Abstract
Background
We hypothesized that simulator-generated metrics and intraoperative errors may be able to differentiate the technical differences between hand-assisted laparoscopic (HAL) and straight laparoscopic (SL) approaches.
Methods
Thirty-eight trainees performed two laparoscopic sigmoid colectomies on an augmented reality simulator, randomly starting by a SL (n = 19) or HAL (n = 19) approach. Both approaches were compared according to simulator-generated metrics, and intraoperative errors were collected by faculty.
Results
Sixty-four percent of surgeons were experienced (>50 procedures) with open colon surgery. Fifty-five percent and 69% of surgeons were inexperienced (<10 procedures) with SL and HAL colon surgery, respectively. Time (P < 0.001), path length (P < 0.001), and smoothness (P < 0.001) were lower with the HAL approach. Operative times for sigmoid and splenic flexure mobilization and for the colorectal anastomosis were significantly shorter with the HAL approach. Time to control the vascular pedicle was similar between both approaches. Error rates were similar between both approaches. Operative time, path length, and smoothness correlated directly with the error rate for the HAL approach. In contrast, error rate inversely correlated with the operative time for the SL approach.
Conclusions
A HAL approach for sigmoid colectomy accelerated colonic mobilization and anastomosis. The difference in correlation between both laparoscopic approaches and error rates suggests the need for different skills to perform the HAL and the SL sigmoid colectomy. These findings may explain the preference of some surgeons for a HAL approach early in the learning of laparoscopic colorectal surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic colorectal surgery is feasible, oncologically safe, and improves short-term outcomes compared with open surgery [1–4]. Nonetheless, several studies have demonstrated that laparoscopic colectomy requires significantly longer operative time than open surgery [1, 2]. This last observation reflects the technical complexity of the laparoscopic approach, characterized by loss of three-dimensional view and tactile feedback, a diverting visual/motor axis, a fulcrum effect, and a reduced degree of freedom, contributing to a steep early learning curve to acquire laparoscopic colorectal surgery skills.
The hand-assisted laparoscopic (HAL) approach has been suggested as an introductory approach capable of allowing a transition to straight laparoscopic learning [5–7]. The HAL approach is believed to facilitate the colon dissection by conserving the sense of touch, albeit losing the three-dimensional view. HAL colectomy may be faster than straight laparoscopic (SL) colectomy and has many of the same postoperative advantages as SL colectomy compared with open surgery [8, 9]. Nonetheless, the HAL colectomy has never been shown to be an efficient introductory approach to SL colectomy, indicating that HAL approach may be a destination rather than an initial training technique. In fact, Champagne et al., in a prospective study assessing the completion rate of laparoscopic colectomies performed by a resident, suggested that HAL might be more difficult than SL to initiate residents into laparoscopic colon surgery [10]. No studies have compared the assimilation step-by-step of these two approaches in laparoscopic colorectal surgery. We hypothesized that the simulator-generated metrics and intraoperative errors may be able to distinguish their technical differences for sigmoid colectomy.
Thus, the goal of this prospective observational study was to compare step-by-step HAL and SL sigmoid colectomy techniques on an augmented reality simulator by assessment of simulator-generated metrics and the trainees’ intraoperative errors.
Materials and methods
Protocol
The study took place during two laparoscopic training courses at two international colorectal surgery meetings in 2009–2010. All 38 surgeons enrolled in the courses agreed to participate in the study. Trainees performed both SL and HAL sigmoid colectomies on an augmented reality simulator (ProMIS 2.5, Haptica, Dublin, Ireland). At the start of the course, trainees received instruction about both procedures and the training model from faculty, who were all experienced with this training model. Trainees were randomly distributed to begin by the SL (n = 19) or the HAL (n = 19) approach. Performance was compared between both approaches. The Institutional Review Board of University Hospitals Case Medical Center (Cleveland, OH, USA) approved this study.
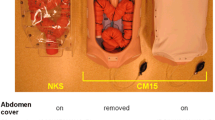
Simulation
The ProMIS simulator is composed of a real scaled plastic manikin linked to a laptop computer (http://www.haptica.com). Inside, an anatomical tray, composed of disposable and reusable plastic components, replicated the peritoneal cavity and the different anatomical planes. Trainees used real surgical instruments on this physical model, providing them with tactile feedback. The laparoscopic sigmoid colectomy technique was standardized for both approaches as follows: access device insertion; medial peritoneal incision; medial to lateral dissection of the Toldt’s fascia; proximal ligation (clips or stapler) of the inferior mesenteric artery; lateral peritoneal incision with mobilization of the spleen flexure; intraperitoneal rectal transection (linear stapler); extraction of the sigmoid specimen; and intraperitoneal colorectal anastomosis (circular stapler). The laparoscopic sigmoid colectomy procedure was performed in eight steps for both approaches as follows: inferior mesenteric artery (1) and left ureter (2) identifications; transection of the inferior mesenteric artery (3); sigmoid (4), descending colon (5), and splenic flexure (6) mobilizations; colorectal anastomosis (7); and peritoneal irrigation (8). Trainees used real instruments, such as access devices, scissors, graspers, staplers, energy devices, and suction. A 0° laparoscope was held by an assistant to perform the SL procedures. HAL procedures were performed without an assistant, using cameras that were incorporated into the body of the simulator.
Assessment criteria
Before the training, trainee experience in colorectal surgery was collected using standardized forms. During the training, the simulator recorded each procedural step for both approaches, automatically and in real time, the operative time (s), the distance covered (path length, mm), and velocity changes over the time (smoothness, jerk cm/s3; a lower smoothness for a better performance) of each instrument tip, and of the assisting hand for the HAL approach (the mid part of the hand was tracked thanks to a specific glove). Right and left hand instrument data for the SL approach, and left hand instrument and right assisting hand data were pooled respectively for the SL and the HAL approach. After completion of each procedure, each anatomical tray of the simulator was examined in standardized fashion by an experienced colorectal surgeon (FL, CPD, or PCN), who step-by-step collected the intraoperative errors using a standardized 14-point checklist [11].
Data analysis
Data were prospectively collected and recorded in Excel® (Microsoft, Redmond, WA). Results were expressed as mean ± SD. Analysis was performed with SPSS® software statistical package (SPSS, Chicago, IL). Metrics and error rates were compared with the paired Student’s t test. Distribution of errors was compared with the χ2 test. A correlation between the error rate and the metrics, and the open surgery experience was researched with the Pearson test. P < 0.05 was considered as significant.
Results
Participants
Twenty-nine practicing surgeons (20 colorectal surgeons, nine general surgeons) and 9 surgeons undergoing training (five fellows, four residents) composed the training group. Sixty-four percent of trainees were experienced (>50 procedures) in open colon surgery, whereas 55 and 69% of them were inexperienced (<10 procedures) in SL and HAL laparoscopic colon surgery respectively (Table 1).
Simulation metrics
SL sigmoid colectomies were performed with a mean operative time, path length, and smoothness of 2,473 ± 693 s, 30,905 ± 1,697 mm, and 1,709 ± 820 jerk cm/s3, respectively. HAL sigmoid colectomies were performed with a mean operative time, path length, and smoothness of 1,603 ± 592 s, 9,262 ± 7,822 mm, and 649 ± 376 jerk cm/s3, respectively. Time (P < 0.001), path length (P < 0.001), and smoothness (P < 0.001) were lower with the HAL than with the SL approach. The mean reduction of time, path length, and smoothness were 36, 70, and 62%, respectively, for the HAL approach compared with the SL approach.
In the step-by-step analysis, the operative times of the sigmoid and splenic flexure mobilizations (steps 4 and 6) and of the colorectal anastomosis (step 7) were significantly shorter with the HAL than with the SL approach (Fig. 1). The HAL time savings were 42, 39, and 44% for steps 4, 6, and 7, respectively. The time to divide the inferior mesenteric artery (step 3) was similar between both approaches. The path length of instruments was significantly shorter for the steps 1–7 with the HAL approach, with a maximal saving for the steps 4, 6, and 7 (Table 2). The smoothness was significantly lower for the steps 1–7 with the HAL approach, with a maximal saving for steps 4, 6, and 7 (Table 2).
Hand-assisted versus straight laparoscopic sigmoid colectomy on augmented reality simulator: stepwise comparison of the operative times. Procedural steps: inferior mesenteric artery (1) and left ureter mobilization (2), vascular transection (3), sigmoid (4) and descending colon (5) and splenic flexure (6) mobilization, colorectal anastomosis (7), and peritoneal irrigation (8). Paired Student’s t test
Intraoperative errors
The mean intraoperative error rate by surgeon was similar between both approaches (SL: 3.8 ± 1.7 vs. HAL: 4.0 ± 2.2; P = 0 .867). Distribution of error types were similar between both approaches (P = 0.799; Table 3). The most frequent error was an incomplete lateral mobilization of the left colon for both approaches. With the HAL approach, the error rate significantly correlated with operative time, path length, and smoothness, and tended to inversely correlate with open experience without reaching significance (Table 4). In contrast, operative time was inversely correlated with the number of errors with the SL approach (Table 4).
Discussion
This is the first study to compare simulator-based step-by-step SL and HAL approaches in colorectal surgery. Simulated sigmoid colectomy was performed faster with the HAL approach with the major advantage in the steps of colonic mobilization and colorectal anastomosis. These data suggest that HAL colectomy shares similar skills with open colectomy. Nonetheless, intraoperative errors were not different between both approaches, further suggesting that the addition of laparoscopic guidance requires additional skills even with the HAL approach. The HAL metrics correlated with the number of intraoperative errors. In contrast, the SL operative time was inversely correlated with the number of errors.
The ProMIS simulator offers the opportunity to operate on a physical tray with real surgical instruments, providing a realistic tactile feedback. With this training simulator, the metrics and the checklist of intraoperative errors have already demonstrated their validity to measure the instrument usage efficiency and assess the laparoscopic surgery experience for basic tasks and colectomy [11–13].
These findings suggest that the techniques actually rely upon different skills for instrument guidance, with HAL relying on visual and tactile cues and SL relying exclusively upon visual cues. The application of tactile skills may be more familiar to surgeons with more open surgical experience; however, such experience was not associated with lower error rates in this study. At the present time, two publications have reported SL sigmoid colectomy metrics with the ProMIS training simulator. Essani et al. reported operating times step-by-step from eight residents [14]. Mean operative time of steps 4, 6, and 7 were 720, 630, and 390 s respectively and were strongly different than our findings. However, operative times were not recorded by the simulator and of the exact procedural steps were not identical compared with our study, allowing limited comparability. Neary et al. [11] compared the metrics between three expert and 11 novice senior surgeons and reported significant differences between the cohorts (mean operative time: 1,704 vs. 3,078 s, P < 0.01; path length: 58,550 vs. 110,050 mm, P < 0.02; smoothness: 2,366 vs. 4,534 jerk cm/s3, P < 0.01). Time and smoothness were in accordance with our findings, whereas path length appeared moderately lower in our study. Nonetheless, these authors did not report the metrics step-by-step for comparison, which has been a limitation of data analysis on simulators for laparoscopic colorectal surgery.
In this study, the operative time was significantly shorter with the HAL approach, with a time saving of 36%, compared with the SL approach. This reduction was limited to colonic mobilization and anastomosis times, and not for vascular control. In a multicenter, randomized trial comparing 33 HAL with 33 SL approaches, Marcello et al. reported a significantly shorter operative time for sigmoid and left colectomy (175 ± 58 vs. 208 ± 55; P = 0.021) [8]. In their study, the mean time saving of 33 min (16%) was lower than noted in the current study. Our data suggest good reproducibility and reliability of the simulator for both HAL and SL approaches. However, the operative time may not be similar between the simulator and clinical practice due to less anatomical complexity as previously suggested with the ProMIS simulator [15].
The intraoperative error rate was similar between both approaches in this study, and is in accordance with clinical practice [5, 8]. The relatively high rate of errors in this study may be explained first by the relative participants’ inexperience in laparoscopic colonic surgery, but also by a less realistic replication than the human cadaver model of tissue consistency and anatomic planes as suggested in a previous study [16]. Importantly, error rate significantly correlated with all three metrics for HAL. Moreover, the error rate tended to correlate inversely with the open experience for HAL. The surgeons in the study group tended to have significant experience in open colon surgery and relative inexperience in laparoscopic colon surgery. These data suggest that HAL performance may rely upon existing open skills related to a combination of tactile and visual guidance of instrumentation. Ozturk et al. assessed operative time and conversion rate of eight HAL total colectomies performed by two senior surgeons (group A), with the first eight SL- (group B) and the last eight SL-total colectomies (group C) performed by three other senior surgeons [8]. These novice laparoscopic colorectal surgeons demonstrated similar conversion rates in groups A and C, both of which were lower than in group B, suggesting better abilities to perform HAL than SL colectomy for senior surgeons in their early learning curve. In contrast, the error rate inversely correlated with the operative time, but not with the movements of instruments for the SL approach. This finding may be explained by specific skills required for the SL approach, which may be significantly more reliant upon visual cue assessment and guidance of operative steps, and which seems to be affected by age, experience, gender, or hand dominance [17]. Champagne et al. suggested a similar hypothesis with the comparison of a single resident’s procedure completion rate for 37 SL and 44 HAL left colectomies [10]. The completion rate (88 vs. 72%; P = 0.06) and operative time (133 vs. 142 min; P = 0.04) were both superior with the SL approach, suggesting a different SL learning curve for surgeons less experienced in open surgery. These data and the current study suggest that SL and HAL surgery rely upon different skills. These data could account for the absence of evidence that HAL surgery provides a platform to migrate to SL colectomy. It also suggests that residents who already have strong SL experience may be able to be taught SL colectomy directly.
In conclusion, the ProMIS simulator appeared to be a reliable model to accurately compare both laparoscopic approaches in terms of operative time and intraoperative errors. The data suggest that the HAL approach for sigmoid colectomy is associated with a reduction of operative time for the colonic mobilization and anastomosis steps, without a difference in intraoperative errors. Conversely, SL demonstrated correlation between errors and operating speed. These findings also suggest that HAL colectomy performance may be more influenced by open surgery experience and skills, whereas the SL approach seems to require different skills and visual pattern recognition. Therefore, although the HAL approach may be useful for senior surgeons, it is unclear that HAL mastery provides skills that will allow junior surgeons to transition easily to SL colectomy.
References
Transatlantic Laparoscopically Assisted vs Open Colectomy Trials Study Group (2007) Laparoscopically assisted vs. open colectomy for colon cancer: a meta-analysis. Arch Surg 142:298–303
Clinical Outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopically-assisted and open surgery for colon cancer. N Engl J Med 350:2050–2059
Laurent C, Leblanc F, Wütrich P et al (2009) Laparoscopic versus open surgery for rectal cancer: long term oncologic results. Ann Surg 250:54–61
Laurent C, Leblanc F, Bretagnol F et al (2008) Long-term wound advantages of the laparoscopic approach in rectal cancer. Br J Surg 95:903–908
Ozturk E, Kiran PR, Remzi F et al (2009) Hand-assisted laparoscopic surgery may be a useful tool for surgeons early in the learning curve performing total abdominal colectomy. Colorectal Dis 12:199–205
Agha A, Moser C, Iesalnieks I et al (2008) Combination of hand-assisted and laparoscopic proctocolectomy (HALP): technical aspects, learning curve and early postoperative results. Surg Endosc 22:1527–1552
Takakura Y, Okajima M, Yoshimitsu M et al (2009) Hybrid hand-assisted colectomy for transverse colon cancer: a useful technique for non-expert laparoscopic surgeons. World J Surg 33:2683–2687
Marcello PW, Fleshman JW, Milsom JW et al (2008) Hand-assisted laparoscopic vs. laparoscopic colorectal surgery: a multicenter, prospective, randomized trial. Dis Colon Rectum 51:818–826
Aalbers AG, Biere SS, van Berge Henegouwen MI et al (2008) Hand-assisted or laparoscopic-assisted approach in colorectal surgery: a systematic review and meta-analysis. Surg Endosc 22:1769–1780
Champagne BJ, Lee EC, Valerian B et al (2008) A novel end point to assess a resident’s ability to perform hand-assisted versus straight laparoscopy for left colectomy: is there really a difference? J Am Coll Surg 207:554–559
Neary PC, Boyle E, Delaney CP et al (2008) Construct validation of a novel hybrid virtual-reality simulator for training and assessing laparoscopic colectomy; results from the first course for experienced senior laparoscopic surgeons. Surg Endosc 22:2301–2309
Oostema JA, Abdel MP, Gould JC (2008) Time-efficient laparoscopic skills assessment using an augmented-reality simulator. Surg Endosc 22:2621–2624
Ritter EM, Kindelan TW, Michael C et al (2007) Concurrent validity of augmented reality metrics applied to the fundamentals of laparoscopic surgery (FLS). Surg Endosc 21:1441–1445
Essani R, Scriven RJ, McLarty AJ et al (2009) Simulated laparoscopic sigmoidectomy training: responsiveness of surgery residents. Dis Colon Rectum 52:1956–1961
Leblanc F, Delaney CP, Neary PC et al (2010) Assessment of comparative skills between hand-assisted and straight laparoscopic training on an augmented reality simulator. Dis Colon Rectum 53(9):1323–1327
Leblanc F, Champagne BJ, Augestad KM et al (2010) A comparison of human cadaver and augmented reality simulator models for straight laparoscopic colorectal skills acquisition training. J Am Coll Surg 211(2):250–255
Grantcharov TP, Bardram L, Funch-Jensen P et al (2003) Impact of hand dominance, gender, and experience with computer games on performance in virtual reality laparoscopy. Surg Endosc 17:1082–1085
Acknowledgments
This work was supported by an unrestricted grant from Ethicon EndoSurgery.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leblanc, F., Delaney, C.P., Ellis, C.N. et al. Hand-Assisted Versus Straight Laparoscopic Sigmoid Colectomy on a Training Simulator: What is the Difference?. World J Surg 34, 2909–2914 (2010). https://doi.org/10.1007/s00268-010-0765-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-010-0765-0