Abstract
Background
Laparoscopy-assisted proximal gastrectomy (LAPG) remains a relatively uncommon procedure because of certain technical issues, such as curability, safety, and retention of postoperative patients’ quality of life. The aim of the present study was to evaluate the feasibility of a newly developed LAPG procedure for early-stage proximal gastric cancer.
Methods
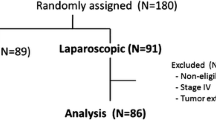
We enrolled 37 consecutive patients who were preoperatively diagnosed with cT1N0M0 primary gastric cancer in the upper third of the stomach with the primary tumor diameter less than 4 cm. Laparoscopy-assisted proximal gastrectomy with sentinel node (SN) mapping and esophagogastric anastomosis with a circular stapler and transoral placement of the anvil was attempted.
Results
The LAPG procedure was completed in 36 patients. It was converted to laparoscopy-assisted total gastrectomy in one patient because one SN detected intraoperatively was positive for metastasis by intraoperative pathological diagnosis. There were no severe postoperative complications in any patient. Only one patient (3%) complained of mild reflux symptoms immediately after operation, which were graded endoscopically as B by the Los Angeles Classification of gastroesophageal reflux disease; however, the symptoms were controlled well by a proton-pump inhibitor. Sentinel nodes were detected successfully in 37 (100%) of our patients. The mean number of dissected lymph nodes and identified SNs per case was 29.7 and 5.8, respectively. The sensitivity of prediction of nodal metastasis (including isolated tumor cells) and diagnostic accuracy based on SN status were 100% (3/3) and 100% (37/37), respectively. All patients have been free from recurrence for a median follow-up period of 26 months.
Conclusions
This study reveals that our novel LAPG approach is curative and represents a feasible minimally invasive surgical procedure with minimal morbidity and postoperative reflux esophagitis in patients with upper-third early-stage gastric cancer.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In Japan, early gastric cancer (cT1) is found in many asymptomatic patients due to recent advances in endoscopic diagnosis, and the proportion of cT1 to all of gastric cancer patients currently reaches in excess of 50% in major institutions [1]. Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) have already been accepted as the most minimally invasive procedures for the resection of early gastric cancer [1]. Laparoscopic gastrectomy represents an important intermediate option between EMR/ESD and open surgery for patients with gastric cancer [2]. More recently, the technique of laparoscopic gastrectomy has shifted from wedge resection to more radical procedures, such as laparoscopy-assisted distal gastrectomy (LADG) or laparoscopy-assisted total gastrectomy (LATG) with D1 or D2 lymphadenectomy, which is comparable to conventional open surgery and can be performed even in patients with advanced cancer [3, 4]. In fact, many patients are currently treated by advanced laparoscopic gastrectomy such as LADG and LATG, not only in Japan but also in Korea and other countries [5]. Advanced laparoscopic gastrectomy is believed to contribute to early postoperative recovery and better cosmesis [6]. However, patients’ quality of life (QOL) is mainly affected by late phase complications such as dumping syndrome and body weight loss resulting from oral intake disturbance. Attention should be paid to both minimal invasiveness for early phase recovery and satisfactory late phase function after gastric cancer surgery.
In Japan and Korea, where distal gastric cancer is the dominant type of gastric cancer observed, the incidence of proximal gastric cancer located in the upper third of the stomach is increasing, similar to Western countries [7, 8]. Total gastrectomy has been attempted in the past for proximal gastric cancer because of its radical nature and safety [9]. More recently, however, no significant difference has been reported between total gastrectomy and proximal gastrectomy in terms of postoperative survival of patients with early-stage proximal gastric cancer. Moreover, proximal gastrectomy has been recommended because of the physiological function of the remaining stomach compared with that after total gastrectomy [10–13].
Although function-preserving surgery, including proximal gastrectomy, with limited resection of the stomach and less lymph node dissection helps to improve functional postoperative results, a certain incidence of skip metastasis in the 2nd (or 3rd) compartment of regional lymph nodes remains an obstacle to the wider application of these procedures. To overcome these issues, the sentinel node (SN) concept has attracted attention and is anticipated to become a novel diagnostic tool for identification of clinically undetectable lymph node metastasis in patients with early-stage proximal gastric cancer.
A SN is defined as the lymph node first receiving lymphatic drainage from the primary site of a tumor [14], and is thought to be the first possible site of micrometastasis along the route of lymphatic drainage from the primary lesion. Thus the pathological status of SNs is thought to predict the status of all regional lymph nodes. If SNs are recognizable and negative for cancer metastasis, unnecessary radical lymph node dissection may be avoided. The SN hypothesis is applied to patients at high risk of lymph node metastasis based on the characteristics of their primary tumor, but having clinically undetectable regional metastatic nodes by preoperative diagnostic imaging. Sentinel node navigation surgery is defined as a novel, minimally invasive surgery avoiding unnecessary lymph node dissection based on SN mapping and diagnosis of nodal metastasis targeting SNs. We previously developed a radio-guided method for SN mapping in gastric cancer and reported the procedure for the first time [15–18]. Sentinel node navigation surgery can be applied to proximal gastrectomy for patients with early-stage upper-third gastric cancer.
Worldwide, laparoscopy-assisted proximal gastrectomy (LAPG) is still relatively uncommon because of certain technical difficulties [19, 20]. In particular, lymphadenectomy and reconstruction with LAPG, which are required for curative and safety reasons, have not been standardized for clinical application to date. We have recently established a novel LAPG procedure based on the SN concept and secure esophagogastric anastomosis, which uses a circular stapler and transoral placement of the anvil. Our LAPG procedure consists of three major stages: (1) optimization of the extent of lymphadenectomy based on SN mapping for curative resection, (2) easy and secure esophagogastric anastomosis using Orvil (Autosuture, Norwalk, CT) for placement of the anvil, and (3) antireflux surgery to prevent postoperative reflux esophagitis.
In the present study, we hypothesized that this new LAPG procedure for early-stage proximal gastric cancer would be useful in terms of curability, safety, and prevention of postoperative reflux esophagitis in clinical practice. This study demonstrates the results of our LAPG procedure in 37 patients with cT1N0M0 proximal gastric cancer.
Patients and methods
Patients
Between 2007 and 2010, we enrolled 37 consecutive patients at Keio University Hospital (Tokyo, Japan) who were preoperatively diagnosed with cT1N0M0 primary gastric cancer of the upper third of the stomach with a primary tumor diameter of less than 4 cm, in which approximately two thirds of the stomach could be preserved after proximal gastrectomy. All patients underwent proximal (or total) gastrectomy with SN mapping after signing an informed consent. Prior to treatment, patients were assessed via esophagogastrography, esophagogastroscopy, computed tomography, ultrasonography, and endoscopic ultrasonography. Clinical staging and pathological examination for resected specimens were performed according to the Japanese Classification of Gastric Cancer by the Japanese Gastric Cancer Association [21] and the TNM classification as proposed by the AJCC (American Joint Committee on Cancer). The Japanese classification scheme identifies lymph nodes by number, and that system is used to describe lymph node stations identified in this report. Preoperative endoscopic clipping was performed distal to the tumor as an indicator of tumor location.
SN mapping procedures
To detect SNs in proximal gastric cancer, we employed the dual tracer method using radioactive colloid and blue dye rather than the conventional blue dye only, as previously described [15, 16]. In brief, one day prior to surgery, 2.0 ml of technetium-99 m tin colloid solution (150 MBq) was injected at four quadrants into the submucosal layer around the primary tumor with an endoscopic puncture needle. Laparoscopic intraoperative SN detection was performed as follows [22]: blue dye (1% isosulfan blue or indocyanine green) was injected at the beginning of surgery using intraoperative endoscopy in the same manner as the preoperative injection of radioactive tracer. Blue-stained lymphatic vessels and nodes could be identified by laparoscopy within 15 min of dye injection. Simultaneously, a hand-held gamma probe was used to locate the radioactive SNs. Intraoperative gamma probing is feasible in laparoscopic gastrectomy using a gamma detector (GPS Navigator; RMD Instruments LLC, Watertown, MA), introducible via either a trocar port or a small incision. The nodes identified as SN as either blue-stained or radioactive in the resected specimens were carefully investigated using the gamma probe, and all SNs were sent for intraoperative pathological examination. After lymph node dissection, the absence of SNs in the abdominal cavity was carefully confirmed by the gamma probe through either the incisional wound or the laparoscopy ports.
Laparoscopy-assisted proximal gastrectomy
Laparoscopy-assisted proximal gastrectomy was performed with the patient in the open-leg position. A 12 mm port was inserted through the inferior of the umbilicus by the open method and the peritoneal cavity was inflated with 10 mmHg carbon dioxide. The placement of the surgical ports is shown in Fig. 1. The portion of the greater omentum from its middle to its left side was opened toward the spleen with ultrasonically activated coagulation shears (SonoSurg; Olympus Medical Systems, Tokyo, Japan) and a vessel-sealing system (LigaSure Blunt Tip; Valley Lab, Boulder, CO). The arcade of the right gastroepiploic artery was preserved. The left gastroepiploic artery and vein were clipped and divided, and No. 4sb lymph nodes were removed. The short gastric arteries and veins were divided and the dissection of lymph nodes Nos. 4sa and 2 was completed up to the gastroesophageal junction (GEJ).
The lesser sac was opened and the lymph nodes along the common hepatic artery (No. 8) and the proximal side of the splenic artery (No. 11p) were dissected. The left gastric vein and artery were clipped and divided, followed by dissection of the lymph nodes around the root of the left gastric artery and the celiac axis (Nos. 7 and 9). The right gastric artery was preserved in all cases. After resection of the posterior gastric artery, the abdominal esophagus was mobilized circumferentially. The anterior and posterior vagal nerves were not preserved in most cases. Finally, the abdominal esophagus was transected obliquely with the Endo GIA Universal (Autosuture) for the hemi-double stapling technique (DST) that we prefer for the creation of an esophagogastric anastomosis (Fig. 2a).
a The abdominal esophagus was transected obliquely using a 60 mm linear stapler. b The stomach was pulled out through the incisional wound. Intraoperative gamma probing was performed extracorporally to identify SNs. c Laparoscopic techniques for placement of the anvil. The orogastric tube was pulled through the esophagotomy incision. d Placement of the anvil was completed
Laparotomy was performed through a midline incision (4–5 cm) in the upper abdomen, and a small wound retractor was inserted. The stomach was pulled out through the incisional wound, and intraoperative gamma probing was performed extracorporally to confirm that SNs (radioactive or blue nodes) were not located in station Nos. 3b, 5, 12, 4d, or 6 (Fig. 2b). The appropriate line of the distal resection margin over the greater curvature was guided by the clip that had been placed preoperatively during endoscopy. After the vessels of the greater and lesser curvatures were divided, the gastric body was extracorporally transected with a linear stapler. Oblique transection of the stomach to marginally extend the greater curvature more than the lesser curvature is preferred for antireflux surgery after esophagogastric anastomosis. The staple line of the residual stomach was closed with 3-0 silk or Vicryl (Ethicon, Inc., Somerville, NJ). All SNs identified in the resected specimen were sent for intraoperative pathological examination. If these were positive for macrometastasis on intraoperative pathological diagnosis, LAPG was converted to LATG for more radical lymphadenectomy. After gastrectomy and lymph node dissection, the absence of SNs, especially at station Nos. 10 and 11d, was carefully confirmed by gamma probe, via either the incisional wound or the laparoscopic ports. The arcades of the right gastroepiploic artery and right gastric artery were essentially preserved. At a minimum, D1 + dissection (removal of station Nos. 1, 2, 3a, 4sa, 4sb, 7, 8, 9, 11p, and part of Nos. 3b and 4d) under the Gastric Cancer Treatment Guidelines 2010 of the Japanese Gastric Cancer Association [23] was performed in all cases.
Esophagogastric anastomosis with the circular stapler
The circular stapling technique was employed for esophagogastric anastomosis after proximal gastrectomy. Orvil, the orogastric tube with the attached pretilted anvil head, was passed transorally by an assistant in the conventional manner. A small esophagotomy was performed to the right of the staple line of the esophageal stump, which was at a relatively acute angle to the stump following oblique transection of the esophagus (Fig. 2a, c). The orogastric tube was drawn through the esophagotomy by the surgical operator and withdrawn through a trocar until the anvil was positioned within the end of the esophageal stump (Fig. 2c). After the suture attaching the anvil to the orogastric tube was cut and the orogastric tube was separated from the anvil, placement of the anvil for connection to the 25 mm circular stapler was accomplished (Fig. 2d).
A small incision (3 cm) was made in the anterior wall of the antrum of the residual stomach. The shaft of a 25 mm circular stapler (EEA 25-3.5 XL Circular Stapler; Autosuture) was inserted and placed extracorporally within the residual stomach from the gastrotomy in preparation for reconstruction of the esophagogastric anastomosis. The trocar of the circular stapler was extended to penetrate the anastomotic portion on the anterior wall 2.5 cm from the transected line of the stomach. After re-establishment of pneumoperitoneum with a plastic glove covering the wound retractor to maintain airtightness, the trocar was intracorporally connected to the anvil placed in the esophagus, and circular stapling was performed in the conventional way, thus completing the esophagogastric anastomosis (Fig. 3a, b). The access opening on the anterior antral wall was closed either with conventional sutures or with the laparoscopic linear stapler (Fig. 4a). Pyloroplasty was not performed routinely and, if needed, postoperative balloon dilatation of the pylorus was performed by gastroendoscopy in selected cases.
a Reconstruction of the esophagogastric anastomosis. The anastomotic portion was on the anterior wall 2.5 cm from the transected line of the stomach. The access opening on the anterior antral wall was closed by either conventional sutures or the laparoscopic linear stapler. b Laparoscopic subtotal wrapping of the abdominal esophagus by the residual stomach as antireflux surgery
Antireflux surgery
We recommend antireflux surgery to prevent postoperative reflux esophagitis following LAPG. Subtotal wrap of the abdominal esophagus by the residual stomach, similar to Toupet fundoplication, is preferred for efficient antireflux surgery after LAPG (Fig. 4b). In short, the greater curvature of the gastric stump was hand-sutured to the left wall of the abdominal esophagus intracorporally, and also to the diaphragmatic hiatus. Next, the lesser curvature of the gastric stump was sutured to the right wall of the abdominal esophagus and the diaphragmatic hiatus in the same manner (Fig. 5a). Finally, intraoperative gastroendoscopy was performed to ensure successful completion of esophagogasrostomy with no anastomotic leaks, and fundoplication.
Results
Laparoscopy-assisted proximal gastrectomy was planned for 37 patients (28 male and 9 female; median age: 64 years; age range: 27–81 years) (Table 1) but was completed in only 36. The procedure in the other patient was intraoperatively converted to LATG because one SN detected was positive for metastasis by intraoperative pathological diagnosis (Table 2). The mean operating time for the 36 LAPG patients was 271 ± 65 min, and mean blood loss was 26 ± 37 ml. There were no intraoperative complications or conversions to open surgery from laparoscopic surgery in any patient.
Patients who had undergone LAPG generally took sips of water 4 days after surgery and began a semifluid diet at 6 days after surgery; median duration of hospital stay for the 36 LAPG patients was 13 days. There were no severe postoperative complications, such as hemorrhage, anastomotic leak, pancreatic fistula, intra-abdominal abscess, or incisional wound infection in any patient. Postoperatively, five patients (14%) experienced mild temporary anastomotic stenosis, which was successfully treated by endoscopic balloon dilation in the outpatient clinic. Food was relatively well tolerated by all patients, and postoperatively, most patients did not experience severe reflux symptoms or a significant degree of reflux esophagitis by endoscopic examination (Fig. 5b, c). Immediately after surgery, only one patient (3%) complained of mild reflux symptoms, which were graded endoscopically as B according to the Los Angeles Classification of gastroesophageal reflux disease (GERD), but they were well controlled by the use of a proton-pump inhibitor. All patients have been free from cancer recurrence for a median follow-up period of 26 months.
In this study, SNs were detected successfully in 37 (100%) patients. The mean number of dissected lymph nodes and identified SNs per case were 29.4 and 5.8, respectively. Three patients with lymph node metastasis showed positive SNs by pathological diagnosis. One case with lymph node metastasis showed evidently positive SN by intraoperative pathological diagnosis and the other two were negative by intraoperative pathological diagnosis. However, these two cases showed the presence of isolated tumor cells (ITCs) in SNs, which were postoperatively diagnosed by immunohistochemistry with cytokeratin antibodies. Sensitivity in predicting nodal metastasis, including ITCs, and diagnostic accuracy based on SN status were 100% (3/3) and 100% (37/37), respectively.
The location of identified SNs was analyzed in all 37 patients (Table 3). Most SNs were located in the lesser curvature area, such as at station Nos. 3a (76%), 1 (59%), and 7 (32%). In particular, when the primary tumor was located at the lesser curvature, SNs were usually identified only in that area. However, when the primary tumor was located at other sites, such as the anterior wall, posterior wall, or greater curvature, SNs were identified at the greater curvature, such as at station Nos. 2, 4sa, and 4sb. No SNs were identified at station Nos. 5, 6, 10, and 11d. Only one patient showed an SN (No. 3a) that was positive for macrometastasis (2 mm) by intraoperative pathological diagnosis; this patient therefore underwent LATG rather than LAPG, which allows for a more radical lymphadenectomy. This patient showed no metastasis in other regional lymph nodes.
Discussion
In this study, we report the development of a novel LAPG procedure with SN mapping and esophagogastric anastomosis, which uses a circular stapler with transoral placement of the anvil. The LAPG procedure was completed in 36 patients, and LATG rather than LAPG was performed in one patient because he showed SNs positive for cancer metastasis by intraoperative pathological diagnosis. There were no intraoperative complications or conversion to open surgery from laparoscopic surgery in any patient. There were no severe postoperative complications, including anastomotic leaks. All patients have been free from recurrence for a median follow-up period of 26 months.
Laparoscopy-assisted proximal gastrectomy is known to involve certain technical difficulties in terms of curability and safety, compared with LADG or LATG [19, 20]. First, the extent of regional lymphadenectomy in LAPG has to be optimized to avoid postoperative lymph node recurrence. The incidence of lymph node metastasis in early gastric cancer at the proximal third of the stomach is not high [24], and nodal metastasis does not usually involve lymph node station Nos. 3b, 5, 6, 4d, or 12 [25]. However, it is crucial to confirm that nodal metastasis is not present in these nondissected nodes during LAPG. In this regard, we believe that intraoperative SN mapping and sentinel lymphadenectomy can provide efficient and accurate diagnosis of lymph node metastasis for unexpected stations in patients with early cT1N0M0 gastric cancer. We have established a standard protocol of SN mapping for gastric cancer on the basis of previous experience [22, 26]. The dual tracer method using radioactive colloid and blue dye is feasible and represents the most reliable current method for the stable detection of SNs in early gastric cancer [16, 26]. Radio-guided methods allow identification of SNs even in resected specimens and to confirm the total harvesting of SN by gamma probing, and blue dye is effective for intraoperative real-time visualization of lymphatic flows even in laparoscopic surgery [22].
In addition to the present study, we have reported SN mapping for 378 patients with early gastric cancer and verified the accuracy of this procedure [27]. According to current thinking, however, patients with cT1N0M0 gastric cancer of the upper third of the stomach should undergo LAPG with, at a minimum, D1 + dissection according to the Japanese Guidelines for assurance of curability, even if SNs are negative for metastasis by intraoperative pathological diagnosis. Moreover, if SNs are positive for macrometastasis, patients should be treated by standard D2 dissection, which means conversion to LATG from LAPG. In fact, the patient with a positive SN in this study showed no metastasis in other regional lymph nodes. However, we have no useful tools with which to predict the number and the location of all metastatic lymph nodes intraoperatively in patients with positive SNs. Therefore we chose LATG as a more radical and curative lymphadenectomy for our patient with positive SNs. Further studies will be needed to verify the appropriate approach to lymphadenectomy for patients with positive SNs.
In addition, we consider that intraoperative SN mapping and sentinel lymphadenectomy are reliable and adaptable to Siewert type II cT1N0M0 adenocarcinoma of the GEJ. If SNs are identified only in the abdominal area and are pathologically negative in cT1N0M0 adenocarcionoma of GEJ, the patient would be treated by limited resection of the abdominal esophagus and proximal gastrectomy by the laparoscopic approach, without extensive mediastinal lymph node dissection [28].
In the present study, SNs were identified only at the lesser curvature when the primary tumor was located at this site. However, when the primary tumor was located at another site, such as the anterior wall, posterior wall, or greater curvature, SNs were identified at the greater curvature in some patients. In no case were SNs identified at station Nos. 5, 6, 10, 11d, or 12. In only one patient was a SN (No. 3a) identified as positive for macrometastasis by intraoperative pathological diagnosis. After this diagnosis, it was decided to use LATG, which allows for a more radical lymphadenectomy than LAPG. No patient in our series has evidence of tumor recurrence postoperatively, which suggests that SN mapping and biopsy may enable the performance of not only individualized and minimally invasive surgery that could maintain patients’ QOL, but also appropriate and curable lymphadenectomy for patients with cT1N0M0 proximal gastric cancer.
Reconstruction after LAPG must be technically safe and easy to perform. Although various reconstruction procedures following proximal gastrectomy in open surgery have been attempted to date, the optimum method remains to be determined [11, 29–35]. Interposition of the jejunum is known to involve less morbidity in terms of severe reflex esophagitis compared with direct esophagogastric anastomosis; however, this procedure can prove very complicated technically, especially in laparoscopic surgery. Another approach, esophagogastric anastomosis, is a simple technique that is applicable to laparoscopic surgery if postoperative reflex esophagitis can be avoided. In the present study, therefore, we developed esophagogastric anastomotic methods in which the circular stapler was used with Orvil for easy and secure anastomotic reconstruction, after which we performed antireflux surgery to prevent postoperative reflux esophagitis.
Most gastrointestinal surgeons are familiar with the circular stapler for reconstruction after gastrectomy in open surgery. However, placement of the anvil in the esophageal stump seems to be a major technical concern when the circular stapler is used in laparoscopic surgery. Recently, Orvil was developed specifically for the purpose of transoral delivery of the anvil head. The pretilted anvil head enables easy passage through the hypopharynx and upper esophageal sphincter during transoral delivery. Orvil was originally developed for laparoscopic Roux-en-Y gastric bypass to simplify reconstruction in gastrojejunostomy. More recently, Nguyen et al. [36] reported their clinical experiences using Orvil for transoral placement of the anvil in preparation for circular stapling in esophagogastrostomy during thoracoscopic Ivor Lewis esophagogastrectomy. We applied these techniques to esophagogastric anastomosis during LAPG. In our experience, although some mechanical maneuvers such as extension of the patient’s neck and deflation of the endotracheal tube balloon were necessary to facilitate transoral delivery of the anvil head, this was successfully accomplished using Orvil in all patients without any complications or esophageal injury. There was a learning curve involved in reducing operative time associated with transoral delivery of the anvil head, but only a few minutes were required for this stage of the procedure for the final 20 patients.
Laparoscopic antireflux surgery is known to be a safe, effective, and feasible procedure. To date, we have performed laparoscopic Toupet or Nissen fundoplication in more than 50 patients with GERD [37]. In general, after proximal gastrectomy a larger residual stomach is desirable to prevent the postoperative reflux symptoms related to the esophagogastric anastomosis. Moreover, in the present study, subtotal wrap of the abdominal esophagus with the residual stomach, similar to Toupet fundoplication, was performed for the purpose of preventing reflux esophagitis after LAPG [20], which was controlled well by fundoplication. However, we believe that further studies will be needed to verify the retention of postoperative patients’ QOL, which should be evaluated more precisely in the long term by several scales such as the Gastrointestinal Symptom Rating Scale [38] and the GERD Health-Related Quality of Life [39].
In conclusion, novel LAPG with SN mapping and esophagogastric anastomosis using a circular stapler with transoral placement of the anvil proved to be curative and safe procedures involving minimally invasive surgery for patients with upper-third early-stage gastric cancer. Associated morbidity, including postoperative reflux esophagitis, was minimal. Although further study will be needed for validation, this novel surgical procedure is feasible and reliable for the treatment of early cT1N0M0 proximal gastric cancer.
References
Sano T, Hollowood K (2006) Early gastric cancer: diagnosis and less invasive treatments. Scand J Surg 95:249–255
Kitano S, Iso Y, Moriyama M et al (1994) Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 4:146–148
Adachi Y, Shiraishi N, Shiromizu A et al (2000) Laparoscopy-assisted Billroth I gastrectomy compared with conventional open gastrectomy. Arch Surg 135:806–810
Shinohara T, Kanaya S, Taniguchi K et al (2009) Laparoscopic total gastrectomy with D2 lymph node dissection for gastric cancer. Arch Surg 144:1138–1142
Hur H, Jeon HM, Kim W (2008) Laparoscopy-assisted distal gastrectomy with D2 lymphadenectomy for T2b advanced gastric cancers: three years’ experience. J Surg Oncol 98:515–519
Kim YW, Baik YH, Yun YH et al (2008) Improved quality of life outcomes after laparoscopy-assisted distal gastrectomy for early gastric cancer: results of a prospective randomized clinical trial. Ann Surg 248:721–727
Powell J, McConkey CC (1990) Increasing incidence of adenocarcinoma of the gastric cardia and adjacent sites. Br J Cancer 62:440–443
Blot WJ, Devesa SS, Kneller RW et al (1991) Rising incidence of adenocarcinoma of the esophagus and gastric cardia. JAMA 265:1287–1289
Papachristou DN, Fortner JG (1996) Adenocarcinoma of the gastric cardia: the choice of gastrectomy. Ann Surg 192:58–64
Harrison LE, Karpeh MS, Brennan MF (1998) Total gastrectomy is not necessary for proximal gastric cancer. Surgery 123:127–130
Adachi Y, Inoue T, Hagino Y et al (1999) Surgical results of proximal gastrectomy for early-stage gastric cancer: jejunal interposition and gastric tube reconstruction. Gastric Cancer 2:40–50
Shiraishi N, Adachi Y, Kitano S et al (2002) Clinical outcome of proximal versus total gastrectomy for proximal gastric cancer. World J Surg 26:1150–1154
Katai H, Sano T, Fukagawa T et al (2003) Prospective study of proximal gastrectomy for early gastric cancer in the upper third of the stomach. Br J Surg 90:850–853
Morton DL, Wen DR, Wong JH et al (1992) Techinical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg 127:392–399
Kitagawa Y, Fujii H, Mukai M et al (2000) The role of the sentinel lymph node in gastrointestinal cancer. Surg Clin North Am 80:1799–1809
Kitagawa Y, Kitano S, Kubota T et al (2005) Minimally invasive surgery for gastric cancer—toward a confluence of two major streams: a review. Gastric Cancer 8:103–110
Kitagawa Y, Fujii H, Kumai K et al (2005) Recent advances in sentinel node navigation for gastric cancer: a paradigm shift of surgical management. J Surg Oncol 90:147–152
Kitagawa Y, Kitajima M (2006) Diagnostic validity of radio-guided sentinel node mapping for gastric cancer—a review of current status and future direction. Surg Technol Int 15:32–36
Aihara R, Mochiki E, Ohno T et al (2010) Laparoscopy-assisted proximal gastrectomy with gastric tube reconstruction for early gastric cancer. Surg Endosc 24:2343–2348
Sakuramoto S, Yamashita K, Kikuchi S et al (2009) Clinical experience of laparoscopy-assisted proximal gastrectomy with Toupet-like partial fundoplication in early gastric cancer for preventing reflux esophagitis. J Am Coll Surg 209:344–351
Japanese Gastric Cancer Association (2010) Japanese classification of gastric cancer, 14th edn. Kanehara Publishing Co, Tokyo
Saikawa Y, Otani Y, Kitagawa Y et al (2006) Interim results of sentinel node biopsy during laparoscopic gastrectomy: possible role in function-preserving surgery for early cancer. World J Surg 30:1962–1968
Japanese Gastric Cancer Association (2010) Gastric cancer treatment guidelines, 3rd edn. Kanehara Publishing Co, Tokyo
Kurihara N, Kubota T, Otani Y et al (1998) Lymph node metastasis of early gastric cancer with submucosal invasion. Br J Surg 85:835–839
Kong SH, Kim JW, Lee HJ et al (2010) Reverse double-stapling end-to-end esophagogastrostomy in proximal gastrectomy. Dig Surg 27:170–174
Takeuchi H, Saikawa Y, Kitagawa Y (2009) Laparoscopic sentinel node navigation surgery for early gastric cancer. Asian J Endosc Surg 2:13–17
Kitagawa Y, Saikawa Y, Takeuchi H (2006) Sentinel node navigation in early stage gastric cancer—updated data and current status. Scand J Surg 95:256–259
Burian M, Stein HJ, Sendler A (2004) Sentinel node detection in Barrett’s and cardia cancer. Ann Surg Oncol 3:255S–258S
Oka M, Yamamoto K, Nakamura M et al (1998) Reconstruction after proximal gastrectomy using a stapled, U-shaped jejunal pouch. J Am Coll Surg 186:601–603
Uyama I, Sugioka A, Fujita J et al (2000) Completely laparoscopic proximal gastrectomy with jejunal interposition and lymphadenectomy. J Am Coll Surg 191:114–119
Takeshita K, Saito N, Saeki I et al (1997) Proximal gastrectomy and jejunal pouch interposition for the treatment of early cancer in the upper third of the stomach: surgical techniques and evaluation of postoperative function. Surgery 121:278–286
Yoo CH, Sohn BH, Han WK et al (2005) Proximal gastrectomy reconstructed by jejunal pouch interposition for upper third gastric cancer: prospective randomized study. World J Surg 29:1592–1599
Uyama I, Sugioka A, Matsui H et al (2001) Laparoscopic side-to-side esophagogastrostomy using a linear stapler after proximal gastrectomy. Gastric Cancer 4:98–102
Tonouchi H, Mohri Y, Tanaka K et al (2006) Hemidouble stapling for esophagogastrostomy during laparoscopically assisted proximal gastrectomy. Surg Laparosc Endosc Percutan Tech 16:242–244
Hiki N, Fukunaga T, Yamaguchi T et al (2007) Laparoscopic esophagogastric circular stapled anastomosis: a modified technique to protect the esophagus. Gastric Cancer 10:181–186
Nguyen TN, Hinojosa MW, Smith BR et al (2008) Thoracoscopic construction of an intrathoracic esophagogastric anastomosis using a circular stapler: transoral placement of the anvil. Ann Thorac Surg 86:989–992
Irino T, Takeuchi H, Ozawa S et al (2010) Age and body mass index: significant predictive factors for successful laparoscopic antireflux surgery. Surg Today 40:1137–1143
Svedlund J, Sjodin I, Dotevall G (1988) GSRS-a clinical rating score for gastrointestinal symptoms in patients with irritable bowel syndrome and peptic ulcer disease. Dig Dis Sci 33:129–134
Velanovich V (1998) Comparison of generic (SF-36) vs. disease-specific (GERD-HRQL) quality-of-life scales for gastroesophageal reflux disease. J Gastrointest Surg 2:141–145
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takeuchi, H., Oyama, T., Kamiya, S. et al. Laparoscopy-assisted Proximal Gastrectomy with Sentinel Node Mapping for Early Gastric Cancer. World J Surg 35, 2463–2471 (2011). https://doi.org/10.1007/s00268-011-1223-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-011-1223-3