Abstract
Background
The number of lymph nodes retrieved and examined from a resected colon cancer specimen may be crucial for correct staging. We examined if efforts to increase the lymph node harvest to more than 12 lymph nodes per specimen would upstage some patients from TNM stage II to III.
Methods
Three hospitals compared results from 2000 with those of 2007 in 421 resected patients with stage II and III colon cancer. Hospital A endeavored to improve the surgical procedure while the pathologists enhanced the quality of lymph node sampling. Hospital B did not make any marked changes, while hospital C introduced the GEWF lymph node solvent (glacial acetic acid, ethanol, distilled water, and formaldehyde) in their pathology method.
Results
In 2000, 12 or more lymph nodes were harvested in 39.6, 45.0, and 21.1% of the specimens from the three hospitals, while the figures for 2007 were 85.7, 42.0, and 90.3%, respectively. The significant increase in lymph node harvest in two of the hospitals in 2007 compared to 2000 (p < 0.001) did not affect the share of patients with stage III in 2007 (38.7%) compared to 2000 (44.1%) (p = 0.260). The number of positive lymph nodes and the lymph node ratio (LNR) decreased from 2000 to 2007. A lymph node yield of 12 or more was not associated with an increased probability of positive lymph nodes in a multivariable logistic regression analysis.
Conclusion
More radical surgery and dedicated pathologists and the use of the GEWF solvent significantly increased the lymph node yield but did not upstage patients from TNM stage II to III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There are clear indications that more extensive surgery for colon cancer will improve the prognosis of the patient [1]. In this context, lymph nodes may act as a surrogate marker for sufficient surgery with the removal of metastatic lymph nodes in TNM (tumor-node-metastases) stage III. However, there are also reports that increased lymph node sampling may improve prognosis even for stage II tumors, indicating that mere removal per se of as many nodes as possible may do something to improve outcome [2, 3]. A lower limit of 12 lymph nodes harvested in colon cancer has been recommended [4]. The hypothesis of this strategy has been that a minimum number of lymph nodes are needed to correctly stage tumors, meaning that the more lymph nodes the more likely the pathologist is to detect metastases, even though 12 is a rather arbitrary level [1, 5, 6].
It is confounding that many variables influence the lymph node harvest, such as patient and tumor characteristics and the surgical and pathological methods used [7]. However, even if many centers have endorsed the concept of detecting a minimum number of lymph nodes, this strategy has been condoned by some [8]. The importance of lymph node detection has even been contradicted through interpretation of American data [9, 10].
In Norway, patients younger than 75 years of age with TNM stage III colon cancer are routinely offered chemotherapy and this has raised overall survival figures [11]. Consequently, it is important to stage patients correctly. Many consider that an increase in the number of harvested lymph nodes will also increase the share of stage III patients, the so-called Will Rogers phenomenon [12]. However, this is largely an assumption that has not really been convincingly shown [9, 13]. In our multicenter study of three Norwegian hospitals, we wanted primarily to examine if an increased lymph node harvest would also cause migration from TNM stage II to III. A secondary aim was to examine if an increase in lymph node yield would also affect the number of N+ nodes and the lymph node ratio (LNR) of positive vs. total number of lymph nodes in each specimen.
Material and methods
Three teaching community hospitals (A, B, C) with stable catchment areas compared results for segmental R0 and TNM stage II to III segmental colon resections from 2000 with those of 2007 in 421 patients, while 144 patients with stage I (n = 90) and IV (n = 54) were excluded from analysis. Patients who had double resections or subtotal colectomy (n = 4) were also excluded. According to the TNM classification, 247 patients (58.7%) were stage II and 174 patients (41.3%) stage III.
The importance of the lymph node (Ln) harvest was examined overall for more than 12 nodes and divided into these four groups: Ln group 1, 0–6 lymph nodes; Ln group 2, 7–11 nodes; Ln group 3, 12–17 nodes; and Ln group 4, >18 nodes. Patient age, gender, and tumor locations are given in Table 1.
Specimen examination and preparation
Hospital A endeavored to improve the surgical procedure in 2007 and recorded data as part of a prospective study. At the same time, the Department of Pathology at hospital A had improved the dissection of colon cancer specimens, including an optimal lymph node sampling. Hospital B did not make any changes for the time being, while hospital C changed their pathology method to include the lymph node-detecting solvent GEWF (glacial acetic acid, ethanol, distilled water, and formaldehyde) to detect a maximum number of lymph nodes [14]. Hospital A fixed the specimens in formalin for a minimum of 2 days and thereafter examined the specimen and retrieved lymph nodes mainly by palpation. The sections were processed embedded in paraffin using standard techniques. Sections were cut at 4 μm and stained with hematoxylin and eosin (HE) for routine histology. Collaboration with pathologists ensured a heightened state of alert regarding lymph node dissection. Moreover, resection specimens with fewer than 12 lymph nodes after the first dissection were evaluated a second time. Hospital B followed a similar procedure except that the pathologist received specimens removed during daytime directly from the operating room and performed a macroexamination before fixation in formalin. Hospital C also followed a similar routine to the first hospital in 2000 but used the lymph node solvent GEWF in 2007. The specimens from this hospital were opened, pinned, and allowed to fix in GEWF for about 48 h. Each specimen was cut in parallel sections about 5 mm thin, and standard sections were taken from different parts of the tumor. All lymph nodes in the mesenteric fat were easily identified as white nodules that were different from the yellow fat. The sections were then processed similar to the other two hospitals.
Surgery
All three hospitals did ordinary colon resections in 2000. This can best be described as intermediate mesocolic resections in the majority of cases. In 2007, hospital A changed to a more standardized radical approach with removal of apical lymph nodes [1]. Surgeons at hospital B did not change their surgical strategy or routine handling of specimens but may have increased their effort inadvertently to raise the number of lymph nodes in the specimens. Hospital C followed a similar open surgical procedure.
Ethics
The Regional Committee for Medical and Health Research Ethics of Western Norway and the Data Inspectorate for National Registries approved this study. The study is part of a prospective project registered with clinicaltrials.gov (NCT00963352).
Statistical analysis
The distribution of lymph nodes was analyzed using three-way and two-way analyses of variance. The TNM stages were compared using Pearson’s χ2 test. The level of significance was set at 0.05 for all statistical tests. All analyses were done using SPSS 17, Syntax04.sps, Output04j, and k.spv.
Results
Demographics, tumor characteristics, and overall lymph node harvest for 421 patients with colon cancer are given in Table 1. There were significantly more female patients operated on in 2000 compared to 2007, but more male patients were operated on in 2007 than in 2000 (p = 0.026), and 64.4% of the patients were 70 years or older. Tumors were most common in the right colon (40.9%) and sigmoid (27.6%). The two cohorts did not differ in mean age, tumor location, or distribution of T categories.
Lymph node harvest overall
The total number of lymph nodes was significantly higher (p < 0.001) in 2007 (n = 15.7) than in 2000 (n = 10.5) (Table 1). The share of patients with a lymph node harvest of 12 or more was significantly higher for hospitals A (p < 0.001) and C (p < 0.001) in 2007. Hospital B had an unchanged harvest (p = 0.887) (Fig. 1).
Table 2 shows that in a multivariable (Poisson regression) analysis, age younger than 70 years (p < 0.001), year 2007 (p < 0.001), hospital A and C vs. B (p = 0.028), location of tumor in the right colon (p < 0.001), and T category (p = 0.027) were significant variables for an increased lymph node count.
Detection of positive lymph nodes and lymph node ratio (LNR)
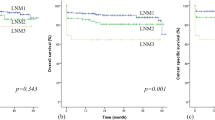
The number of positive lymph nodes did not increase overall from 2000 to 2007 (p = 0.563) (Table 3). When all three hospitals combined were compared for year 2000 vs. 2007, there was a significant decrease in 2007 (p = 0.004). Hospitals A and B found a mean of 2.6 positive nodes in 2000 and a mean of 1.0 positive nodes in 2007, but hospital C increased the number from 1.2 to 2.1 positive nodes.
The presence of N+ was found in a simple logistic regression analysis to have age <70 years, location in the right colon, and T category as significant variables (Table 4). Similarly, in multiple regression analysis, age <70 years (p = 0.016), location in the right colon vs. left colon (p = 0.023), and T category (p > 0.001) increased N+ significantly. When Ln groups were compared per year, we did not find that patients with a high lymph node count in 2000 and 2007 (Ln groups 3 and 4: ≥12 lymph nodes) had more N+ (stage III) than patients with Ln groups 1 and 2 (p = 0.441).
Overall, there was a significant decrease in LNR at stage III from 2000 to 2007 (p < 0.001). LNR decreased despite an increasing number of lymph nodes in stage III patients (Fig. 2). However, when the hospitals were compared separately, only hospital A had a significant decrease in LNR from 2000 to 2007 (p = 0.023) (Table 3).
TNM stage II and III numbers
No stage migration occurred even though the lymph node harvest was significantly better in 2007 (p < 0.001). The TNM stage distribution did not significantly change when divided into hospitals A (p = 0.154), B (p = 0.614), and C (p = 0.838). The result was similar overall (p = 0.402). Table 4 shows that the detection of the total number of lymph nodes had no influence on the occurrence of a TNM stage III tumor. Stage III was more likely to be diagnosed in younger patients, in right colon cancers compared to the sigmoid colon, and in category T4.
A rather spurious effect is that the likelihood of having a TNM III cancer was much higher for stage T1 + 2 than for stage T3 or T4. This was probably a selection effect as most T1 + 2 patients were excluded from the analysis because they had mostly TNM 1.
Discussion
The lymph node yield from colon cancer specimens may be a surrogate measure for radical colon cancer surgery. It has been suggested by some that the detection of a minimum number of lymph nodes in the specimen is necessary for a proper staging of the tumor [5]. A lower limit of 12 lymph nodes has been endorsed by international organizations [4], although 18 has also been suggested [6] or even as many as possible [1]. Thus, as a consequence, tumors would be upstaged and a worse prognosis could be expected unless adjuvant treatment would compensate for this, according to the authors of a recent Dutch report [5]. They found a rate of 36.3% N+ in patients with only 6–11 lymph nodes in the specimen while 12 or more yielded a rate of 41% N+. In patients with 12 or more lymph nodes this effect seemed to level of. A recent large Canadian survey found that the effect of the number of lymph nodes on stage composition applied only when there were fewer than 7 lymph nodes [15]. Overall, our study population had stage III tumors in 41.3% of the patients. This is only slightly less than the 46–48% that others have found when stage I and IV are excluded [1, 16, 17]. However, if studies on lymph node harvest and its effect on staging are based on less-than-optimal surgery and pathology methods, there is the potential for several confounding factors [7]. A large national Norwegian study found a 5% increase to 35% in N+ patients during two recent time periods but did not offer further explanation for this [11].
A concept of upstaging may rest in part on the hypothesis that skip lesions abound. Merrie et al. [18] found an 18% incidence of skip lesions using PCR, but it is questionable if these were skip lesions in the true meaning of the word as only 5% had lesions detected in apical nodes in Dukes B patients. Only about 1% had positive apical nodes without histological proof of metastases in nodes closer to the colonic wall. The importance of finding skip lesions with respect to the prognosis of the patient remains to be proven. A recent study of nodal ultrastaging found only 30% N+ in colorectal cancer specimens examined with conventional histology, even with a mean number of 20 lymph nodes, but increased this share to 44.3% after ultrastaging [19]. In their resections, more than 80% had 12 or more nodes detected. Ultrastaging with detection of cancer cell clusters of <0.2 mm did not significantly change 4-year disease-free survival. Detection of micrometastases (MM) (cell clusters >0.2–2 mm) was recognized as true upstaging and these received adjuvant chemotherapy. They found that a patient with >12 nodes harvested and N0, without micrometastases (N0i-), were cured with surgery alone, while harvesting 12 lymph nodes was significant for the 4-year disease-free survival figures.
Stage 1 may perhaps have fewer detectable lymph nodes [7]. TNM stages were not a significant variable for the overall lymph node count in our study. It follows that the picture is somewhat confusing as to what is really achieved with more extensive surgery and a higher lymph node yield. Our results showed, first of all, that it is possible to increase the lymph node yield by various independent methods. A conjoint effort by surgeons and pathologists in one hospital resulted in a significant increase in the number of patients with a harvest of 12 or more lymph nodes using conventional methods for histology. The use of the lymph node detection solvent GEWF caused a highly significant increase of lymph nodes in hospital C. However, no increase in stage III over stage II was detected when all hospitals were analyzed together. In fact, a slight and probably coincidental drop was found at hospital A. In 2000 the mean number of positive nodes in the three hospitals was 3.6 compared to 3.7 in 2007. This demonstrates that only the number of negative nodes rose appreciably in the two hospitals with an improved harvest and examination with routine staining methods. This is in concert with a recent Japanese study [20].
Some have also focused on lymph node ratio (LNR) as a prognostic factor, meaning that the higher the ratio the worse the prognosis [17, 21, 22]. However, LNR did not matter when fewer than 10 lymph nodes were detected [23]. The explanation for this is obscure but may perhaps be explained by inferior surgical quality [1]. In hospitals A and C with an increased yield, the ratio fell with an increasing number of nodes. In hospital B, with an unchanged number of nodes, the ratio was unchanged. Overall, the LNR decreased with an increasing number of lymph nodes. This suggests that inadequate resections with many positive nodes will have a higher ratio and thus indicate a poor prognosis because of less extensive surgery. Another explanation is that a high ratio suggests a worse biological behavior in itself if a large number of positive nodes are found. Rosenberg et al. [17] found a decreasing survival rate with increasing LNR. They used statistically identified cutoff values from an earlier work on a population cohort consisting of 17,134 patients from the Munich region. They showed better prognostic discrimination with LNR than with pN, and LNR was useful in patients with a lymph node harvest of both more and fewer than 12 nodes.
The prognostic value of a high lymph node yield in stage III patients has been debated. Some authors argue that a high lymph node harvest does not improve prognosis for patients with a high LNR [5, 21] because the disease is no longer localized and adjuvant therapy is necessary. Although the prognosis is still worse with a high LNR than with a low LNR, patients with a low LNR, as well as stage II patients, may benefit from a high lymph node harvest [17]. The reason for this is obscure but biological factors may be important [10]. Radical lymph node removal, even if it does not increase survival, may potentially reduce local recurrences. This should be of importance to the patient.
With increased scrutiny of the specimen and use of PCR techniques, one will more often find smaller nodes and so-called tumor deposits that make it increasingly difficult to agree on the meaning of such findings. A tumor collection of more than 3 mm or with a round contour has been suggested to represent a lymph node [7, 22]. Further subdivisions have emerged in the shape of micrometastases, sub-micrometastases, and isolated tumor cells categories, but opinions have been divided over their importance [7, 19, 24]. Despite this, the UJCC 7th edition has taken this issue into account, to much criticism [25]. A recent review found no significance attached to tumor deposits in the mesentery [24]. Therefore, it seems that even though refined and meticulous techniques are able to increase the number of metastases or tumor deposits in the specimen, the importance of such findings has not as yet been ascertained. Even though the discovery of micrometastases may upstage some patients, this upstaging does not relate to an increased survival and consequently it is still uncertain what oncological importance it may carry [19].
So far, only the number of lymph nodes in the specimen seems to have a bearing on the prognosis, but opinions differ as to what influences this parameter, i.e., patient, tumor, surgeon, or pathologist [10], even though the pathologist seems to hold the key [7]. It is also debatable what should be the minimum number, but we had agreed with our pathologists to look for at least 12 lymph nodes. Hohenberger et al. [1, 26] found improved prognosis when more than 28 nodes were detected. In contrast, Wong et al. [9] did not show that lymph node numbers in US hospitals were associated with staging or survival. Nevertheless, the metastatic pattern to regional lymph nodes would support extensive surgery in most cases [26–29]. However, it was not within the scope of the present study to examine the effect of an increased lymph node yield on outcome. This will be studied in forthcoming reports.
We conclude that the lymph node harvest in our patients could be increased significantly by different surgical and pathological methods without increasing the share of stage III patients compared with stage II patients. In concert, the overall number of N+ fell and so did the LNR. In effect, the Will Rogers phenomenon did not occur. Thus, the whole concept that more lymph nodes are needed to stage patients correctly is contentious.
References
Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S (2009) Standardized surgery for colonic cancer: complete mesocolic excision and central ligation—technical notes and outcome. Colorectal Dis 11:354–364 discussion 364–365
Tsai HL, Lu CY, Hsieh JS, Wu DC, Jan CM, Chai CY, Chu KS, Chan HM, Wang JY (2007) The prognostic significance of total lymph node harvest in patients with T2-4N0M0 colorectal cancer. J Gastrointest Surg 11:660–665
Swanson RS, Compton CC, Stewart AK, Bland KI (2003) The prognosis of T3N0 colon cancer is dependent on the number of lymph nodes examined. Ann Surg Oncol 10:65–71
Nelson H, Petrelli N, Carlin A, Couture J, Fleshman J, Guillem J, Miedema B, Ota D, Sargent D (2001) Guidelines 2000 for colon and rectal cancer surgery. J Natl Cancer Inst 93:583–596
Kelder W, Inberg B, Schaapveld M, Karrenbeld A, Grond J, Wiggers T, Plukker JT (2009) Impact of the number of histologically examined lymph nodes on prognosis in colon cancer: a population-based study in the Netherlands. Dis Colon Rectum 52:260–267
Polignano F, Henderson N, Alishahi SM, Zito A (2006) Laparoscopic colectomy for cancer and adequate lymphadenectomy: association between survival and number of lymph nodes. Surg Endosc 20:996–997
Storli K, Lindboe CF, Kristoffersen C, Kleiven K, Søndenaa K (2010) Lymph node harvest in colon cancer specimens depends on tumour factors, patients and doctors, but foremost on specimen handling. APMIS 119:127–134
Sjövall A, Granath F, Cedermark B, Glimelius B, Holm T (2006) Loco-regional recurrence from colon cancer: a population-based study. Ann Surg Oncol 14:432–440
Wong SL, Ji H, Hollenbeck BK, Morris AM, Baser O, Birkmeyer JD (2007) Hospital lymph node examination rates and survival after resection for colon cancer. JAMA 298:2149–2154
Hsu CW, Lin CH, Wang JH, Wang HT, Ou WC, King TM (2009) Factors that influence 12 or more harvested lymph nodes in early-stage colorectal cancer. World J Surg 33:333–339. doi:10.1007/s00268-008-9850-z
Nedrebø BS, Søreide K, Eriksen MT, Dørum LM, Kvaløy JT, Søreide JA, Kørner H (2011) Survival effect of implementing national treatment strategies for curatively resected colonic and rectal cancer. Br J Surg 98:716–723
Feinstein AR, Sosin DM, Wells CK (1985) The Will Rogers phenomenon. Stage migration and new diagnostic techniques as a source of misleading statistics for survival in cancer. N Engl J Med 312:1604–1608
Bui L, Rempel E, Reeson D, Simunovic M (2006) Lymph node counts, rates of positive lymph nodes, and patient survival for colon cancer surgery in Ontario, Canada: a population-based study. J Surg Oncol 93:439–445
Iversen LH, Laurberg S, Hagemann-Madsen R, Dybdahl H (2008) Increased lymph node harvest from colorectal cancer resections using GEWF solution: a randomised study. J Clin Pathol 61:1203–1208
Baxter NN, Ricciardi R, Simunovic M, Urbach DR, Virnig BA (2010) An evaluation of the relationship between lymph node number and staging in pT3 colon cancer using population-based data. Dis Colon Rectum 53:65–70
Prandi M, Lionetto R, Bini A, Francioni G, Accarpio G, Anfossi A, Ballario E, Becchi G, Bonilauri S, Carobbi A, Cavaliere P, Garcea D, Giuliani L, Morziani E, Mosca F, Mussa A, Pasqualini M, Poddie D, Tonetti F, Zardo L, Rosso R (2002) Prognostic evaluation of stage B colon cancer patients is improved by an adequate lymphadenectomy: results of a secondary analysis of a large scale adjuvant trial. Ann Surg 235:458–463
Rosenberg R, Engel J, Bruns C, Heitland W, Hermes N, Jauch KW, Kopp R, Pütterich E, Ruppert R, Schuster T, Friess H, Hölzel D (2010) The prognostic value of lymph node ratio in a population-based collective of colorectal cancer patients. Ann Surg 251:1070–1078
Merrie AE, Phillips LV, Yun K, McCall JL (2001) Skip metastases in colon cancer: assessment by lymph node mapping using molecular detection. Surgery 129:684–691
Bilchik A, Nissan A, Wainberg Z, Shen P, McCarter M, Protic M, Howard R, Elashoff D, Tyler J, Peoples GE, Stojadinovic A (2010) Surgical quality and nodal ultrastaging is associated with long-term disease-free survival in early colorectal cancer. Ann Surg 252:467–476
Kobayashi H, Mochizuki H, Sugihara K, Morita T, Kotake K, Teramoto T, Kameoka S, Saito Y, Takahashi K, Hase K, Oya M, Maeda K, Hirai T, Kameyama M, Shirouzu K, Muto T (2007) Characteristics of recurrence and surveillance tools after curative resection for colorectal cancer: a multicenter study. Surgery 141:67–75
Wang J, Kulaylat M, Rockette H, Hassett J, Rajput A, Dunn KB, Dayton M (2009) Should total number of lymph nodes be used as a quality of care measure for stage III colon cancer? Ann Surg 249:559–563
Quirke P, Morris E (2007) Reporting colorectal cancer. Histopathology 50:103–112
Berger AC, Sigurdson ER, LeVoyer T, Hanlon A, Mayer RJ, Macdonald JS, Catalano PJ, Haller DG (2005) Colon cancer survival is associated with decreasing ratio of metastatic to examined lymph nodes. J Clin Oncol 23:8706–8712
Nagtegaal ID, Quirke P (2007) Colorectal tumour deposits in the mesorectum and pericolon; a critical review. Histopathology 51:141–149
Sobin LGM, Wittekind C (eds) (2009) International union against cancer TNM classification of malignant tumours, 7th edn. Wiley-Blackwell, Hoboken
West NP, Hohenberger W, Finan PJ, Quirke P (2009) Mesocolic plane surgery: an old but forgotten technique? Colorectal Dis 11:988–989
Yada H, Sawai K, Taniguchi H, Hoshima M, Katoh M, Takahashi T (1997) Analysis of vascular anatomy and lymph node metastases warrants radical segmental bowel resection for colon cancer. World J Surg 21:109–115. doi:10.1007/s002689900202
Toyota S, Ohta H, Anazawa S (1995) Rationale for extent of lymph node dissection for right colon cancer. Dis Colon Rectum 38:705–711
Nash GM, Row D, Weiss A, Shia J, Guillem JG, Paty PB, Gonen MR, Weiser M, Temple LK, Fitzmaurice G, Wong WD (2011) A predictive model for lymph node yield in colon cancer resection specimens. Ann Surg 253:318–322
Acknowledgment
The study was supported by a grant from the Western Norway Hospital Trust, The University of Bergen, and Haraldsplass Deaconal Hospital. We thank Cand. Med. Malte Schmidt for organizing the statistical data file.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Storli, K., Søndenaa, K., Furnes, B. et al. Improved Lymph Node Harvest from Resected Colon Cancer Specimens Did Not Cause Upstaging from TNM Stage II to III. World J Surg 35, 2796–2803 (2011). https://doi.org/10.1007/s00268-011-1248-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-011-1248-7