study was defined as a calculated DeMeester score greater than 14.7 on either day. Upright, supine, and total fraction time pH <4 was automatically calculated.
Twenty-four-hour MII
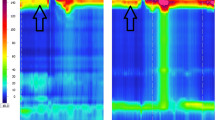
24-h MII was performed using a specialized impedance catheter configured to measure LPR (CZAI-BL-55; Sandhill Scientific, Inc, Highlands Ranch, CO). The configuration of this catheter has been described previously [10]. Briefly, the catheter has two pH probes (hypopharynx and distal esophagus) and three impedance electrodes, one each in the distal (3 and 5 cm proximal to the upper border of the LES) and proximal esophagus (2 and 4 cm distal to the UES) and the hypopharynx (Fig. 1). The catheter was attached to an ambulatory recording device and the total testing period was 24 h. Upright, supine, and total fraction time pH <4 and median acid clearance times were calculated. Content (gas, liquid, and mixed) and proximity of reflux events were recorded.
MII. Upper-left the configuration of a specialized impedance catheter to directly measure LPR. Upper - middle the scheme of full column reflux. Upper - right the scheme of LPR. Lower impedance tracing of acid LPR, which is defined as when retrograde bolus transit occurs across all ring sets and ultimately reaches the hypopharynx and when both esophageal and pharyngeal pH sensors dropping <4 (reproduced from [18] and [5])
Definition of position-related reflux patterns
To determine the effect of position on LES structure and function, we categorized subjects into isolated upright reflux, UBR, and SBR groups based on the position-related fraction of time pH <4. A positive DeMeester score was not required for inclusion in this study. Isolated upright reflux was considered present when the supine fraction of time pH <4 was 0% in the presence of upright reflux events. UBR was considered present when the upright fraction of time pH <4 was greater than the supine fraction of time, whereas SBR was considered present when the supine fraction time was equal to or greater than the upright fraction of time. Exclusion criteria included patients with achalasia and those who had no reflux events during the testing period.
Data interpretation and definition of proximal reflux events based on MII
Data were transferred and analyzed using dedicated software (Bioview AnalysisTM, Sandhill Scientific Inc., Highlands Ranch, CO). A retrograde 50% fall in impedance from the mean baseline impedance between the two electrode pairs indicated the presence of liquid-only reflux. The mean was calculated from baseline impedance values measured 5 s prior to the decrease. Gas reflux was defined as an abrupt increase in impedance >3,000 Ω in any two consecutive impedance sites, with one site having an absolute value >7,000 Ω. Mixed liquid–gas reflux was defined as an abrupt increase in impedance (gas) occurring during or immediately before liquid reflux. LPR event was considered present when retrograde bolus transit reached the hypopharynx regardless of whether there was a change in pH (Fig. 1). A full-column reflux event was defined as reflux that reached the electrode pairs 2 cm distal to the cricopharyngeus muscle but did not reach the hypopharyngeal ring set. Abnormal proximal exposure was considered present when patients had one or more LPR events per day and/or five or more full-column reflux events per day [5]. DeMeester score was calculated for the distal pH monitor using established criteria [11]. Meal times were excluded from the analysis.
Data analysis
After assessing the distribution of the data, values were expressed as a median with interquartile range or mean ± standard deviation as appropriate. Supine and upright HRM differences in esophageal structure and function were compared within and between upright and bipositional reflux groups. Because experimental data were not normally distributed, statistical analysis was performed by means of the nonparametric Wilcoxon signed-rank test using SPSS software ver. 18.0 (SPSS, Inc., Chicago, IL) and p < 0.05 was considered significant.
Results
Patient demographics and esophageal objective testing
From December 2009 to November 2010, 128 symptomatic patients underwent supine and upright HRM followed by either 48-h pH testing (n = 58) or 24-h MII (n = 70) for the evaluation of GERD and/or LPR symptoms. 35 patients were defined as having isolated upright reflux, 53 patients as having UBR, and 27 patients as having SBR. 13 patients were excluded from the final analysis (Fig. 2). Mean age and BMI were comparable among the three groups. The distribution of clinical symptoms was comparable among the groups, and more than half of the patients in each group had LPR symptoms (isolated or combined) (Table 1). The prevalence of hiatal hernia and esophageal mucosal injury such as esophagitis and Barrett’s esophagus were not different between the groups. However, patients with bipositional reflux were more likely to have severe forms of esophageal mucosal injury such as Los Angeles Classification grade D esophagitis, and the severity of esophageal mucosal injury increased sequentially from isolated upright reflux to UBR and then to SBR. Patients with isolated upright reflux and UBR were more likely to be responsive to PPI therapy than those with SBR. Although a large number of patients with isolated upright reflux (32/35, 91%) had a negative DeMeester score, nearly 70% of patients had either endoscopic or radiographic findings of GERD such as esophagitis, Barrett’s esophagus, or hiatal hernia. More than 60% of patients with UBR and SBR had a positive DeMeester score in conjunction with objective findings of GERD.
Comparison of manometric measurements in isolated upright reflux versus bipositional reflux
In the supine position, resting LESP was higher, and both overall and intra-abdominal LES lengths were significantly longer in the isolated upright reflux group compared to the SBR group. Patients with UBR appeared to have lower LESP and shorter LES length compared to those with isolated upright reflux, although this comparison did not reach statistical significance (Fig. 3a). When moved into the upright position, the isolated upright reflux group had a significant reduction in resting LESP and shortening of both total and intra-abdominal LES lengths, whereas the SBR group had a reduction in resting LESP but no change in both overall and intra-abdominal LES lengths (Table 2). The UBR group had a significant reduction in resting LESP and shortening of overall LES length but no change in intra-abdominal LES length, indicating a complete loss of the intragastric portion of the LES. In the upright position, there was no difference in LESP or LES length among the three groups (Fig. 3b). Based on normative values for pressure and length, the LES in the isolated upright reflux group was more likely to become defective when patients were moved from the supine to the upright position compared to bipositional reflux groups where the LES was commonly defective regardless of body position (Fig. 3c). Bipositional reflux patients had larger hiatal hernias than the isolated upright reflux group, and there was a trend toward size increase when moved from supine to the upright position. In up to 20% of patients in each group, a hiatal hernia was not present in the supine position but appeared in the upright position (Table 2). All groups had a significant reduction of UES resting pressure and a higher mean distal esophageal peristaltic pressure in the upright than in the supine position.
Comparison of LES resting pressure, LES length, and intra-abdominal LES length of reflux patients. a Supine. b Upright. *p < 0.05 was considered significant compared to the isolated upright reflux group. c Change of defective LES defined as either LESP <5 mmHg, overall LES length <2.4 cm, or intra-abdominal LES length <0.9 cm in each group between supine and upright positions. d Composition of proximal reflux events in each group. Iso-U isolated upright reflux, Pred-U predominant-upright, Pred-S predominant-supine
Association between body position and proximal reflux events measured by MII
LPR events were present in 27% (6/22) of the isolated upright reflux group, in 32% (7/22) of the UBR group, and in 14% (2/14) of the SBR group (p = 0.338) (Table 3). The number of patients with isolated upright reflux who had abnormal proximal exposure was comparable between those with LPR and those with typical symptoms (78 vs. 75%) (Table 4). Although there was no difference in the total number of reflux events among the groups, the median acid clearance time was shorter in the upright reflux group than in the UBR and SBR groups (median = 63.5 vs. 149 and 137.5, p = 0.067 and p = 0.085, respectively). The composition of proximal reflux events in the isolated upright reflux group was more likely to be mixed gas–liquid compared to bipositional events, which were mostly liquid (Table 3; Fig. 3d). The incidence of abnormal esophageal motility, including aperistaltic esophagus, was comparable among the groups.
Discussion
The results of the present study demonstrate that in patients with isolated upright reflux, the LES functioned as an intact antireflux barrier in the supine position but became incompetent in the upright position as indicated by a reduction in LESP and length. In addition, a small hiatal hernia appeared in many of these patients when they were positioned upright. Interestingly, there was no difference in LES pressure or length among the three groups in the upright position, with nearly one-half of isolated upright reflux patients converting from normal to abnormal manometric LES criteria. Because the LES was significantly more damaged in the bipositional reflux groups, the “protective” effect of the supine position is lost. This supposition is supported by data demonstrating that patients with bipositional reflux were more likely to have lower upright LESP and length, more severe esophageal mucosal injury, esophageal motility disorder, and a larger hiatal hernia compared to those with solely upright reflux patterns.
A substantial number of patients with isolated upright reflux were found to have objective findings suspicious for GERD such as mild esophageal mucosal injury, small hiatal hernia, and abnormal proximal exposure, even though many had a normal DeMeester score. Interestingly, the prevalence of abnormal proximal exposure was comparable among the groups and this would not have been detected by pH testing in the absence of hypopharyngeal–esophageal impedance and bipositional manometry. We theorize that the mechanism of proximal reflux in the isolated upright and bipositional reflux groups is different, and the DeMeester score is more likely to be normal in isolated upright reflux patients secondary to rapid acid clearance times, shorter reflux events, a normal total number of reflux events, and higher proportion of mixed (gas and liquid) events. Ultimately, the current criteria used to objectify typical GERD are likely insufficient and poorly suited to guide diagnosis and treatment in isolated upright reflux patients with LPR symptoms.
Recently, we demonstrated that proximal reflux events such as LPR are extremely rare in healthy asymptomatic subjects [5]. The mechanism of proximal reflux events has not been well understood. Anatomically, the native LES resides across the diaphragm and is identified as two portions on manometry: intrathoracic and intra-abdominal [10]. Given the fact that the pressure and intra-abdominal length of the LES decrease in proportion to hiatal hernia size, LES function appears to depend on the intra-abdominal portion of the esophagus [12–14]. However, not all patients with hiatal hernia develop gastroesophageal reflux, indicating that the remaining intrathoracic (i.e., intraesophageal) portion of the LES maintains its barrier function [15]. The progression from a normal LES to one that is completely defective correlates with an increasing GEJ diameter secondary to attenuation of the collar-sling musculature; this progression leads to a loss of the acute angle of His and the development of a hiatal hernia [16]. We hypothesize that the transition from isolated upright reflux to bipositional reflux occurs with the loss of the intraesophageal portion of the LES [13]. Along these lines, Pandolfino et al. [17] demonstrated that the composition of refluxate (gas, liquid, and mixed gas–liquid) can be determined by GEJ compliance using a barostat, and the chance of having purely liquid reflux increases with an increasing GEJ diameter and compliance; this finding may explain why patients with GERD have more frequent pure liquid reflux and less frequent gas reflux compared to healthy subjects.
Based on this evidence, we propose a potential mechanism for isolated upright reflux and the relationship to proximal reflux events. The manometrically normal LES (lowest GEJ diameter and compliance) functions as an antireflux barrier to prevent reflux regardless of body position (Fig. 4, upper row). Through the low-compliance LES with a small GEJ diameter, air is vented (belching) with the aid of the transient lower esophageal sphincter relaxation (TLESR) mechanism. Upright reflux patients (intermediate GEJ diameter and compliance) have a competent LES in the supine position and the intrathoracic LES functions as a barrier to reflux; however, in the upright position the intragastric air rushes cephalad and the resultant gastric distention triggers relaxation of the intrathoracic portion of LES via stretch receptors in the stomach. In addition, there is likely a mechanical component related to the decreased valve yield pressure secondary to loss of the intra-abdominal portion of the LES. With air in the proximal stomach in the upright position, the LES is “pried” open with small increases in intra-abdominal or intragastric pressure. Through this intermediate GEJ diameter, gastric contents are aerosolized secondary to the pressurized and accumulated air and thus more likely to deliver mixed gas–liquid into the proximal esophagus or hypopharynx (Fig. 4, middle row). Bipositional reflux patients, especially when reflux events occur predominantly in the supine position, have a completely defective LES with a large GEJ diameter, which enables unpressurized fluid to flow freely into the esophagus regardless of body position, and this sometimes reaches the proximal esophagus or hypopharynx with increases in intra-abdominal pressure (e.g., belching, coughing) or when patients are in the supine position (Fig. 4, bottom row). This hypothesis is further supported by the data that the composition of proximal reflux was more likely to be mixed gas–liquid in the isolated upright reflux patients compared to liquid in especially the SBR patients (Fig. 3d).
There are limitations to the present study. In this study, objective assessment of symptoms using validated questionnaires was not performed. However, the detail and degree of clinical symptoms were meticulously obtained by personal interview at clinic and precisely recorded. In addition, our clinical practice is weighted toward those with LPR symptoms who have undergone MII to evaluate the proximity of reflux events, and this may be associated with selection bias. However, we defined position-related reflux patterns based solely on pH testing and therefore clinical symptoms would be unlikely to affect the manometric measurements of LES structure. Finally, because many upright reflux patients had a normal DeMeester score, it is possible that patients without pathologic reflux were included in the data set, leading to selection bias. This is unlikely because the prevalence of esophageal mucosal injury was similar between groups. In addition, upright reflux patients had a similar number of proximal reflux events compared to bipositional reflux patients, suggesting a different pathologic mechanism.
In conclusion, position change from supine to upright resulted in a reduction of LES pressure and length. Both isolated upright and bipositional reflux patients have abnormal proximal reflux events, likely by different mechanisms. Symptomatic upright reflux is associated with GERD and/or LPR and can frequently occur in the face of negative pH testing. Bipositional HRM should be incorporated into esophageal physiology testing in order to identify a defective LES, especially in isolated upright reflux patients, as it requires only five additional swallows in the upright position.
References
Demeester TR, Johnson LF, Joseph GJ, Toscano MS, Hall AW, Skinner DB (1976) Patterns of gastroesophageal reflux in health and disease. Ann Surg 184(4):459–470
Mittal RK, Holloway RH, Penagini R, Blackshaw LA, Dent J (1995) Transient lower esophageal sphincter relaxation. Gastroenterology 109(2):601–610
Banki F, Mason RJ, Hagen JA et al (2001) The crura and crura-sphincter pressure dynamics in patients with isolated upright and isolated supine reflux. Am Surg 67(12):1150–1156
Perry KA, Enestvedt CK, Lorenzo CS et al (2008) The integrity of esophagogastric junction anatomy in patients with isolated laryngopharyngeal reflux symptoms. J Gastrointest Surg 12(11):1880–1887
Hoppo T, Sanz AF, Nason KS et al (2012) How much pharyngeal exposure is “normal”? Normative data for laryngopharyngeal reflux events using hypopharyngeal multichannel intraluminal impedance (HMII). J Gastrointest Surg 16(1):16–24 discussion 24–25
Oberg S, Peters JH, DeMeester TR et al (1999) Endoscopic grading of the gastroesophageal valve in patients with symptoms of gastroesophageal reflux disease (GERD). Surg Endosc 13(12):1184–1188
Tack J, Koek G, Demedts I, Sifrim D, Janssens J (2004) Gastroesophageal reflux disease poorly responsive to single-dose proton pump inhibitors in patients without Barrett’s esophagus: acid reflux, bile reflux, or both? Am J Gastroenterol 99(6):981–988
Hill LD, Kozarek RA, Kraemer SJ et al (1996) The gastroesophageal flap valve: in vitro and in vivo observations. Gastrointest Endosc 44(5):541–547
Pandolfino JE, Ghosh SK, Zhang Q, Jarosz A, Shah N, Kahrilas PJ (2006) Quantifying EGJ morphology and relaxation with high-resolution manometry: a study of 75 asymptomatic volunteers. Am J Physiol Gastrointest Liver Physiol 290(5):G1033–G1040
Bombeck CT, Dillard DH, Nyhus LM (1966) Muscular anatomy of the gastroesophageal junction and role of phrenoesophageal ligament; autopsy study of sphincter mechanism. Ann Surg 164(4):643–654
Johnson LF, DeMeester TR (1986) Development of the 24-hour intraesophageal pH monitoring composite scoring system. J Clin Gastroenterol 8(Suppl 1):52–58
Jobe BA, Kahrilas PJ, Vernon AH et al (2004) Endoscopic appraisal of the gastroesophageal valve after antireflux surgery. Am J Gastroenterol 99(2):233–243
Kahrilas PJ, Wu S, Lin S, Pouderoux P (1995) Attenuation of esophageal shortening during peristalsis with hiatus hernia. Gastroenterology 109(6):1818–1825
Zaninotto G, DeMeester TR, Schwizer W, Johansson KE, Cheng SC (1988) The lower esophageal sphincter in health and disease. Am J Surg 155(1):104–111
Fein M, Ritter MP, DeMeester TR et al (1999) Role of the lower esophageal sphincter and hiatal hernia in the pathogenesis of gastroesophageal reflux disease. J Gastrointest Surg 3(4):405–410
Seltman AK, Kahrilas PJ, Chang EY, Mori M, Hunter JG, Jobe BA (2006) Endoscopic measurement of cardia circumference as an indicator of GERD. Gastrointest Endosc 63(1):22–31
Pandolfino JE, Shi G, Trueworthy B, Kahrilas PJ (2003) Esophagogastric junction opening during relaxation distinguishes nonhernia reflux patients, hernia patients, and normal subjects. Gastroenterology 125(4):1018–1024
Hoppo T, Jarido V, Pennathur A (2011) Antireflux surgery preserves lung function in patients with gastroesophageal reflux disease and end-stage lung disease before and after lung transplantation. Arch Surg 146(9):1041–1047
Conflicts of interest
The authors have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hoppo, T., Komatsu, Y., Nieponice, A. et al. Toward an Improved Understanding of Isolated Upright Reflux: Positional Effects on the Lower Esophageal Sphincter in Patients with Symptoms of Gastroesophageal Reflux. World J Surg 36, 1623–1631 (2012). https://doi.org/10.1007/s00268-012-1537-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-012-1537-9