Abstract
Background
Two nomograms are available for predicting patient survival after hepatic resection for metastatic colorectal cancer (CRC). However, they have not been externally validated using other databases, and so their universal applicability has not been established. We aimed to examine the validity of these nomograms for predicting patient survival after hepatic resection for metastatic CRC in different institutions.
Methods
We analyzed the cases of 113 patients who underwent hepatic resection for metastatic CRC at Hiroshima University Hospital between 1995 and 2006. In this patient set, we assessed the predictive value of the Kattan nomogram of the Memorial Sloan-Kettering Cancer Center (MSKCC) (United States) and the Kanemitsu nomogram from the Aichi Cancer Center (Japan). The concordance index was used as an accuracy measure for comparing these two nomograms. The predictive accuracy of these nomograms was compared with that of conventional predictive models.
Results
The 3-, 5-, and 10-year overall survival rates in our cohort were 66.3%, 52.4%, and 42.7%, respectively. The concordance indexes of the pre- and postoperative Kanemitsu nomogram and that of the Kattan nomogram were 0.70, 0.69, and 0.68, respectively. These values were higher than those obtained using other models for hepatic metastatic CRC, including the clinical risk score of the MSKCC and the grading system of the Japanese Society for Cancer of the Colon and Rectum.
Conclusions
The high predictive accuracy of both nomograms shows that these predictive tools can be used in different institutions. Patient counseling and adjuvant therapy decision-making should benefit from use of these nomograms.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Liver metastases from colorectal cancer are classified as stage IV according to the tumor-node-metastasis (TNM) system. It has become clear, however, that the risk of recurrence and death, particularly after hepatectomy, is not the same in all patients with colorectal liver metastasis (CLM).
Surgical resection is the essential step in curative treatment for CLM. Recently, perioperative chemotherapy for CLM has become a matter of discussion [1, 2]. Because the characteristics of patients with CLM greatly vary, in future studies on perioperative chemotherapy for CLM the patients should be stratified on the basis of the predicted individual risk to enable selection of patients who can benefit most from perioperative chemotherapy.
To assess patient risk and to aid in patient care, many investigators have attempted to develop prognostic scoring systems for predicting the outcome of patients with CLM [3–7]. All of these scoring systems were based on several clinical factors, but the factors differed among systems. These variations have resulted in conflicting outcome predictions, with the result that there is no consensus on which system is the most reliable in the clinical setting.
The clinical risk score (CRS) proposed by Fong et al. [4] is widely known, and it has been validated using other independent databases [8–10]. In Japan, the grading system developed by the Japanese Research Society for Cancer of the Colon and Rectum—the Japanese grading system (JGS) [11]—is most widely used.
The nomogram, a statistical predictive model that has been developed in recent years, can be applied to most cancer types, including soft tissue sarcoma [12], gastric carcinoma [13], pancreatic carcinoma [14], prostate carcinoma [15–18], renal cell carcinoma [19], and breast carcinoma [20]. The nomogram generates a simple graphic representation of the predictive model that calculates the numeric probability of a clinical event and enables clinicians to calculate an overall risk score that reflects the risk for individual patients.
Recently, two nomograms for predicting patient survival after hepatic resection for metastatic colorectal cancer (CRC) were developed. One, developed by Kattan et al., predicts the 96-month disease-specific survival after hepatic resection for metastatic CRC by quantitating 10 clinical variables [21]. The basis for this nomogram was a statistical model derived from a study on 1477 patients treated at the Memorial Sloan-Kettering Cancer Center (MSKCC). The other effort, by Kanemitsu et al., was based on a study on 578 patients treated at 18 major Japanese medical centers [22]. Kanemitsu et al. developed two nomograms—a preoperative one and postoperative one. The peroperative nomogram was designed to predict the probability of the 3-year overall survival of individual patients after curative resection of CLMs by quantitating five clinical variables. The postoperative nomogram was designed to predict 5-year disease-specific survival by quantitating six clinical variables.
The purposes of this study were to assess the validity of the above-mentioned nomograms for patients with CLM in different institutions and to compare the predictive accuracy of these nomograms with that of the CRS and the JGS.
Material and methods
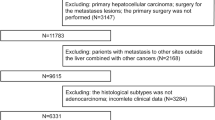
Patients
Between 1995 and 2006, a total of 120 patients underwent initial hepatic resection for CLM at Hiroshima University Hospital, Hiroshima, Japan. For seven patients, the resections were not radical because of gross residual disease within or outside the liver. The remaining 113 patients, who underwent curative hepatic resection, were included in this study.
Preoperative evaluation of CLM was performed using both conventional computed tomography (CT) and magnetic resonance imaging (MRI). 18F-Fluorodeoxyglucose positron emission tomography (FDG-PET) scanning was used to evaluate suspected hilar lymph nodes and extrahepatic disease, if necessary. Liver function was assessed using the indocyanine green retention rate at 15 minutes (ICGR15). All resected specimens were pathologically confirmed to be CLM by the pathology division in the hospital.
The primary CRC was treated by curative resection in all patients. The indications for hepatic resection of CLM were as follows: (1) completely resectable CLM diagnosed by preoperative imaging; (2) ability of the patient to tolerate the required surgical procedure (evaluated using pulmonary function tests, electrocardiography, and echocardiography) and to maintain the remaining hepatic function; (3) surgically controllable extrahepatic disease, including the primary lesion. Potentially resectable bilateral or multiple lesions were not excluded from the selection criteria.
Principally, partial hepatectomy with a tumor-free surgical margin was the procedure of choice, and we attempted to preserve as much of the normal hepatic parenchyma as possible. Hilar lymph node dissection was not performed unless obvious positive findings were observed on the preoperative CT scan or during the operation.
The routine follow-up protocol for both primary colorectal resection and hepatic metastasectomy comprised serum carcinoembryonic antigen (CEA) measurement and chest and abdominal CT scans. The serum CEA level was measured every 2–3 months during the first year after surgery, every 3–6 months for 2–5 years after that, and every 6–12 months thereafter. Chest and abdominal CT scans were obtained every 3–6 months for the first year after surgery, every 6–12 months for 2–5 years after that, and once a year thereafter. Additional CT scans were considered when the serum CEA level increased to above the normal range during follow-up. After 2003, FDG-PET scanning was performed to evaluate any suspected metastases that were observed on CT scans.
All patients were retrospectively analyzed with regard to age at hepatectomy and sex; primary tumor location; histology, depth, and number of positive lymph nodes; lobar distribution of the hepatic lesions; size and number of hepatic tumors; presence or absence of extrahepatic disease before or at hepatic metastasectomy; CEA level before hepatectomy; the interval between resection of the primary colorectal tumor and hepatic resection (disease-free interval). The number of metastatic lesions was evaluated using preoperative CT, MRI, and intraoperative ultrasonography (US). When multiple metastases were present, the largest diameter observed was recorded.
Kattan nomogram
The nomogram developed by Kattan et al. (Fig. 1) [21] predicts the survival of patients with CLM using the following clinical factors.
Nomogram for predicting 96-month disease-specific survival after hepatic resection for metastatic colorectal cancer. CEA carcinoembryonic antigen, Preop preoperative, Num. number, Met. metastasis, Mo. month, DSS disease-specific survival (adapted from Kattan et al. [21], with permission from the Annals of Surgery)
-
1.
Nodal status of the primary tumor
-
2.
Disease-free interval
-
3.
Size of the largest metastatic tumor
-
4.
Preoperative CEA level
-
5.
Bilateral resection
-
6.
Extensive resection (lobectomy or more)
-
7.
Sex
-
8.
Number of hepatic tumors
-
9.
Primary cancer site (colon vs. rectum)
-
10.
Age
Kanemitsu nomogram
The nomogram developed by Kanemitsu et al. (Fig. 2) [22] predicts the survival of patients with CLM using the following clinical factors. The details are as follows.
Preoperative (a) and postoperative (b) nomograms for estimating the survival of patients with colorectal liver metastases treated with hepatectomy. *Well, moderately, or mucinous or poorly differentiated tumors (with permission, World Journal of Surgery) (adapted from Kanemitsu et al. [22], p. 1104 [figure 2 and figure3])
Preoperative nomogram
-
1.
Primary histology
-
2.
Number of metastatic lymph nodes of the primary lesion
-
3.
Number of hepatic tumors
-
4.
Extrahepatic disease
-
5.
Preoperative CEA level (ng/ml)
Postoperative nomogram
-
1.
Primary histology
-
2.
Number of metastatic lymph nodes of primary lesion
-
3.
Metastasis of hilar lymph nodes
-
4.
Surgical margin
-
5.
Extrahepatic disease
-
6.
Preoperative CEA level (ng/ml)
To use the nomograms, read the points assigned for each predictor on a scale of 0–100 and add these points. Locate this value on the “total points” axis with a vertical ruler and run the ruler down to read the predicted values of interest.
Statistical analysis
Nomogram validation comprised two activities. First, discrimination of the nomogram was quantified using the concordance index (c-index). The c-index is similar to the area under the receiver operating characteristic curve (AUC), but it is appropriate for censored data. The c-index reflects the probability that for a randomly selected pair of patients in which one patient dies before the other the patient who died first had the worse predicted outcome from the nomogram. The c-index of the nomograms was compared to that of other prognostic scoring systems.
Second, the calibration was assessed. Calibration compares the predicted probability of overall survival with the actual survival. This was performed plotting the Kaplan–Meier curves for survival, stratified by nomogram prediction. The patients were categorized into quadrants of nomogram-derived risk (e.g., 0–25%, 25–50%, 50–75%, 75–100%). All analyses were performed using S-Plus 2000 professional software (Statistical Sciences, Seattle, WA, USA) with the Design and Hmisc libraries added.
Results
Patient demographics
The patient demographics are shown in Table 1. The study population comprised 69 (61.1%) men and 44 (38.9%) women. The median age of all the patients was 62 years (range 38–87 years). All 113 patients underwent macroscopically complete resection for CLM. The primary tumor was located in the colon in 67 patients (59.3%) and in the rectum in 46 patients (40.7%). Liver metastases were present at the time of diagnosis of the primary tumor in 57 patients (50.4%), whereas 56 patients (49.6%) had metachronous hepatic lesions. The median disease-free interval of the metachronous patients was 20 months (range 3–198 months). Lymph node involvement resulting from the primary tumor was present in 73 patients (64.6%), and the median number of positive lymph nodes was 1 (range 0–24). In all, 65 (57.5%) patients had a solitary CLM and 48 (42.5%) had multiple CLMs (range 2–10). The median diameter of the liver metastases was 3.3 cm (range 0.8–15.0 cm). A total of 11 patients (9.8%) had extrahepatic disease, and 15 patients (13.3%) underwent repeat hepatic resection.
Survival
The median follow-up interval after initial hepatic resection was 41.5 months (range 9–196 months). The cumulative 1-, 3-, 5-, and 10-year disease-specific survival rates in the cohort were 92.8%, 66.3%, 52.4%, and 42.7%, respectively (Fig. 3). The median survival period of all patients was 60.5 months.
Evaluation of the predictive accuracy of the two nomograms
The c-index for the Kattan nomogram was 0.68 in this study (the c-index with the original cohort was 0.61 [21]). The c-indexes for the preoperative and postoperative Kanemitsu nomograms were 0.70 and 0.69, respectively (c-indexes with the original cohort for the preoperative and postoperative nomograms were 0.66 and 0.69, respectively [22]). This means that in 68% to 70% of cases these nomograms correctly predicted the ordering of the outcome between two randomly selected patients.
To compare the nomograms to previous models, we compared the predictive accuracy of two nomograms with that of the JGS and CRS. We found that the accuracy of the nomograms were superior to that of JGS (c-index 0.54) and CRS (c-index 0.62).
The difference is difficult to appreciate clinically. The survival of patients, stratified by quartiles of nomogram-predicted median survival times, are depicted in Fig. 4; and the survival curve of patients, stratified by the JGS and CRS, are depicted in Fig. 5. Figure 4 indicates that the quartiles of median survival predictions by the Kanemitsu preoperative nomogram (A) and the Kattan nomogram (B) were associated with different observed periods of survival (p < 0.001). Furthermore, these graphs showed that the nomograms had better discriminating ability of survival than the JGS or the CRS (Fig. 5). Also, the Kanemitsu nomogram (preoperative) had slightly better discriminating ability of survival than the Kattan nomogram, although the p values for both were appreciably small.
Survival curves for patients stratified by a the Japanese grading system (JGS) and b the clinical risk score (CRS). a Grade A: HT1 with pN0/1; grade B: HT2 with pN0/1 or HT1 with pN2; grade C: HT2 with pN2, HT3 with any pN, or any HT and any pN with extrahepatic metastases. HT1: CLMs <4 lesions and <5 cm; HT2: CLMs except for HT1 and HT3; HT3: CLMs >5 lesions and >5 cm. b The CRS was calculated by counting the following criteria: (1) positive nodal status of the primary lesion; (2) disease-free interval from the primary lesion to discovery of liver metastases of <12 months; (3) number of hepatic metastases >1; (4) size of the largest hepatic metastases >5 cm; (5) preoperative CEA level >200 ng/ml
Discussion
The liver is the most common site of distant metastases from CRC. Resection remains the only curative strategy for patients with CLM, resulting in longer survival than in patients treated with palliative chemotherapy [23]. In this study, the overall 5-year survival rate was 52.4%, which can be positively compared with data in the literature, where it ranges from 15% to 67% (reviewed by Simmonds et al. [24]).
More than half of the patients who undergo hepatectomy for CLM die within 5 years. Therefore, it is important to assess an individual patient’s risk of disease recurrence. Also, there is a need to prolong patient survival by using chemotherapy.
The ability to stratify the prognosis of patients preoperatively would have the following benefits: (1) it would increase the information available to patients when obtaining their informed consent; (2) it would enable assessment of the need for perioperative chemotherapy, (3) and it would facilitate comparative studies and clinical trials.
Several clinical scoring systems have been developed to predict the prognosis of individual patients more accurately [3–7]. All of these systems estimate the risk of cancer recurrence and patient prognosis by counting individual risk factors. These methods for calculating clinical risk are simple and convenient, but they do pose some problems. With these simple scoring systems, counting various risk factors implies that each factors carries equal weight. Counting the risk factors requires that continuous variables (e.g., CEA level, number of hepatic tumors) be converted to discrete variables. This conversion would result in a considerable loss of information. For example, many authors include “the number of metastatic hepatic tumors” as a prognostic factor—i.e., as “solitary or multiple hepatic tumors.” In such scoring systems, patients who have 2 metastatic hepatic tumors and those who have 10 metastatic hepatic tumors are both classified as having “multiple hepatic tumors.” In the clinical setting, however, it is obvious that the risks for these two patients are not the same. Nomograms could solve these problems and enable a more precise assessment.
Our study validates the predictive value of two nomograms, one of which has been previously tested in multiple Japanese institutions and the other in an American single institution. External validation of published nomograms is important because it must be determined whether the predictive accuracy reported in the original study can be expected elsewhere. Thus far, there are no reports of external validation of these two available nomograms for patients with CLM.
In this study, an increasing nomogram score was shown to be associated with poor survival. Although the calibration graph was difficult to depict because of the small sample size, the actual overall survival of the patients in this study could be stratified into four risk groups on the basis of the predicted survival when using the nomogram. Thus, these nomograms can help identify the beneficiaries of the therapy before surgery.
In our study, the Kanemitsu nomograms (both preoperative and postoperative) appeared to have better predictive ability than the Kattan nomogram. This result may be attributed to race-related differences, as the Kanemitsu nomogram was developed in Japanese patients, and our cohort also comprised Japanese patients. Conversely, although the Kanemitsu nomogram had a slightly higher c-index (0.70 and 0.69 for the preoperative and postoperative nomograms, respectively), the Kattan nomogram had a satisfactorily high c-index (0.68). Hence, the Kattan nomogram is useful and can be used for non-American patients.
As far as Japanese patients are concerned, the Kanemitsu nomogram was more useful and convenient because it could predict patient survival using only five or six variables, whereas the Kattan nomogram requires 10 variables to predict patient survival; thus, the latter is more complex for use in clinical settings. However, both nomograms provided better predictive ability than the conventional prognostic models—CRS and JGS. The nomograms comprise a more sensitive assessment tool, allowing more careful evaluation.
The ability to provide the patient with a realistic estimation of his or her life expectancy after hepatectomy improves the effectiveness of patient counseling. The expected prognosis has a great impact on the kind of treatment a patient receives.
Although the nomogram seems useful for predicting patient risk in the clinical setting, it has some limitations. First, both nomograms can be applied only to patients who undergo initial hepatic resection for CLM. Currently, repeat hepatic resection is increasingly performed for recurrent CLM and greatly affects patient survival [25]. Neither nomogram could predict the prognosis of patients who undergo repeat hepatic resection.
Second, even after using a nomogram, it was difficult to determine which patients would benefit from perioperative chemotherapy. Patients who have unresectable colorectal metastases and are treated using the latest multidrug systemic chemotherapy are reported to have a median survival period of approximately 2 years [26]. Therefore, perioperative chemotherapy may be considered a treatment option if nomogram-predicted survival is <2 years for such patients. In the present long-term study, various chemotherapeutic regimens were used at varying dosages. Because these differences could not be controlled and owing to the small sample size, the efficacy of chemotherapy cannot be discussed in this study. Further clinical trials involving nomogram-based risk stratification are required to investigate the usefulness of perioperative chemotherapy.
Conclusions
The two nomograms for patients with CLM—the Kattan nomogram and the Kanemitsu nomogram—were found to be good predictors of survival. The Kanemitsu nomogram had better predictive ability in Japanese patients, whereas the Kattan nomogram could be applied to patients outside the United States. The nomograms provided better predictions than other well-known staging systems. The availability of these nomograms for external validation can encourage individual counseling and tailored decision-making with regard to perioperative chemotherapy.
References
Benoist S, Nordlinger B (2009) The role of preoperative chemotherapy in patients with resectable colorectal liver metastases. Ann Surg Oncol 16:2385–2390
Nordlinger B, Sorbye H, Glimelius B et al (2008) Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup Trial 40983): a randomised controlled trial. Lancet 371:1007–1016
Iwatsuki S, Dvorchik I, Madariaga JR et al (1999) Hepatic resection for metastatic colorectal adenocarcinoma: a proposal of a prognostic scoring system. J Am Coll Surg 189:291–299
Fong Y, Fortner J, Sun RL et al (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 230:309–318 (discussion 318–321)
Rees M, Tekkis PP, Welsh FK et al (2008) Evaluation of long-term survival after hepatic resection for metastatic colorectal cancer: a multifactorial model of 929 patients. Ann Surg 247:125–135
Nordlinger B, Guiguet M, Vaillant JC et al (1996) Surgical resection of colorectal carcinoma metastases to the liver: a prognostic scoring system to improve case selection, based on 1568 patients: Association Francaise de Chirurgie. Cancer 77:1254–1262
Minagawa M, Yamamoto J, Kosuge T et al (2007) Simplified staging system for predicting the prognosis of patients with resectable liver metastasis: development and validation. Arch Surg 142:269–276 (discussion 277)
Mala T, Bohler G, Mathisen O et al (2002) Hepatic resection for colorectal metastases: can preoperative scoring predict patient outcome? World J Surg 26:1348–1353. doi:10.1007/s00268-002-6231-x
Merkel S, Bialecki D, Meyer T et al (2009) Comparison of clinical risk scores predicting prognosis after resection of colorectal liver metastases. J Surg Oncol 100:349–357
Mann CD, Metcalfe MS, Leopardi LN et al (2004) The clinical risk score: emerging as a reliable preoperative prognostic index in hepatectomy for colorectal metastases. Arch Surg 139:1168–1172
Yamaguchi T, Mori T, Takahashi K et al (2008) A new classification system for liver metastases from colorectal cancer in Japanese multicenter analysis. Hepatogastroenterology 55:173–178
Kattan MW, Heller G, Brennan MF (2003) A competing-risks nomogram for sarcoma-specific death following local recurrence. Stat Med 22:3515–3525
Kattan MW, Karpeh MS, Mazumdar M et al (2003) Postoperative nomogram for disease-specific survival after an R0 resection for gastric carcinoma. J Clin Oncol 21:3647–3650
Brennan MF, Kattan MW, Klimstra D et al (2004) Prognostic nomogram for patients undergoing resection for adenocarcinoma of the pancreas. Ann Surg 240:293–298
Cagiannos I, Karakiewicz P, Eastham JA et al (2003) A preoperative nomogram identifying decreased risk of positive pelvic lymph nodes in patients with prostate cancer. J Urol 170:1798–1803
Diblasio CJ, Kattan MW (2003) Use of nomograms to predict the risk of disease recurrence after definitive local therapy for prostate cancer. Urology 62(Suppl 1):9–18
Kattan MW (2003) Nomograms are superior to staging and risk grouping systems for identifying high-risk patients: preoperative application in prostate cancer. Curr Opin Urol 13:111–116
Kattan MW, Zelefsky MJ, Kupelian PA et al (2003) Pretreatment nomogram that predicts 5-year probability of metastasis following three-dimensional conformal radiation therapy for localized prostate cancer. J Clin Oncol 21:4568–4571
Kattan MW, Reuter V, Motzer RJ et al (2001) A postoperative prognostic nomogram for renal cell carcinoma. J Urol 166:63–67
Van Zee KJ, Manasseh DM, Bevilacqua JL et al (2003) A nomogram for predicting the likelihood of additional nodal metastases in breast cancer patients with a positive sentinel node biopsy. Ann Surg Oncol 10:1140–1151
Kattan MW, Gonen M, Jarnagin WR et al (2008) A nomogram for predicting disease-specific survival after hepatic resection for metastatic colorectal cancer. Ann Surg 247:282–287
Kanemitsu Y, Kato T (2008) Prognostic models for predicting death after hepatectomy in individuals with hepatic metastases from colorectal cancer. World J Surg 32:1097–1107. doi:10.1007/s00268-007-9348-0
Giacchetti S, Itzhaki M, Gruia G et al (1999) Long-term survival of patients with unresectable colorectal cancer liver metastases following infusional chemotherapy with 5-fluorouracil, leucovorin, oxaliplatin and surgery. Ann Oncol 10:663–669
Simmonds PC, Primrose JN, Colquitt JL et al (2006) Surgical resection of hepatic metastases from colorectal cancer: a systematic review of published studies. Br J Cancer 94:982–999
De Jong MC, Mayo SC, Pulitano C et al (2009) Repeat curative intent liver surgery is safe and effective for recurrent colorectal liver metastasis: results from an international multi-institutional analysis. J Gastrointest Surg 13:2141–2151
Van Cutsem E, Rivera F, Berry S et al (2009) Safety and efficacy of first-line bevacizumab with FOLFOX, XELOX, FOLFIRI and fluoropyrimidines in metastatic colorectal cancer: the BEAT study. Ann Oncol 20:1842–1847
Conflict of interest
The authors have no commercial associations that might pose a conflict of interest in connection with the submitted article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takakura, Y., Okajima, M., Kanemitsu, Y. et al. External Validation of Two Nomograms for Predicting Patient Survival After Hepatic Resection for Metastatic Colorectal Cancer. World J Surg 35, 2275–2282 (2011). https://doi.org/10.1007/s00268-011-1194-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-011-1194-4