Abstract
Introduction
Irish general surgery faces a recruitment crisis with only 87 of 145 (60%) basic surgical training (BST) places filled in 2009. We assessed basic surgical trainees to identify objective, and potentially modifiable, factors that influence ultimate recruitment into a general surgical career.
Methods
Candidates commencing BST training during a 5-year period between 2004 and 2008 were included in a quantitative study. In addition a total of 2,536 candidates, representing all those who commenced surgical training in Ireland since 1960 were identified through the Royal College of Surgeons in Ireland (RCSI) database and invited to complete an online survey. Statistical analysis was performed using SPSS version 15, with p < 0.05 considered significant.
Results
During the 5-year quantitative study period there were 381 BST trainees. Gender was a significant predictor of career choice with women more likely to ultimately choose a nonsurgical career after initial surgical training (p = 0.049). Passing surgical membership examinations (MRCS) also was predictive of remaining in surgery (p = 0.005). Training region was not a significant predictor of ultimate career choice. There were 418 survey respondents. The influence of role models was most commonly cited as influencing candidates in choosing to commence surgical training. Candidates who rated “academic opportunity” (p = 0.023) and “intellectual challenge” (p = 0.047) as factors that influenced their decision to commence surgical training were more likely to ultimately continue their careers in a surgical speciality.
Conclusions
This study describes the career pathway of surgical trainees and confirms the importance of academic achievement in discriminating between candidates applying for surgical training schemes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In Ireland, after completion of medical school, graduates must complete a mandatory 1-year internship to be registered as medical practitioners with the Irish Medical Council. Those who wish to pursue a career in surgery must then interview for placement in a 2-year basic surgical training (BST) scheme consisting of four 6-month rotations. All trainees must complete at least 6 months of general surgery, and approximately 80% spend 1 year rotating through general surgery placements. During the BST scheme candidates are required to pass Membership to the Royal College of Surgeons (MRCS) examinations. Having completed BST, candidates interested in a general surgical career are then required to attain a higher degree through research to successfully attain placement on a higher surgical training (HST) scheme. Progression to HST is competitive with only seven training places per year in general surgery.
At present, recruitment of graduates to commence surgical training faces a potential crisis with only 87 of 145 (60%) BST places filled in 2009. In addition, withdrawal rates from the BST program are significantly higher now than in the past; 25% of BST candidates in 2007 withdrew before completion of the 2-year scheme compared with only 5% in 2002. At present the practice of medicine in Europe is undergoing enormous change with the inevitable implementation of the European Working Time Directive (EWTD). In a statement by the Royal College of Surgeons of England regarding the implementation of the EWTD, they have highlighted the need to train a greater number of surgeons to maintain current patient safety levels [1]. This requirement is likely to be mirrored across Europe.
The need to train a greater number of surgeons has been reported in the United States where manpower analyses predict a worsening shortage of general surgeons during the next 10–20 years [2]. However, the output of the Accreditation Council for Graduate Medical Education (ACGME) reports that accredited residency programs in general surgery has remained constant at approximately 1,000 chief residents per year since the early 1980s, despite a population increase of more than 33% since that time [3].
Given the need to train more consultant surgeons, it is instructive to consider the cost implications of such an undertaking. The economic worth of a general surgeon to the hospital in which they are working has been estimated to be $1.05–$2.4 million per annum in the United States [4]. In contrast to this is the high cost associated with training NCHDs to consultant surgeon proficiency [5]. The cost of using operating room time for training surgical residents in the United States is an estimated $53 million per year [6]. It is intuitive then, that in a time of economic crisis, that optimizing training of surgical trainees would have positive financial ramifications both for training institutions, and healthcare systems as a whole. Optimizing surgical training begins with recruitment, and it is essential that the right candidate is attracted into a surgical training scheme.
To optimize recruitment, we believe that it is important to assess surgical trainees with regard to identifying both objective and subjective factors that influence surgical trainees in continuing their careers in surgery. Previous studies assessing objective factors, such as gender, noted that although women now represent 50% of medical students, in the United States they account for only 20% of surgical residencies [7–10]. In addition, several studies have investigated the subjective factors that influence medical students and junior doctors in choosing a career in surgery [7, 10–13]. A previous Irish survey-based study found that amongst medical school students considering a career in surgery, men were more likely to be influenced by financial reward and prestige in choosing their ultimate career specialty, whereas females were more likely to rate lifestyle factors as important [8]. For those who choose to pursue nonsurgical careers, it has been suggested that a “controllable lifestyle” is becoming an essential factor in career selection [13–16]. The aforementioned studies have highlighted a diminishing medical student interest in surgical careers, with training duration, the demanding nature of surgical training, and associated lifestyle noted as factors contributing to this diminishing interest. However, such studies are survey-based and therefore are purely subjective.
Our goal was to assess basic surgical trainees during a 5-year period to identify objective quantifiable factors associated with continuation in a surgical career with particular focus on general surgery. We further sought to identify subjective factors that influenced surgical trainees in Ireland in commencing surgical training, and subsequently leaving surgery where applicable.
Methods
The study design consisted of two distinct parts. The first part of the study was commenced in November 2009 and involved identification of quantitative objective factors that influence surgical trainees commencing training during a 5-year period. The second part of the study assessed subjective factors and consisted of circulating a survey in December 2009 amongst all candidates commencing surgical training in Ireland during a 50-year period, including those candidates enrolled in our quantitative study.
With regard to our quantitative study of objective factors, all candidates commencing BST training during a 5-year period between 2004 and 2008 were identified through the Royal College of Surgeons in Ireland (RCSI) database and were included in a retrospective study. Factors assessed included gender, training region, nationality, and success in the MRCS examinations. These trainees were then followed up to determine their ultimate career choice.
Follow-up was performed using the Irish medical council register where trainees are registered to a particular speciality. For those trainees who were not registered to a particular speciality, determination of their ultimate career choice was performed through assessment of peer-reviewed publications in the 6 months before commencement of the study as well as internet searches.
The second part of our study assessing subjective factors involved the design and hosting of an online survey at www.surginfection.com—a surgical education website developed by the authors. A total of 2,536 candidates—representing all those who commenced surgical training in Ireland since 1960—were identified through the RCSI database. These candidates were invited via email to complete the online survey. Participation was voluntary and anonymous. Candidates ultimate career choice was determined and a detailed Likert scale assessed the importance of “academic,” “clinical,” and “lifestyle” factors in determining career choice and progression using a survey model previously described in the literature [8]. When the online survey was accessed, candidates were asked to “indicate how much each of the factors below influenced you in choosing a surgical career.” Those who had left surgery were asked, “How did the following factors influence your decision to leave surgery?” Candidates were asked to rate the influence of different factors as “no influence,” “minimal influence,” “moderate influence,” “strong influence,” or “very strong influence.”
Both objective and subjective factors were collected and tabulated to Microsoft Excel for transfer to SPSS version 15 as two distinct data sets. Candidates ultimate career choice was grouped into general surgery, other surgical specialty, and nonsurgical specialty for cross-tabulation with Chi-squared analysis of factors associated with each career choice. Associations with p < 0.05 were considered significant.
Results
Quantitative study
During the 5-year study period, there were 381 BST trainees, of whom 45.4% (173/381) were of Irish nationality. Of the 381 trainees, 85.3% (n = 325) completed their BST training, and there was a 12% (n = 56) withdrawal rate. Career follow-up data were obtained for 61% (232/381) of trainees. With regard to ultimate career choice, general surgery was most commonly chosen, accounting for 30.2% (70/232) of candidates. The remainder of the top five careers chosen by BST trainees were orthopedics (n = 30; 12.9%), radiology (n = 23 9.9%), plastic surgery (n = 17; 7.3%), and general practice (n = 15, 6.5%; Fig. 1).
Overall, 73% (279/381) were men and 27% (102/381) were women. Men were more likely to continue their career in a surgical speciality, whereas women were significantly more likely to ultimately choose a nonsurgical speciality (p = 0.049).
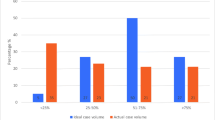
Of the 381 trainees, 28.3% (108/381) passed their MRCS examinations in a single attempt. Of the remainder, 38.1% (145/381) obtained their MRCS examinations after multiple attempts. In total, 18.4% (70/381) of trainees failed to pass their MRCS examinations and another 15.2% (58/381) of trainees did not attempt the examinations at all. Overall, candidates passing their MRCS examinations were more likely to choose a career in surgery than a nonsurgical speciality (p = 0.023). However, there was no significant association between BST training region or nationality and ultimate career choice.
Online survey
Demographics
A total of 1,609 candidates were invited to complete the online survey. There were 418 responses, giving a response rate of 26%. Candidates responding had obtained their medical degrees between 1967 and 2008. The majority were Irish (75.8%; n = 317). Those from Asia accounted for 8.6% (n = 36), Africa 8.1% (n = 34), European 5.2% (n = 22), North America 1.9% (n = 8), and Australia 0.2% (n = 1). Overall 80.6% (n = 337) had obtained their medical degree in Ireland. With regard to surgical training region, 95% (n = 397) of trainees commenced surgical training in Ireland. Dublin-based trainees represented the majority, comprising 54% (n = 226) of respondents.
In total, 353 (84%) respondents had continued their career in surgery after commencing surgical training. Of these, 144 (46%) had continued in general surgery. There were 52 (16.2%) respondents who had ultimately chosen a career in orthopedics and 27 (8.6%) who had chosen a career in plastic surgery. The remaining 90 (28.8%) respondents represented all other surgical specialities. Of the 418 respondents, 65 (15.5%) indicated that they had chosen a nonsurgical career after commencing surgical training. As per our quantitative study results, there were no significant associations between surgical training region or nationality and ultimate career choice.
Factors influencing candidates in commencing surgical training
Of those surveyed, the influence of role models (84%; n = 351) was most commonly cited as influencing candidates in choosing to commence surgical training (Fig. 2). This was followed by intellectual challenge (83.7%; n = 350) and undergraduate experience (73.7%; n = 308). Career opportunities (53.1%; n = 222) and academic opportunities (51.4%; n = 215) comprised the remainder of the top five influencing factors in choosing to commence surgical training. Candidates who rated academic opportunity (p = 0.023) and intellectual challenge (p = 0.047) as factors that influenced their decision to commence surgical training were more likely to ultimately continue their careers in a surgical speciality. Furthermore, those who rated academic opportunity (p < 0.001) and research opportunity (p = 0.03) as important factors were more likely to continue their careers in general surgery rather than a surgical speciality (Table 1). Candidates who commenced surgical training because of geographic convenience of location were more likely to ultimately leave surgery to pursue an alternative career (p = 0.01).
Factors influencing candidates in choosing to leave surgery
Of those surveyed who had left surgery to pursue an alternative career, the most influential factor in their decision to leave was lack of “career opportunity” (75.4%; n = 49). This was followed by “lifestyle during training” (61.5%; n = 40), “growing interest in a nonsurgical speciality” (61.5%; n = 40), “length of surgical training” (58.5%; n = 38), and “on-call demands” (58.5%; n = 38). Candidates who left surgery because of concerns regarding “future employment” were more likely to ultimately pursue a career in general practice (p = 0.027). Those citing length of training as a more significant factor in their decision to leave surgery were more likely to choose a career in radiology (p = 0.023).
Discussion
This study demonstrates that significant proportion of surgical trainees ultimately choose a career in a nonsurgical speciality. We have shown that gender and success at MRCS examinations are significantly relevant quantitative factors for choosing a surgical career. With regard to our survey findings, we have demonstrated that surgeons overall and general surgeons in particular are more likely to rank academic factors as important in their choosing to pursue a surgical career compared with those who ultimately leave surgery.
We acknowledge a number of limitations of our study. Our quantitative study followed up only 61% of our BST cohort. Given that many of these trainees were not registered on the Irish medical council database, this may represent high levels of emigration amongst our surgical trainees who may be pursuing careers in surgery abroad. Similarly although our online survey had more than 400 respondents, this merely represented a 26% response rate, which was only reached after a second reminder email was sent to candidates invited to complete the survey. However, this low survey response rate also stresses the importance of quantitative assessment, such as that performed in the first part of our study.
As per previous studies, our study confirms the preponderance of male surgical trainees; women accounted for only 27% (102/381) of trainees beginning BST. In our cohort, women were significantly more likely to ultimately leave surgery having commenced training. Previous survey-based studies have demonstrated that women weighed lifestyle during and after training, along with working hours, as influential in career decisions [8]. It seems intuitive then that women would be less likely to choose a career in surgery and our study validates this.
Furthermore, in our quantitative study, we have shown that the more successful trainees at MRCS examinations tend to continue their careers in surgery (p = 0.023). This is borne out in our survey results, where candidates motivated by academic opportunity and intellectual challenge were significantly more likely to remain in surgery. At present in applying for higher surgical training (HST) in the United Kingdom and Ireland, 25% of the application points available are designated to which higher degrees the candidate holds, as well as any research publications or presentations that they may have. This study vindicates such application criteria, further stressing the importance of previous academic achievement in ensuring that candidates successful in attaining a surgical training scheme ultimately continue their careers in a surgical speciality. This is particularly the case in general surgery, where candidates ultimately choosing a general surgical career have been previously more likely to have had a greater interest in academia and research than other surgical specialities.
It is interesting to note that in our 5-year cohort of surgical trainees, a career in radiology was more commonly chosen than any surgical speciality with the exception of general surgery and orthopedic surgery. Two of the top five career choices were nonsurgical; general practice was the fifth most popular ultimate career choice. In fact, more than one-third (n = 81/232; 34.9%) of trainees on whom follow-up data were available ultimately choose a nonsurgical career after having started basic surgical training. This does not correlate with our online survey data, in which 84% of respondents indicated that they had continued their careers in surgery. This is likely due to the fact that surgeons and surgical trainees are more likely to respond to surveys from surgical departments and we believe our quantitative study findings are more indicative of the rates of candidates ultimately leaving surgery.
With this in mind, of equal importance in optimizing recruitment to surgical training schemes are the factors that influence trainees in choosing to leave surgery. Our study highlights the importance of lifestyle and clinical factors in causing trainees to leave surgery. “Lifestyle during training” and the “on-call rota” comprised two of the top five factors cited. This is in keeping with previous studies rating lifestyle factors as important in choosing a nonsurgical career [8, 13–15].
Clinical factors denoting dissatisfaction with the current surgical training model, such as length of training and lack of career opportunity also are highlighted as important. As the EWTD is implemented across Ireland and the United Kingdom, we may expect significant shifts in both clinical and lifestyle factors. However, perceived improvements relating to “lifestyle during training” and “on-call rotas” may be offset by increased “length of training.” As such it remains to be seen whether a more “lifestyle-friendly” surgical career pathway will in fact result in more trainees ultimately staying in surgery, particularly if length of training is increased as a result. This represents an opportunity for further research in this area as the lifestyle of a surgical trainee changes. A shift in the perceived lifestyle associated with a career in surgery may lead to surgery becoming a more attractive career choice. This may result in changing profiles amongst candidates who choose surgical careers.
Conclusions
We have identified a number of quantitative factors associated with continuing a career in surgery, including gender and success at surgical examinations. With regard to subjective factors, surgeons overall are more likely to rank academic factors as important in their choosing to pursue a surgical career compared with those who ultimately leave surgery. This confirms the importance of academic achievement in discriminating between candidates applying for surgical training schemes.
References
The Royal College of Surgeons of England and the European Working Time Directive: A Policy Statement, July 2003
Williams TE, Ellison EC (2008) Population analysis predicts a future critical shortage of general surgeons. Surgery 144:548–566
Russell JC, Fry DE (2010) Commentary: the case for expanding general surgery residencies. Acad Med 85(5):749–751
Cofer JB, Burns RP (2008) The developing crisis in the national general surgery workforce. J Am Coll Surg 206(5):790–795 (discussion 795–797)
Scott DJ, Bergen PC, Rege RV, Laycock R, Tesfay ST, Valentine RJ et al (2000) Laparoscopic training on bench models: better and more cost effective than operating room experience? J Am Coll Surg 191(3):272–283
Bridges M, Diamond DL (1999) The financial impact of teaching surgical residents in the operating room. Am J Surg 177(1):28–32
Azizzadeh A, McCollum CH, Miller CC III, Holliday KM, Shilstone HC, Lucci A Jr (2003) Factors influencing career choice among medical students interested in surgery. Curr Surg 60(2):210–213
Corrigan MA, Shields CJ, Redmond HP (2007) Factors influencing surgical career choices and advancement in Ireland and Britain. World J Surg 31(10):1921–1929
Marschall JG, Karimuddin AA (2003) Decline in popularity of general surgery as a career choice in North America: review of postgraduate residency training selection in Canada, 1996–2001. World J Surg 27(3):249–252
O’Herrin JK, Lewis BJ, Rikkers LF, Chen H (2003) Medical student operative experience correlates with a match to a categorical surgical program. Am J Surg 186(2):125–128
Calligaro KD, Dougherty MJ, Sidawy AN, Cronenwett JL (2004) Choice of vascular surgery as a specialty: survey of vascular surgery residents, general surgery chief residents, and medical students at hospitals with vascular surgery training programs. J Vasc Surg 40(5):978–984
Cochran A, Melby S, Neumayer LA (2005) An Internet-based survey of factors influencing medical student selection of a general surgery career. Am J Surg 189(6):742–746
De SK, Henke PK, Ailawadi G, Dimick JB, Colletti LM (2004) Attending, house officer, and medical student perceptions about teaching in the third-year medical school general surgery clerkship. J Am Coll Surg 199(6):932–942
Miller G, Bamboat ZM, Allen F, Biernacki P, Hopkins MA, Gouge TH et al (2004) Impact of mandatory resident work hour limitations on medical students’ interest in surgery. J Am Coll Surg 199(4):615–619
Schwartz RW, Simpson WG, Strodel WE, Jarecky RK, Griffen WO Jr, Young AB (1989) Career change: in quest of a controllable lifestyle. J Surg Res 47(3):189–192
Griffen WO Jr, Schwartz RW (1990) Controllable lifestyle as a factor in choosing a medical career. Am J Surg 159(2):189–190
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McHugh, S., Corrigan, M., Sheikh, A. et al. Factors Influencing Career Choice After Initial Training in Surgery. World J Surg 35, 487–492 (2011). https://doi.org/10.1007/s00268-010-0934-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-010-0934-1