Abstract
Background
There are few strategies for treating patients who have suffered cardiopulmonary arrest due to blunt trauma (BT-CPA). The aim of this population-based case series observational study was to clarify the outcome of BT-CPA patients treated with a standardized strategy that included an emergency department thoracotomy (EDT) under an emergency medical service (EMS) system with a rapid transportation system.
Methods
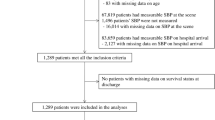
The 477 BT-CPA registry data were augmented by a review of the detailed medical records in our emergency department (ED) and action reports in the prehospital EMS records.
Results
Of those, 76% were witnessed and 20% were CPA after leaving the scene. In all, 18% of the patients went to the intensive care unit (ICU), the transcatheter arterial embolization (TAE) room, or the operating room (OR). Only 3% survived to be discharged. Among the 363 witnessed patients—11 of whom had ventricular fibrillation (VF) as the initial rhythm, 134 exhibiting pulseless electrical activity (PEA), and 221 with asystole—13, 1, and 3%, respectively, survived to discharge. The most common initial rhythm just after collapse was not VF but PEA, and asystole increased over the 7 min after collapse. There were no differences in the interval between arrival at the hospital and the return of spontaneous circulation between the patients that survived to discharge and deceased patients in the ED, OR, TAE room, or ICU. The longest interval was 17 min.
Conclusions
In BT-CPA patients, a 20-min resuscitation effort and termination of the effort are thought to be relevant. The initial rhythm is not a prognostic indicator. We believe that the decision on whether to undertake aggressive resuscitation efforts should be made on a case-by-case basis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The outcome of patients who experience out-of-hospital cardiopulmonary arrest (CPA) due to blunt trauma (BT-CPA) is poor [1–5]. Indeed, in some regions, such patients do not receive cardiopulmonary resuscitation (CPR) if they show no life signs on the scene or upon arrival at the hospital [6, 7]. Nevertheless, there are a few strategies for BT-CPA patients, although they are not always effective. Many hospitals and emergency departments (EDs) do not have a standardized or fixed approach for these cases even in a single geographic area, a single institute, or by a single physician, which results in a lack of reliable data with which to formulate treatment strategies or ascertain outcomes. Because we have few data concerning the outcomes of these cases, it is difficult to determine which therapeutic procedures should be used. The relation between the initial cardiac rhythm in BT-CPA patients and their prognosis is also unclear.
The aim of this population-based study was to clarify the outcome of BT-CPA patients treated with a standardized, fixed strategy that included emergency department thoracotomy (EDT) in a single, crowded ED under an emergency medical service (EMS) system with a quick transportation system. The study was conducted in Yokohama, Japan during the past 10 years.
Subjects and methods
This population-based single-center case series observational study used the medical records of the clinical courses of BT-CPA patients. These registry data were augmented by a review of the detailed medical records in our ED and of action reports in the prehospital EMS records. The outcomes of patients were examined according to the initial cardiac rhythm. The interval from arrival at the hospital to the return of spontaneous circulation (ROSC) of patients who survived to discharge was compared with that of patients who died in the ED, operating room (OR), transcatheter arterial embolization (TAE) room, or intensive care unit (ICU). Among the patients, the interval from collapse to arrival at the hospital of those who were taken to the ICU, TAE room, or OR (including survivors to discharge) was compared with that of patients who died in the ED with or without ROSC. Statistical analysis was performed using Student’s t-test.
Exclusion criteria included the following: patients displaying the full signs of death (rigor mortis, dead spot, decapitation) whom we could not resuscitate, patients received simultaneously with multiple other patients whom we could not resuscitate according to our strategy and patients showing a little hemorrhage and distinct evidence of a fainting attack before the BT-CPA including an ischemic heart attack, cerebral attack, or hypoglycemic attack. In Japan, there is no legal or ethical protocol concerning the treatment strategy for patients without vital signs or signs of life. We are usually required to try to resuscitate CPA patients independent of their vital signs or signs of life, and these efforts often prove fruitless.
We have taken three approaches to patients who are not excluded by these criteria that are an existing trauma system and not a study intervention: (1) a unique aggressive treatment strategy; (2) an in-hospital system that supports aggressive resuscitation; and (3) a prehospital EMS system in our city. We treated these patients according to our strategy for BT-CPA that was established in 1994. It includes aggressive resuscitation for at least 30 min after arrival at the hospital, insertion of a 7F sheath introducer into the subclavian vein for aggressive infusion, epinephrine administration every 3 min, and EDT including intrathoracic hemostasis, open-chest cardiac massage, and cross-clamping the descending thoracic aorta. During resuscitation we perform some simple radiographic examinations and ultrasonography (US) for all patients basically according to the concept of several trauma courses (e.g., Japanese Advanced Trauma Evaluation and Care) and blood transfusion based on the physician’s decision early in the study period. After ROSC, we performed CT and blood transfusion if necessary. We then moved to the OR or TAE room based on the physical, radiographic, and US findings.
Second, we have also established an in-hospital system for supporting aggressive resuscitation attempts. This system includes logistical considerations such as close proximity between the ED and the TAE room, the placement of CT and radiography facilities on the same floor, direct access to the OR by an exclusive elevator, and common instruments that are interchangeable between the ED and OR, including surgical beds (Fig. 1). We can operate just after arrival in the OR without transferring the patient from the ED stretcher to the operating bed. At the same time, we perform all types of operations in the ED using the same instruments that are used in the OR. These operations include all types of damage control surgery, major abdominal surgery, and open thoracic aortic surgery [8], which are performed by surgical specialists. In Japan, there is no identified specialty for trauma surgery or acute care surgery, and trauma patients are usually operated on by surgeons with some surgical specialty who are familiar with trauma or acute care specialists who are familiar with acute care surgery. Some specialists stay in the hospital and others stay at home but can usually come to the hospital within 30 min.
Logistical considerations including close proximity between the emergency center/department (ED) and catheter intervention room, or transcatheter arterial embolization (TAE) room; placement of computed tomography (CT) and radiography facilities on the same floor; direct access to the operating room (OR) by an exclusive elevator; and common instruments interchangeable between the ED and OR, including surgical beds. ICU intensive care unit; BCU burn care unit; OPD outpatient department; GF ground floor; 1F first floor; 3F third floor
Third, we have established a prehospital and interhospital EMS system in our city for severely injured patients, including those with CPA. Yokohama, which is south of Tokyo, is the second-largest city in Japan, and our institution is located in the city center. The surface area and population of Yokohama are 434 km2 and 3.37 million people, respectively.
We selected 11 hospitals, including our center, whose EDs can receive and treat all patients with CPA independent of their capacity. An emergency director (medical doctor) who works for the city’s fire department coordinates the activities of ambulance crews, including emergency life-saving technicians (ELSTs), and oversees the transfer of CPA patients to the nearest of the 11 selected hospitals [9].
For each hospital in Yokohama, all data concerning CPA patients are population-based. Under our EMS system, the interval between the ambulance’s departure from the ambulance station to its arrival at the scene (response interval) for CPA cases is 6.0 min (2.3 km in distance). The interval between arrival at the scene and departure from it (on-scene interval) for CPA cases is 12.9 min. The interval from departure from the scene to arrival at the hospital is 7.2 min (4.6 km). The interval from arrival at the hospital to arrival back at the ambulance station (delivery interval + recovery interval) is 34.1 min (4.4 km). The interval between leaving the ambulance station and returning to the fire station (out-of-service interval) is 60.7 min. All of the given time intervals represent the average time.
Results
Over the past 10 years, 477 BT-CPA patients have been treated. Their mean age was 44 years, and the main mechanisms of trauma were road traffic accidents and falls (Fig. 2). Among those with CPA, 363 (76%) were witnessed, and 95 (20%) occurred after leaving the scene. EDT with open-chest CPR was performed in 408 (86%) cases, and aortic cross-clamping was performed in 341 (71%). In all, 69 patients did not undergo EDT because of rapid ROSC before EDT, the difficulty of controlling massive bleeding, or the difficulty of repair. Although ROSC was established after administration of 2.82 mg of epinephrine (mean) in 161 (34%) cases, most died within 24 hours of arriving at the hospital. Only 14 (3%) patients survived more than 7 days. A total of 85 (18%) patients were sent to the ICU, TAE room, or OR (admitted); only 13 (3%) survived to discharge (survivors) (Figs. 3, 4). Most of the survivors were in a vegetative status at discharge (Table 1). Abdominal damage control surgery was performed in 15 cases. Among the 363 witnessed patients, 142 (39%) achieved ROSC; among them, 76 (21%) were admitted and 9 (2%) survived to discharge.
The initial rhythms presented at the scene were ventricular fibrillation (VF) in 11 patients, pulseless electrical activity (PEA) in 153 patients, and asystole in 313 patients. Of the 11 patients displaying VF, 4 (36%) achieved ROSC and 1 (9%) survived to discharge. The mean interval from CPA confirmation to the initial rhythm check by defibrillator was 6.4 min. Among the 153 patients with PEA as the initial rhythm, 81 (53%) achieved ROSC, 41 (27%) were admitted, and 3 (2%) survived to discharge. The number of patients presenting with VF was small, and they appeared either in the very early phase (within 4 min) or in the later phase (7–10 min). The latter appeared just after the peak of the appearance of patients presenting with PEA (5–8 min). The rate of patients showing asystole increased as an initial rhythm over 7–12 min after collapse (Fig. 5). Of the 11 VF patients, 5 did not undergo defibrillation because the interval to the natural disappearance of VF was too short, and they died in the ED. The other 6 patients underwent attempted defibrillation during transfer; however, 4 could not be defibrillated until their arrival at the hospital. Of those four patients, two were successfully defibrillated to achieve ROSC after tracheal intubation with adequate oxygenation, bolus crystalloid infusion, and epinephrine administration in the ED. One survived to discharge (Fig. 6).
A total of 92 patients, or 60% of the 153 BT-CPA patients, showing PEA as the initial cardiac rhythm at the scene presented with PEA upon arrival at our center. Of those patients, 3 (3%) survived to discharge. On the other hand, 61 (40%) had an asystolic rhythm upon arrival, and none survived to discharge. Of the 313 patients with asystole as the initial cardiac rhythm on the scene, 76 (24%) achieved ROSC, 42 (13%) were admitted, and 9 (3%) survived to discharge.
Among the eight witnessed patients displaying VF at the scene, 3 (38%) achieved ROSC, and 1 (13%) survived to discharge. Among the 134 patients displaying PEA, 75 (56%) achieved ROSC, 38 (28%) were admitted, and 1 (1%) survived to discharge. Among the 221 patients showing asystole, 64 (29%) achieved ROSC, 37 (17%) were admitted, and 7 (3%) survived to discharge (Fig. 7). The most common initial rhythm just after collapse in witnessed patients was not VF but PEA.
There were no statistical differences in the interval from arrival at the hospital to ROSC between patients who survived to discharge and deceased patients in the ED, OR, TAE room, or ICU. The longest interval from arrival at the hospital to ROSC for patients who survived to discharge was 17 min. There were no survivors to discharge for whom the interval was more than 18 min (Fig. 8). On the other hand, the interval from collapse to arrival at the hospital for patients who survived to discharge and patients taken to the ICU, TAE room, or OR was shorter than that of patients who died in the ED with or without ROSC (P < 0.05). The longest interval from collapse to arrival was 47 min for patients who survived to discharge (Fig. 9).
Interval from collapse to arrival among witnessed patients. The interval for patients who survived to discharge and patients taken to the ICU, TAE room, or OR was shorter than that of patients who died in the ED with or without ROSC. The longest interval was 47 min for patients who survived to discharge and 89 min for patients sent to the ICU, TAE room, or OR after ROSC
Discussion
In a joint position paper, the National Association of EMS Physicians Standards and Clinical Practice Committee and the American College of Surgeons Committee on Trauma published guidelines for withholding or terminating resuscitation attempts in prehospital traumatic cardiopulmonary arrest (NAEMSP/ASCOT guidelines) [6]. The guidelines demonstrate the importance of triaging traumatic CPA patients on scene to preserve resources and to maximize benefits because survival after traumatic CPA, particularly after BT-CPA, is rare, even with maximum resuscitative efforts [6]). Many authors have reported extremely poor prognoses for traumatic CPA patients (survival rates of 0–3.7%) [3, 6, 10–12] and have considered attempts to resuscitate BT-CPA patients as futile and as an inappropriate use of precious medical resources. The reports also point out the risks to rescuers and the financial burdens of such attempts [3, 10, 11, 13, 14].
On the other hand, some other experts have emphasized that the adoption of these guidelines remains controversial and that they are not applicable to rapid transport systems outside the United States. Some authors have said that although only a small number of BT-CPA patients who receive CPR survive to discharge this therapy is not always futile. Indeed, some articles have documented the successful resuscitation of BT-CPA patients who might not have survived if the NAEMSP/ASCOT guidelines [6] been strictly applied to them.
The predictors of successful resuscitation in cases of traumatic CPA are controversial. Some authors have concluded that sinus rhythm and pupil size, and its reactivity, are important physiologic variables that predict potential survival and may be used to guide the continuation of resuscitative efforts in traumatic CPA patients [10]. However, others have insisted that prehospital clinical assessments (e.g., pupillary light response, the presence of a respiratory effort, a sinus electrocardiogram) are not reliable for triaging BT-CPA patients. Those authors concluded that BT-CPA patients should be transported to the ED for further evaluation and care and that NAEMSP/ASCOT guidelines [6] should not be adopted until more thorough studies are conducted [3]. Our present data also showed no reliable predictors of successful resuscitation.
Even after full examinations during and after resuscitation, we cannot strictly differentiate patients with CPA after blunt trauma due to medical problems from patients with BT-CPA in a narrow sense—which is significant limitation of this study. However, to resuscitate and treat these CPA patients, even after blunt trauma due to medical problems, we should control their injuries themselves using the same strategy as for “real” BT-CPA patients. Of course, it is important to manage the causative medical problems in these CPA patients. From the point of view of initial resuscitation at the ED, it may be needless to differentiate real BT-CPA strictly from CPA after trauma due to medical problems.
With regard to open-chest CPR, ILCOR guidelines in the ALS section state that no prospective randomized studies of the use of this procedure for resuscitation have been published; and, thus, there is no scientific consensus on the matter. The guidelines also found that the observed benefits of this procedure included improved coronary perfusion pressure [15] and increased ROSC [16, 17] in clinical situations, whereas some animal studies [18–22] have indicated that this procedure increased survival rates, perfusion pressure, and organ blood flow when compared with closed-chest CPR. The guidelines recommend considering this procedure for CPA patients when the chest or abdomen is already open. Other studies have demonstrated that patients with BT-CPA may benefit from open-chest CPR with the same probability as those patients with penetrating traumatic CPA. This observation is especially true if the procedure is started as soon as possible, no more than 20 min after the initial CPR [23]. On the other hand, some authors have proposed that resuscitative EDT is futile in patients with BT-CPA requiring prehospital CPR longer than 5 min and is warranted only in BT-CPA patients with pericardial tamponade, even among those presenting with asystole upon arrival [7]. We previously published data concerning the rate of survival in patients with penetrating traumatic CPA, which is slightly better than the rate derived from the current data on BT-CPA [24].
Based on our present data, we can neither prove nor disprove the usefulness of EDT, open-chest CPR, or cross-clamping of the thoracic descending aorta for the treatment of BT-CPA. Although proportionately fewer patients underwent EDT among survivors than among nonsurvivors, survivors who did not undergo EDT quickly achieved ROSC before we completed the EDT and started open-chest cardiac massage. Moreover, although EDT is indeed an invasive procedure, repair of the thoracotomy wound and hemostasis of the wound are easily and quickly completed after ROSC. We find EDT to be worth trying. We usually perform closed-chest compression from the right side of the patient and then stopped it when the surgeon used a knife for the thoracotomy from the left side to avoid iatrogenic injury to the rescuer. We start closed-chest compression again as soon as possible when the surgeon used scissors. The duration of interference with chest compression in this procedure can be shortened to less than 10 seconds, which is also the duration permitted for checking rhythm during closed-chest CPR. We can even shorten the compression-interference time for the whole EDT procedure if we combine the duration of knife usage during EDT with the duration of rhythm checking during CPR.
It is well known that patients with nontraumatic CPA who present with VF as the first cardiac rhythm have a good prognosis. In most cases, VF means that the etiology of the CPA is cardiogenic and treatable. Moreover, we can easily treat VF, which means successful defibrillation with an electrical procedure even if the etiology of CPA is not cardiogenic. However, we can hardly treat patients with BT-CPA displaying VF to survive to discharge. Some authors have reported that CPA patients who present with VF have a better chance of survival (33–74%) [25, 26] than those presenting with PEA or asystole [25, 27–30]. Although the survival rate of VF patients seems to be little better than that of PEA and asystole patients with BT-CPA, based on the results of the present study, VF does not always indicate good life expectancy. We could not perform a statistical analysis owing to the small number of BT-CPA patients presenting with VF. Based on our data, patients presenting with VF were mainly seen either during the very early phase after collapse or just after the phase in which patients presenting with PEA were the major population. Additionally, it was difficult to defibrillate VF in BT-CPA patients using a defibrillator, unlike the case of cardiogenic CPA displaying VF.
The presentation of VF during the later phase was suspected to be a sign of lethal hypoxia and acidosis of the myocardial cells due to lethal hypovolemia or the terminal stage of PEA, not a simple abnormal electrical storm with viable myocardial cells. PEA in BT-CPA is usually thought to be a sign of lethal hypovolemia due to inadequate venous return, resulting in inadequate cardiac contraction. It is extremely difficult to save BT-CPA patients who present with VF as a terminal stage of PEA unless we control the massive bleeding, even if the VF is defibrillated. On the other hand, we can save patients presenting with lethal bradycardia or asystole as an initial cardiac rhythm if these lethal rhythms are mainly due to a nerve reflex such as a vagal reflex or temporary functional collapse of the central nervous system. Of course, in most cases asystole means the eternal collapse of all myocardial cells due to irreversible hypoxia or acidosis, or the last stage of life. We cannot save patients presenting with this type of asystole. We should differentiate the biologic significance of the initial cardiac rhythm of BT-CPA from those of nontraumatic CPA.
The present study showed that in the studied patients the shorter the interval from collapse to arrival at the hospital, the greater the chance for survival. Arrival at the hospital usually means the beginning of our contact with the patient and start of the medical treatment. We should transfer these victims to the hospital as quickly as possible, or we should contact them as early as possible on the scene. On the other hand, based on our experience of 477 BT-CPA patients, no patient can achieve ROSC after more than 18 min’ resuscitation effort. We think it is relevant to terminate the resuscitation effort after this time.
Conclusions
The expected outcome of BT-CPA patients is dismal. However, because some BT-CPA patients who survived to discharge were not witnessed by anyone and showed asystole as the initial cardiac rhythm at the scene, we cannot and should not stop efforts to resuscitate them merely because they have BT-CPA. In the studied BT-CPA patients, the interval from the event to arrival at the hospital was not a prognostic indicator. However, our data show that a 20-min resuscitation effort and termination of the effort after that time are thought to be relevant, and we recommend 20 min of resuscitation. Additionally, the initial rhythm is not a prognostic indicator like VF, PEA, and asystole are for nontraumatic cardiogenic CPA. We recommend that the decision on whether to undertake aggressive resuscitation efforts should be decided on a case-by-case basis.
References
Willis CD, Cameron PA, Bernard SA et al (2006) Cardiopulmonary resuscitation after traumatic cardiac arrest is not always futile. Injury 37:448–454
Lockey D, Crewdson K, Davies G (2006) Traumatic cardiac arrest: who are the survivors? Ann Emerg Med 48:240–244
Pickens JJ, Copass MK, Bulger EM (2005) Trauma patients receiving CPR: predictors of survival. J Trauma 58:951–958
Pepe PE, Swor RA, Ornato JP et al (2001) Resuscitation in the out-of-hospital setting: medical futility criteria for on-scene pronouncement of death. Prehosp Emerg Care 5:79–87
Grove CA, Lemmon G, Anderson G et al (2002) Emergency thoracotomy: appropriate use in the resuscitation of trauma patients. Am Surg 68:313–317
Hopson LR, Hirsh E, Delgado J, et al (2003) Guidelines for withholding or termination of resuscitation in prehospital traumatic cardiopulmonary arrest: a joint position paper from the National Association of EMS Physicians Standards and Clinical Practice Committee and the American College of Surgeons Committee on Trauma. J Am Coll Surg 196:106–112; Prehosp Emerg Care 7:141–146
Powell DW, Moore EE, Cothren CC et al (2004) Is emergency department resuscitative thoracotomy futile care for the critically injured patient requiring prehospital cardiopulmonary resuscitation? J Am Coll Surg 199:211–215
Moriwaki Y, Sugiyama M, Toyoda H et al (2006) Monitoring and evaluation of intraperitoneal bleeding (IPB) by small portable ultrasonography during transcatheter arterial embolization (TAE) in abdominal-pelvic trauma patients with shock: as a monitor for early detection of increase of IPB. Hepatogastroenterology 53:175–178
Moriwaki Y, Sugiyama M, Hayashi H et al (2001) Emergency medical service system in Yokohama, Japan. Ann Degli Ospedali San Camillo Forlanini 3:344–356
Cera SM, Mostafa G, Sing RF et al (2003) Physiologic predictors of survival in post-traumatic arrest. Am Surg 69:140–144
Rosemurgy AS, Norris PA, Olson SM et al (1993) Prehospital traumatic cardiac arrest: the cost of futility. J Trauma 35:468–474
Mazzorana V, Smith RS, Morabito DJ et al (1994) Limited utility of emergency department thoracotomy. Am Surg 60:516–521
Luk SS, Jacobs L, Ciraulo DL et al (1999) Outcome assessment of physiologic and clinical predictors of survival inpatients after traumatic injury with trauma score less than 5. J Trauma 46:122–128
Fulton RL, Voigt WJ, Hilakos AS (1995) Confusion surrounding the treatment of traumatic cardiac arrest. J AM Coll Surg 181:209–214
Boczar ME, Howard MA, Rivers EP et al (1995) A technique revisited: hemodynamic comparison of closed- and open-chest cardiac massage during human cardiopulmonary resuscitation. Crit Care Med 23:498–503
Takino M, Okada Y (1993) The optimum timing of resuscitative thoracotomy for non-traumatic out-of-hospital cardiac arrest. Resuscitation 26:69–74
Weil MH, Rackow EC, Trevino R et al (1986) Difference in acid-base state between venous and arterial blood during cardiopulmonary resuscitation. N Engl J Med 315:153–156
Angelos MG, DeBehnke DJ, Leasure JE (1992) Arterial pH and carbon dioxide tension as indicators of tissue perfusion during cardiac arrest in a canine model. Crit Care Med 20:1302–1308
DeBehnke DJ, Angelos MG, Leasure JE (1991) Comparison of standard external CPR, open-chest CPR, and cardiopulmonary bypass in a canine myocardial infarct model. Ann Emerg Med 20:754–760
Bircher N, Safar P (1985) Cerebral preservation during cardiopulmonary resuscitation. Crit Care Med 13:185–190
Kern KB, Sanders AB, Badylak SF et al (1987) Long-term survival with open-chest cardiac massage after ineffective closed-chest compression in a canine preparation. Circulation 75:498–503
Raessler KL, Kern KB, Sanders AB et al (1988) Aortic and right atrial systolic pressures during cardiopulmonary resuscitation: a potential indicator of the mechanism of blood flow. Am Heart J 115:1021–1029
Fialka C, Sebok C, Kemetzhofer P et al (2004) Open-chest cardiopulmonary resuscitation after cardiac arrest in cases of blunt chest or abdominal trauma: a consecutive series of 38 cases. J Trauma 57:809–814
Moriwaki Y, Sugiyama M, Toyoda H et al (2010) Cardiopulmonary arrest on arrival due to penetrating trauma. Ann R Coll Surg Engl 92:142–146
Hallstrom A, Rea TD, Mosesso VN Jr et al (2007) The relationship between shocks and survival in out-of-hospital cardiac arrest patients initially found in PEA or asystole. Resuscitation 74:418–426
Herlitz J, Bahr J, Fischer M et al (1999) Resuscitation in Europe: a tale of five European regions. Resuscitation 41:121–131
Bunch TJ, Hammill SC, White RD (2005) Outcomes after ventricular fibrillation out-of-hospital cardiac arrest: expanding the chain of survival. Mayo Clin Proc 80:774–782
Atwood C, Eisenberg MS, Herlitz J et al (2005) Incidence of EMS-treated out-of-hospital cardiac arrest in Europe. Resuscitation 67:75–80
Rea TD, Eisenberg MS, Sinibaldi G et al (2004) Incidence of EMS-treated out-of-hospital cardiac arrest in the United States. Resuscitation 63:17–24
Nishiuchi T, Hayashino Y, Fukuhara S et al (2008) Survival rate and factors associated with 1-month survival of witnessed out-of-hospital cardiac arrest of cardiac origin with ventricular fibrillation and pulseless ventricular tachycardia: the Utstein Osaka project. Resuscitation 78:307–313
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moriwaki, Y., Sugiyama, M., Yamamoto, T. et al. Outcomes from Prehospital Cardiac Arrest in Blunt Trauma Patients. World J Surg 35, 34–42 (2011). https://doi.org/10.1007/s00268-010-0798-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-010-0798-4