Abstract
Background
The aim of this study was to ascertain the outcome of liver transplantation (LT) due to hepatocellular carcinoma (HCC) in patients who had undergone previous liver resection (LR) for HCC.
Methods
A case-control study (1:2) was designed to compare patients who underwent LT due to HCC recurrence with a previous LR for HCC (study group) with those who underwent LT for primary HCC but without previous LR (control group).
Results
From January 1990 to December 2007, a total of 303 cirrhotic patients with primary HCC were evaluated for surgery. Primary LT was performed in 191 and LR in 100. When HCC recurrence was diagnosed after LR (69/100), 17 of the 69 (25%) patients underwent LT (study group). The median follow-up was 70 months (12.7–203.0 months). Disease-free survivals at 1, 3, and 5 years in the study group versus the control group were 86%, 68%, 58% vs. 97%, 93%, 89%, respectively (p < 0.04). The 1-, 3-, and 5-year actuarial patient survivals in the study group versus the control group were 59%, 52%, 52% vs. 85%, 76%, 65%, respectively (p = NS). Patients of the study group were divided into two groups according to the time to recurrence after LR: group 1 was <1 year, and group 2 was >1 year. Recurrence after LT was 75% in group 1 vs. 15.4% in group 2 (p < 0.03). The 1-, 3-, and 5-year actuarial patient survivals were 25%, 0%, 0% in group 1 and 69%, 69%, 69% in group 2, p < 0.02).
Conclusions
Liver transplantation can be safely performed after a previous LR for HCC. Patients with recurrence during the first year after hepatectomy have a poor prognosis after LT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Partial liver resection (LR) is a safe, effective treatment for early hepatocellular carcinoma (HCC) in patients with nondecompensated cirrhosis [1, 2]. However, there is a new tumor or recurrence in a high percentage of patients due to various factors, such as liver cirrhosis persistence [3].
Treatment of recurrence includes the use of antineoplasic drugs, locoregional therapies (radiofrequency, chemoembolization, alcoholization), re-resection, and liver transplantation (LT). The advantage of LT as a treatment for HCC recurrence over other treatments is its efficacy in treating HCC with total hepatectomy, removing underlying cirrhotic tissue and restoring normal liver function [4]. However, owing to organ shortage and other medical reasons, LT cannot always be applied; consequently, liver grafts must be optimized and LT performed only in selected cases [5]. Thus, careful selection of patients who may benefit from LT and identifying those whose risk of recurrence is as low as possible must be done preoperatively. Results regarding LT outcome in patients who underwent LT because of HCC and who have undergone partial LR for a previous tumor are controversial [6, 7].
The aim of our study was to ascertain the outcome of patients with LT due to HCC who had undergone partial LR for a previous tumor compared with that of patients who underwent LT for a primary HCC. We also wanted to determine if there is a group of patients in whom LT would be contraindicated after LR.
Materials and methods
Study design
The study group comprised cirrhotic patients who underwent LT for HCC recurrence who had undergone previous LR for HCC. A case-control (1:2) study was designed to compare these patients with those who underwent LT for primary HCC without previous LR (control group). Patients in the control group had undergone transplantation before and after each patient in the study group and with the same cirrhosis origin.
Preoperative evaluation
Written informed consent was obtained from all patients prior to surgery or to inclusion on the waiting list for LT.
Imaging study
Ultrasonography (US) was used as the first diagnostic approach for early detection of HCC in our surveillance program. HCC was diagnosed by US and abdominal computed tomography (CT) or abdominal nuclear magnetic resonance (MRI) of the abdomen. Extrahepatic tumoral spread was evaluated by abdominal and chest CT and bone scintigraphy. Since the publication of the AASLD Practice Guideline of Management of Hepatocellular Carcinoma, the diagnosis of HCC has been based on this guideline [8]. US-guided percutaneous needle liver biopsy of the liver nodule was performed when the diagnosis was not confirmed by two imaging studies.
Liver function tests and portal hypertension
Liver function was evaluated with liver function tests, and patients were classified according to the Child-Pugh classification. Significant portal hypertension was defined as a portosystemic gradient >10 mmHg. The presence of esophageal varices, splenomegaly, and/or a platelet count <100,000 were also accepted for diagnosis. An α-fetoprotein (AFP) value ≥100 ng/ml was also used as an aid to diagnosis [9].
Liver resection criteria and surgical techniques
Criteria for LR changed over the study period (before 1999 patients who underwent LR were mostly those with a single tumor and preserved liver function). Basically, candidates for surgery were patients with good general status and a feasible, complete, safe resection (Child-Pugh A or B) of the liver tumor, with no extrahepatic disease. Patients have been treated according to the HCC management guideline since its publication [8].
The surgical techniques and postoperative treatment were described previously by our group [10]. Intraoperative US examination was performed on all occasions to rule out other foci of HCC and to perform radical surgery with safe margins. Minor hepatectomy was defined as LR of fewer than three liver segments and major hepatectomy as three or more liver segments [10].
Liver transplantation criteria
Criteria for LT also changed during the study period (before 1996 candidates for LT were mostly those with fewer than three tumors and the tumors being <5 cm). Cirrhotic patients were considered for LT who were <70 years of age, had no contraindications for major surgery, and had a single unresectable central tumor or other tumors in patients with significant portal hypertension or bilirubin >1 mg/dl. During the early years of the study period, patients with large HCCs or with more nodules were selected to undergo transplantation. Since the Milan criteria were established, however, only patients fulfilling these criteria have been included on the waiting list for LT [11].
High pathologic risk of recurrence after liver transplantation
Patients with HCC who presented with microvascular invasion and/or satellitosis on pathologic study after LT or LR for HCC were considered to have a high pathologic risk of recurrence [12].
Treatment of HCC recurrence
Patient follow-up after LR included US and AFP every 3 months during the first year and every 6 months after the first year. A new complete evaluation was undertaken to detect extrahepatic metastases when liver HCC recurrence was diagnosed. Treatment of recurrence was repeat liver resection when technically feasible and the patient had nondecompensated cirrhosis, normal bilirubin, and no portal hypertension. In cases of decompensated cirrhosis or abnormal bilirubin and significant portal hypertension, LT was indicated if the patient’s age and HCC characteristics permitted such a procedure. In the remaining cases, ablative techniques such as radiofrequency thermal ablation (RFA) and transarterial chemoembolization (TACE) were applied. When HCC recurrence was systemic, other palliative treatments were administered.
Postoperative morbidity and mortality
Morbidity and mortality were considered as those incidents occurring during the postoperative hospital stay prior to discharge or within the first 30 days after surgery.
Statistical analysis
Data were expressed as the mean ± SD and median (range) when an abnormal distribution of data was identified. A nonparametric test was used (Mann-Whitney U-test) for numeric variables; and the chi-squared test with Fisher’s correction for categoric variables was used to compare the groups. Patient survival rates were estimated using the Kaplan-Meier method and compared by the long-rank test. p < 0.05 was considered statistically significant. Statistical analyses were performed with SPSS 15.0 softward (SPSS, Chicago, IL, USA).
All data were prospectively collected and retrospectively analyzed. Median follow-up was 70 months (12.7–203.0 months).
Results
Patient population
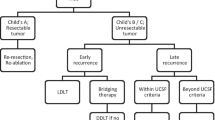
From January 1990 to December 2007, a total of 303 cirrhotic patients with primary HCCs were evaluated for surgical treatment at our department. Of these patients, 203 were included on the waiting list for LT. During follow-up, 11 patients dropped out and 1 remains on the waiting list; ultimately, 191 underwent LT for primary HCC (Fig. 1). In all, 100 patients underwent LR. When HCC recurrence was observed in the LR group (69/100), only 17 of the 69 patients (25%) could be treated by LT (study group). The other 52 patients were not eligible for LT at the time of HCC recurrence, of whom 30 had oncologic reasons (15 had out of Milan local recurrence and 15 extrahepatic disease) (Fig. 1).
Characteristics of the study group versus HCC recurrence in the patients noneligible for liver transplantation group
At the time of LR, the characteristics of the 17 patients who underwent LT due to HCC recurrence (study group) are summarized in Table 1. No differences were observed between the study group and the group of patients with HCC recurrence after LR who could not undergo transplantation for oncologic reasons (Table 2).
Liver transplantation for HCC recurrence in patients with previous liver resection (study group) versus the control group
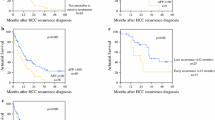
No differences were found between the study group and the control group except for preoperative portal hypertension (Table 3). Although no significant differences were found regarding HCC recurrence and mortality after LT between groups, the recurrence rate in patients in the study group was twice as high (Table 3). No differences were found regarding actuarial survival between groups, although better disease-free survival was observed in patients of the control group (Fig. 2).
Survival according to time to recurrence after liver resection
Patients of the study group were divided into two groups according to the time to recurrence after the partial LR. The first group comprised 4 patients whose recurrence post-LR occurred during the first year of follow-up (<12 months). The other 13 patients formed the second group, whose recurrence was diagnosed after the first year (>12 months). Characteristics of the two groups are shown in Table 4. Patients with a recurrence during the first year had significantly poorer tumor cell differentiation than patients with recurrences after the first year. Although no significant differences were found, patients in the first group had three times more pathologic risk of recurrence at the time of LR. After LT, recurrence was higher in the first group than in the second group (75% vs. 15.4%, respectively, p < 0.03) (Table 4). Moreover, actuarial 1-, 3-, and 5-year patient survivals were better in the second group (25%, 0%, 0% vs. 69%, 69%, 69%; p < 0.02) (Fig. 3).
Patients of the study group recurring after the first year (n = 13) versus control group
No differences were found according to HCC recurrence and disease-free survival when patients of the study group were compared with the control group once patients with recurrence during the first year had been excluded from the study group. HCC recurrence was 15.4% for patients with recurrence after 1 year vs. 12% for the control group; and the 1-, 3-, and 5-year disease-free survivals were 100%, 88%, and 75% for patients with recurrence after 1 year vs. 97%, 93%, and 89% for the control group.
Discussion
Over the last decade, improvement in patient selection for LR, surgical skills, and postoperative period management, together with organ shortage, have led to an increase in the applicability of this treatment [13]. It is well known that 5-year survival rates after LR are at least 50% [14] with a high recurrence rate (up to 70%) [3]. At the time of HCC recurrence, the treatment we can offer our patients depends on various factors, such as age, size of the largest nodule, number of nodules, tumor location in the liver, and cirrhosis status, as well as the presence of extrahepatic recurrence. Poon et al. reported that almost 80% of patients with recurrence after a primary LR for HCC remain eligible for LT [15].
Our study focused on a group of patients who had undergone LR for HCC and, at the time of recurrence, were given a transplant. LT in patients with HCC is clearly limited by organ shortage worldwide. Various strategies, such as performing LR in patients with HCC who are eligible for LT, have been proposed in an attempt to cure these patients [16]. One consists of LR and “salvage” LT at the time of HCC recurrence; however contradictory results have been reported [6, 7]. Patients from the series of Belghiti et al. were favorable regarding HCC recurrence risk, and in some of those patients LT was not indicated for HCC recurrence [7]. On other hand, Adam et al. noted that the indication for LT was HCC recurrence in all patients [6]. Probably it is these and other differences between the cohorts that render the results so contradictory. The problem with this strategy and its applicability lies, first, in the type of HCC recurrence: advanced intrahepatic disease and extrahepatic recurrence are contraindications to transplantation. Moreover, it is not clear which patients, who are eligible for LT at the time of recurrence, will benefit from LT.
In our study group, LR was performed for primary HCC mainly in patients with a single tumor and no significant portal hypertension. However, some patients exceeded these criteria as our patient population belonged to a historical cohort of patients, some of whom had undergone LR before the Barcelona Clinic Liver Cancer (BCLC) staging classification and guidelines for HCC management were reported [8, 17]. The tumor size of a solitary nodule has not been reported as a clear-cut limiting factor for LR [8, 18]. Despite the risk of vascular invasion and satellitosis increasing with size [19, 20], some single tumors may grow as a large mass with no evidence of vascular invasion [8]. Most of our resections were minor hepatectomies with complete excision of the tumor in all cases; and even though our morbidity rate was high compared with other studies [21], our outcome was successful with nil mortality or liver failure. In our series, we found a low rate (25%) of patients who could have transplantation after HCC recurrence. Most of the patients had extrahepatic HCC recurrence or a local recurrence that exceeded the Milan criteria even though there were no significant differences in HCC pathology between the LR and study groups. These findings are probably explained by intrinsic tumor aggressiveness [22–25].
As previously reported, LT in patients with previous LR for HCC is technically feasible [7, 15]. This fact was confirmed in our case-control study as no differences were found regarding operating time, intraoperative transfusion, or postoperative morbidity and mortality. On the other hand, although both preoperative and pathologic findings of the tumor were similar in both groups, the recurrence rate and disease-free survival were better in the control group. Although vascular invasion and satellitosis are accepted worldwide as the best predictors of tumor recurrence [25, 26], the impact of these findings in patients fulfilling Milan criteria in the liver transplantation setting may not be as significant. As reported in the Adam et al. study and confirmed by our group, patients with a previous LR for HCC have an increased risk of recurrence and poorer disease-free survival [6]. One differential finding between the study and control groups was that the time from diagnosis of the first HCC to LT was clearly longer in the study group. Probably these patients had been exposed to tumor cells for a longer period of time, which would explain the higher recurrence rate.
One of the most salient results of our study was that patient survival post-LT in the study group differed depending on the time of HCC recurrence after LR. No patient in whom HCC recurrence was diagnosed during the first year of follow-up after LR survived more than 3 years post-LT. Although differences did not reach statistical significance, however, patients with early HCC recurrence after LR had a threefold higher pathologic risk of recurrence when the whole cirrhotic liver was examined at the time of LT. Minagawa et al. [25] reported a 5-year survival of 57% after repeat hepatectomy—but in selected patients who probably would have had a good prognosis regardless of the treatment. Interestingly, they found early recurrence (during the first year of follow-up) after the first hepatectomy to be a risk factor for poor outcome after repeated hepatectomy. In our series, when certain patients—those with early recurrence after LR—were excluded from the study, results were similar to those of the control group. These data strongly reinforce the finding that patients with early HCC recurrence after LR for HCC have poor prognosis after LT.
The fact that the tumor recurs early could be an indicator of advanced disease, with other intrahepatic HCC foci at the time of LR that were not detected with imaging techniques. In any event, early recurrence after LR appears to be a predictive factor of poor outcome when patients are included on the waiting list for LT.
Cillo et al. reported that tumor differentiation represents a direct marker of biologic tumor aggressiveness and that it may provide more accurate information on the risk of recurrence [27–29]. Even among the small number of patients in our series, all patients with recurrence during the first year after LR had poor cellular differentiation at the time of the resection. These findings indicate more aggressiveness of the tumors. Along the same lines, it has been suggested that the histologic grade of the HCC can be determined preoperatively with percutaneous needle biopsy, thus indicating the risk of microvascular invasion [30]. In association with new biohumoral factors that may predict the invasiveness of HCC, histologic grading may estimate the risk of posttransplant recurrence, thereby improving selection criteria [29].
To resolve this problem and reduce HCC recurrence after LT, Sala and colleagues from the BCLC study group proposed including on the LT waiting list all patients with unfavorable histopathologic signs (satellitosis and/or vascular invasion) after LR for HCC as a “prophylactic” LT before a hypothetical recurrence appears [12]. Although a good outcome was reported with this approach, further data are required to validate these results.
We consider LR an acceptable option as a first approach even though when HCC recurrence appeared in our patients who had undergone resection “salvage” LT could be applied in only one-fourth of them. Future biological HCC markers may help us decide which of these patients will benefit directly from LR and which will need a more aggressive treatment such as LT.
The MELD system [31] is currently being applied in most countries, and patients with HCC have a shorter waiting-list time than they had before; however, in some countries, dropout from the waiting list is high [32], and treatment to downstage HCCs that grow during the waiting-list time is applied. LR probably represents the best possible downstaging treatment for HCC. Despite being a more aggressive treatment that can be applied in only a small number of cases, it offers a 25% possibility of cure to our patients.
Conclusions
Liver transplantation can be safely performed in patients who have undergone previous LR for HCC, with outcomes similar to those in patients undergoing primary LT for HCC but with a high recurrence rate. In our study, patients with a disease-free interval between LR and HCC recurrence of <1 year had poor survival after LT. The fact that patients with recurrence during the first year after hepatectomy have such a poor prognosis after transplantation should induce us to consider whether, given the shortage of donors, these patients should indeed be chosen for a transplant, particularly if poor cellular differentiation is present in the tumor. Nevertheless, it should be taken into account that our series included a limited number of patients.
References
Fang ST, Lo CM, Liu CL et al (1999) Hepatectomy for hepatocellular carcinoma: toward zero hospital deaths. Ann Surg 3:322–330
Fong Y, Sun RL, Jarnagin W et al (1999) An analysis of 412 cases of hepatocellular carcinoma at a Western center. Ann Surg 6:790–799
Llovet J, Fuster J, Bruix J (1999) Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Hepatology 6:1434–1440
Fuster J, Charco R, Llovet J et al (2005) Liver transplantation in hepatocellular carcinoma. Transpl Int 3:278–282
Margarit C, Charco R, Hidalgo E et al (2002) Liver transplantation for malignant disease: selection and pattern of recurrence. World J Surg 2:257–263
Adam R, Azoulay D, Castaing D et al (2003) Liver resection as a bridge to transplantation for hepatocellular carcinoma on cirrhosis: a reasonable strategy? Ann Surg 4:508–551
Belghiti J, Cortes A, Abdalla EK et al (2003) Resection prior to liver transplantation for hepatocellular carcinoma. Ann Surg 6:885–892
Bruix J, Sherman M (2005) Practice Guidelines Committee, American Association for the Study of Liver Diseases: management of hepatocellular carcinoma. Hepatology 5:1208–1236
Sherman M (2005) Hepatocellular carcinoma: epidemiology, risk factors, and screening. Semin Liver Dis 2:143–154
Balsells J, Charco R, Lázaro JL et al (1996) Resection of hepatocellular carcinoma in patients with cirrhosis. Br J Surg 6:758–761
Mazzaferro V, Refalia E, Doci R et al (1996) Liver transplantation for the treatment of small hepatocellular carcinoma in patients with cirrhosis. N Engl J Med 11:693–699
Sala M, Fuster J, Llovet J et al (2004) High pathological risk of recurrence after surgical resection for hepatocellular carcinoma: an indication for salvage liver transplantation. Liver Transpl 10:1294–1300
Llovet J, Bruix J (2008) Novel advancements in the management of hepatocellular carcinoma in 2008. J Hepatol 48(Suppl 1):S20–S37
Llovet J, Schwartz M, Mazzaferro V (2005) Resection and liver transplantation for hepatocellular carcinoma. Semin Liver Dis 2:181–200
Poon RT, Fan ST, Lo CM et al (2002) Long-term survival and pattern of recurrence after resection of small hepatocellular carcinoma in patients with preserved liver function: implications for a strategy of salvage transplantation. Ann Surg 3:373–382
Margarit C, Escartin A, Castells L et al (2005) Resection for hepatocellular carcinoma is a good option in Child-Turcotte-Pugh class A patients with cirrhosis who are eligible for liver transplantation. Liver Transpl 10:1242–1251
Llovet J, Brú C, Bruix J (1999) Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis 3:329–338
Ng KK, Vauthey JN, Pawlik TM et al (2005) Is the resection for large or multinodular hepatocellular carcinoma justified? Results from a multi-institutional database. Ann Surg Oncol 5:364–373
Nakashima Y, Nakashima O, Tanaka et al (2003) Portal vein invasion and intrahepatic micrometastasis in small hepatocellular carcinoma by gross type. Hepatol Res 2:142–147
Ikai I, Arii S, Kojiro M et al (2004) Reevaluation of prognostic factors for survival after liver resection in patients with hepatocellular carcinoma in a Japanese nationwide survey. Cancer 4:796–802
Makuuchi M, Donadon M, Torzilli G (2008) Hepatic resection for hepatocellular carcinoma in cirrhosis. Ann Ital Chir 2:111–115
Farazi PA, DePinho RA (2006) Hepatocellular carcinoma pathogenesis: from genes to environment. Nat Rev Cancer 6:674–687
Zucman-Rossi J, Jeannot E, Nhieu JT et al (2006) Genotype-phenotype correlation in hepatocellular adenoma: new classification and relationship with HCC. Hepatology 3:515–524
Hoshida Y, Villanueva A, Kobayashi M et al (2008) Gene expression in fixed tissues and outcome in hepatocellular carcinoma. N Engl J Med 19:1995–2004
Minagawa M, Makuuchi M, Takayama T et al (2003) Selection criteria for repeat hepatectomy in patients with recurrent hepatocellular carcinoma. Ann Surg 5:703–710
Imamura H, Matsuyama Y, Tanaka E et al (2003) Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol 2:237–249
Klintmalm GB (1998) Liver transplantation for hepatocellular carcinoma: a registry report of the impact of the tumor characteristics on outcome. Ann Surg 4:479–490
Tamura S, Kato T, Berho M et al (2001) Impact of histological grade of hepatocellular carcinoma on the outcome of liver transplantation. Arch Surg 1:25–30
Cillo U, Vitale A, Bassanello M et al (2004) Liver transplantation for the treatment of moderately or well-differentiated hepatocellular carcinoma. Ann Surg 2:150–159
Jonas S, Bechstein WO, Steinmuller T et al (2001) Vascular invasion and histopathological grading determine outcome after liver transplantation for hepatocellular carcinoma in cirrhosis. Hepatology 5:1080–1086
Wiesner RH, Freeman RB, Mulligan DC (2004) Liver transplantation for hepatocellular cancer: the impact of the MELD allocation policy. Gastroenterology 127(Suppl 1):S261–S267
Schwartz M, Roayaie S, Uva P (2007) Treatment of HCC in patients awaiting liver transplantation. Am J Transplant 8:1875–1881
Acknowledgments
Carlos Margarit, MD, PhD, as the Director of the Liver Transplant Unit from 1988–2005. Miss Christine O’Hara is thanked for valuable revision of the English version of the article. Esther Delgado is also thanked.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sapisochin, G., Bilbao, I., Balsells, J. et al. Optimization of Liver Transplantation as a Treatment of Intrahepatic Hepatocellular Carcinoma Recurrence After Partial Liver Resection: Experience of a Single European Series. World J Surg 34, 2146–2154 (2010). https://doi.org/10.1007/s00268-010-0583-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-010-0583-4